The Role of Acute Phase Proteins in Induction of Tension of Nonspecific Resistance System in Various Clinical Phenotypes of Myasthenia
Received: 09-Nov-2016 / Accepted Date: 29-Nov-2016 / Published Date: 02-Dec-2016 DOI: 10.4172/2161-0681.1000300
Abstract
Introduction: All over the world autoimmune diseases and one of the classic examples of such diseases - myasthenia gravis - are on the rise. This progressing autoimmune disease characterized by pathological muscle weakness and increased fatigue. The literature describes the cause of myasthenia as production of autoantibodies to acetylcholine receptor subunits thereof. However myasthenia inherent immunological phenomena are not described in the literature, except the concentration of interleukins. Methods: All the 69 patients were examined and divided into 3 groups depending on the morphological damage of the thymus: a group of "myasthenia without morphological damage of the thymus" represented by 30 patients, a group of "myasthenia with hyperplasia of the thymus" represented 23 patients, a group of "myasthenia with thymoma" represented by 16 patients. We used these laboratory methods: microscopic determining phagocytic activity of granulocytic neutrophils; studying oxygen-dependent metabolism of neutrophil granulocytes (NBT-test); determining of C-reactive protein in blood serum; photometric determination of haptoglobin content (with rivanol); photometric determination of ceruloplasmin content by Ravin; nephelometric determination of concentration of C3 component of the complement.
Keywords: Autoimmune; Myasthenia; Metabolism; Acute phase proteins; Phagocytosis; NBTtest; C3-complement
315299Introduction
All over the world autoimmune diseases are on the rise [1]. One of the classic examples of such diseases is myasthenia gravis-a progressing autoimmune disease characterized by pathological muscle weakness and increased fatigue. It is noted that the cause of myasthenia is dysfunction of neuromuscular transmission [2].
Myasthenia can be found in 5-10 cases per 100,000 people, according to various authors. Timeliness of studying and treating myasthenia is connected to the social factor, namely: the onset of the disease occurs in a young productive age-the debut is up to 90% before the age of 40; it is more common in women-3:1, according to the data of Moscow Myasthenic center [3]; women get ill earlier than men; women’s cases are more severe than men’s.
In our previous publications it was shown that such pathology as myasthenia of various clinical phenotypes is characterized by tension of the system of non-specific resistance of the body [4]. However, the role of proteins of the acute phase in forming the above condition of tension as formations produced by the body at the earliest stages of immune reaction is still unknown, because functional peculiarities of proteins of acute phase allow putting them in the mediators and inhibitors of inflammation.
Proteins of acute phase (C-reactive protein, haptoglobin and ceruloplasmin) in literature are considered to be indicators of metabolic systems as reactants of blood, i.e., groups of plasma proteins, glycoproteins and their components, the concentration of which is increased a lot and non-specifically in reaction to various pathological stimuli [5].
It is very timely to study the influence of proteins of acute phase as prerequisites of the found phenomenon of the system tension of nonspecific resistance in various clinical phenotypes of myasthenia with the purpose of further developing methods of direct immunocorrection.
The objective of this work: to study the influence of proteins of acute phase on the process of phagocytosis in patients with various clinical phenotypes of myasthenia.
The hypothesis of this article is: the role of proteins of the acute phase in forming the condition of tension of the system of non-specific resistance of patients with different clinical phenotypes of myasthenia gravis is essential and requires in-depth study.
Materials And Methods
A total of 69 patients with myasthenia and morphological and functional changes in the thymus-hyperplasia and thymoma have been observed, ages 13-70. All the patients were examined and divided into 3 groups depending on the morphological damage of the thymus: a group of “myasthenia without morphological damage of the thymus” represented by M-30 patients, a group of “myasthenia with hyperplasia of the thymus” represented by MH-23 patients, a group of “myasthenia with thymoma” represented by MT-16 patients, and also a group of 30 healthy volunteers who were a control group.
The following laboratory methods were used:
Method of separating neutrophil granulocytes
Neutrophil granulocytes were separated from leukocytal suspension of blood drawn from the cubital vein. To study the phagocytosis of neutrophil granulocytes, we use 2.5 ml of blood. Of this amount, we get 1.3-1.5 ml of the leukocyte suspension. We allocate 0.2-0.3 ml of neutrophil granulocytes by the density gradient ficoll-verografin. We use 0.2 ml neutrophil granulocytes for studying phagocytosis.
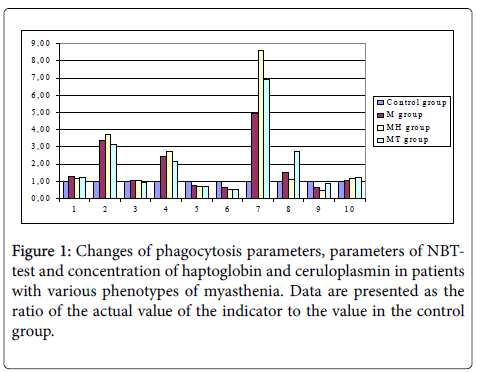
Method of determining phagocytic activity of granulocytic neutrophils
Phagocytic activity of granulocytic neutrophils was determined in leukocytic suspension obtained from heparinized blood. For research, equal amounts of leukocytic suspension (0.2 ml) and washed suspension of Saccharomyces cerevisiae (baking yeast) (0.2 ml) were mixed. The obtained samples were incubated for 60 minutes at 37°C and stirred regularly. After incubation, smears were prepared which were dyed with Romanovsky dye. Microscopic exam was performed under immersion system. The phagocytic index (PI) was calculated as the percentage of cells that joined the phagocytosis of the total number. Phagocytic number (PN) - the average number of yeast cells inside the cell was calculated by dividing the total number of yeast cells absorbed by the number of cells that have entered into phagocytosis. Both specimens (PI and PN) were calculated on smears made after the 30- minute and 90-minute incubation (PI 30, PI 120 and the PN 30, the PN 120). Completeness index of phagocytosis (CIP) was calculated by dividing PN 30 by PN 120 (Figure 1) [6].
1 - Phagocytic Index, Percentage (%);
2 - Percentage of Positive cells in NBT-test spontaneous;
3 - Percentage of Positive cells in NBT-test stimulated;
4 - Average cytochemical coefficient (ACKspont) in NBT-test spontaneous;
5 - Average cytochemical coefficient in (ACKstim) NBT-test stimulated;
6 - Stimulation index;
7 - C-reactive protein, mg/l;
8 - Haptoglobin, g/l;
9 - Ceruloplasmin, mg/l;
10 - C3-fragment of complement, mg/dl.
Method of studying oxygen-dependent metabolism of neutrophil granulocytes (NBT-test)
Oxygen-dependent metabolism of neutrophil granulocytes was studied in reaction of spontaneous and stimulated restoring nitroblue tetrazolium (NBT-test) using A.N. Mayansky’s method. In the course of reaction, NBТ is restored to undissolvable diformazan which is deposited in cells in the kind of dark-blue granules which can be visually detected by microscopic exam [7]. At each stroke 100 neutrophils were counted and the percentage of cells containing diphormazane inclusion in granular form or solid de calculating posits was calculated. Average cytochemical coefficients in spontaneous and stimulated tests (ACKspont, ACKstim) were calculated according to the formula Astaldi-Verg. To do this, the cells are divided into 4 groups according to the number of diphormazane granules: (a) - with no activity (no granules) - 0; (b) - with a slightly positive reaction (single granules) -1+; (c) - with a positive response (coated granules to 50% of the area of the cytoplasm) - 2 ++; (d) - with a strongly positive reaction (more than 50% of the area occupied by cytoplasmic granules) - 3 +++. Calculation was performed as follows: а+в+с+d = 100%, thus, the percentage of positive cells - b+c+d=100%-a%. ACK=(1 × в+2 × с+3 × d)/100. The stimulation index (SI) was calculated as follows:
SI=(Percentage of positive cells in NBT test spontaneous)/ (Percentage of positive cells in NBT test stimulated). NBT-test not only reveals the phagocytic neutrophils, but also characterizes their oxygendependent anti-infective enzyme systems. The intensity of the restoration of nitro blue tetrazolium reflects the production of biological oxidizers with bactericidal action (hydrogen peroxide, superoxide anion oxygen, singlet oxygen). Therefore spontaneus NBTtest is used to evaluate intracellular antibacterial enzyme systems of unactivated neutrophil granulocytes and ACKspont (Average cytochemical coefficient, ACKspont) characterizes the degree of activation of intracellular antibacterial enzyme systems in spontaneous test. Stimulated NBT-test is an informative method of assessment of resistance in the study of immune status, as it characterizes the reserves bactericidal function of neutrophils. Stimulated NBT is used to detect intracellular reserve capacity of phagocytes systems and Average cytochemical coefficient ACKstim characterizes the degree of activation of intracellular antimicrobial enzyme systems in the stimulated test.
Method of determining the content of C-reactive protein in blood serum
It is based on separating protein of acute phase-C-reactive protein in the blood serum. Its presence was determined by agglutination reaction with anti-bodies to C-reactive protein, which was absorbed on neutral latex particles (latex test). The amount was determined by the method of multiple dissolving of blood serum and repeating the agglutination reaction [8]. Diagnostic reagents for the semiquantitative in vitro determination of C-reactive protein in human serum were employed (by GRANUM, Ukraine).
Method of photometric determination of haptoglobin content
The principle of this method: when a solution of hemoglobin is added to blood serum, a haptoglobin-hemoglobin complex is formed which is set by rivanol. The remaining rivanol was determined photometrically by the intensity of coloring on spectrum-photometer SF-46 (LOMO, RF) with the wave length 540 nm [9]. Diagnostic reagents for the quantitative in vitro photometric determination of haptoglobin content in human serum were employed (by REAGENT, Ukraine).
Method of photometric determination of ceruloplasmin content by Ravin
The principle of the method: when p-phenilendiamin is added to ceruloplasmin, a fermentative reaction of oxidation occurs, which is inactivated by sodium fluoride. The content of ceruloplasmin is determined photometrically by the intensity of coloring of the reaction product on spectrum-photometer SF-46 (LOMO, RF) with the wave length 540 nm [10]. Diagnostic reagent for the quantitative in vitro photometric determination of ceruloplasmin in human serum was employed (by REAGENT, Ukraine).
Method of nephelometric determination of concentration of C3 component of the complement
The method is based on the interaction of protein with specific antibodies with forming immunocomplexes, precipitation of which leads to increased suspension materials proportionally to the concentration of C3 component in the sample. The concentration of C3 component of the complement was determined photometrically on biochemical analyzer STAT FAX 1904 (USA) with the wave length 340 nm [11]. Diagnostic reagents for the quantitative in vitro determination of complement C3 in human serum by turbidimetric analysis were employed (by DIALAB, Austria).
Statistical analysis
The results obtained were processed statistically using the Student's t-test, using the software package "STATISTIKA V.6".
Results
During the study of the system of congenital non-specific immunity cell reactions were studied-phagocytic activity of neutrophil granulocytes with detailed study of their enzymatic activity as nonspecific factors of natural resistance in a test with nitro blue tetrazolium (Table 1).
| Indicators of the phagocytic activity of neutrophils | Control group | M group | MH group | MT group |
|---|---|---|---|---|
| Phagocytic index PI(Percentage %) | 65.0 ± 5.1 | 82.70 ± 7.9* | 77.04 ± 8.1* | 81.71± 8.5 * |
| Phagocytic number PN | 3.2 ± 0.2 | 3.33 ± 0.9 | 2.85± 0.6 | 3.51± 0.9 |
| Completeness index of phagocytosis CIP | 1.15 ± 0.12 | 1.12 ± 0.4 | 1.05± 0.2 | 1.04± 0.21 |
Table 1: Phagocytic activity of neutrophil granulocytes in patients with different clinical phenotypes of myasthenia gravis.
Note. *-Significantly of difference from control p ≤ 0.05.
While analyzing the phagocytic activity of neutrophil granulocytes (Table 1), an increased number was found of those of them which were involved in phagocytosis in all clinical phenotypes of myasthenia (the phagocyte index is increased by 20-25% in patients with myasthenia both with and without morphological damage of the thymus). Other indicators of the phagocytic activity of neutrophil granulocytes had not changed so much (Table 1). While studying enzymatic activity of neutrophil granulocytes in a test with nitro blue tetrazolium in all clinical types of myasthenia, an increase by 3-3.5 times of the number of positive, or activated cells in a spontaneous NBT-test was observed (Table 2).
| Indicators of the enzymatic activity of neutrophils | Control group | M group | MH group | MT group |
|---|---|---|---|---|
| Percentage of Positive cells in NBT test spontaneous | 12.0 ± 4.0 | 40.3 ± 5.4* | 44.5 ± 3.5* | 37.5 ± 3.7* |
| Percentage of Positive cells in NBT test stimulated | 60.0 ± 12.0 | 64.9 ± 3.3 | 65.4 ± 3.2 | 58.0 ± 5.9 |
| Average cytochemical coefficient (ACKspont) in NBT test spontaneous | 0.26 ± 0.19 | 0.64 ± 0.06 | 0.71 ± 0.07* | 0.56 ± 0.24 |
| Average cytochemical coefficient in (ACKstim) NBT test stimulated | 1.5 ± 0.3 | 1.15±0.08 | 1.11±0.09 | 1.02±0.89 |
| Stimulation index (SI) | 3.0 ± 1.0 | 1.84±0.16 | 1.59±0.11 | 1.62±0.13 |
Table 2: Enzymatic activity of neutrophil granulocytes in NBT test in patients with different clinical phenotypes of myasthenia gravis.
Note: *-Significantly of difference from control p ≤ 0.05.
**-Significantly of difference from control p ≤ 0.001.
The number of positive cells in a spontaneous NBT-test is increased so much that they are practically are not capable to be activated by an additional stimulator (in stimulation by zimozan the cytochemical coefficient in a stimulated NBT-test was reduced by 1.6-1.9 times; the stimulation index was reduced by 1.3-1.5 times in all groups).
Therefore, neutrophil granulocytes of patients with all clinical phenotypes of myasthenia produce an increased number of activated forms of oxygen.
According to Kogan, “phagocytes are a powerful generator of active forms of oxygen capable not only to provide protection (microbicidal and antiblastomal) but also cause damage of their own cells by inactivation of ferments, destroying basal and cell membranes, change of the DNA structure which in the long run leads to destruction of cells-endotheliocytes, platelets, cardiomyocytes, fibroblasts, etc. Active forms of oxygen carry out their alterating affects through direct influence on cell components and organelles and through initiating free radical lipid peroxidation” [12].
To find out what possible causes of the studied changes of the phagocytosis function of neutrophil granulocytes could be, the concentration of proteins of acute phase was studied-C-reactive protein, C3 fragment of the complement, haptoglobin and ceruloplazmin. Patients of the participating groups had differently directed changes of concentration of proteins of acute phase. While analyzing the obtained data, the following was found out. In myasthenia without pathological changes of the thymus the concentration of C-reactive protein is evidentially increased; the concentration of haptoglobin is increased by 50%; the concentration of ceruloplasmin is evidentially decreased by 30% (p<0.05) (Table 3).
| Indicator Group | C-reactive protein mg/l |
Haptoglobin g/l |
Ceruloplasmin mg/l |
C3-fragment of complement mg/dl |
|---|---|---|---|---|
| Control group | 3.0 ± 2.8 | 1.09 ± 0.27 | 315.0 ± 45.0 | 100.0 ± 11.2 |
| M group | 14.82 ± 8.15* | 1.66 ± 0.24 | 209.3 ± 18.6* | 105.6 ± 20.1 |
| MH group | 25.71 ± 7.89* | 1.24 ± 0.46 | 138.3 ± 8.5* | 116.2 ± 10.4 |
| MT group | 20.77 ± 5.67* | 2.97 ± 0.57** | 267.0 ± 23.2* | 125.8 ± 12.2 |
Table 3: The concentration of acute phase proteins in patients with different clinical phenotypes of myasthenia gravis.
Note: *-Significantly of difference from control p ≤ 0.05.
**-Significantly of difference from control p ≤ 0.005.
In myasthenia with hyperplasia of the thymus the concentration of C-reactive protein was evidentially increased by 8 times, the concentration of haptoglobin was insignificantly increased (by 15-20%), the concentration of ceruloplasmin was evidentially decreased (more than 2 times more) (p<0.05). In myasthenia with thymoma the concentration of C-reactive protein was increased evidentially (6 times more) which is connected to the malignant character of the mediastinal tumor (C-reactive protein is one of tumorinduced markers), the concentration of haptoglobin is increased by 70% (p<0.05), the concentration of ceruloplasmin is insignificantly decreased (by 10%).
In our study the correlation between the concentration of acute phase proteins (C-reactive protein, haptoglobin and ceruloplasmin) and the concentration of C3 fragment of the complement was not found.
There was found a tendency to increased concentration of C3 fragment of the complement in a group of patients with myasthenia with neoplasia of the thymus. C3-fragment is capable to act as immunoregulating molecule with immunodepressing activity in relation to the synthesis of immunoglobulins, including antibodies. Thus, the increased concentration of C3-fragment of the complement can cause the decrease of produced antibodies in a group of patients with myasthenia with thymoma.
Discussion
The fact that the concentration of C3-fragment of the complement in all groups of patients with myasthenia is not decreased can testify the malfunction of the system function of the complement proteins, i.e., not enough activation of the complement system both in classic and alternate ways (otherwise there should be observed consumption of the complement which is characteristic of fighting an acute infection). It should be noted that this phenomenon is in agreement with immunocomplex theory of myasthenia, because immunocomplex pathology develops with insufficient complement [13,14].
From literature it is known that the main characteristics of proteins of acute phase are their obvious opsonizing, antiproteolitic and baktereostatic activity, as well as the ability to fix free radicals, to increase blood coagulation and to activate complement system [5].
The increase of the phagocytic index (the number of cells involved in phagocytosis) in all phenotypes of myasthenia can be connected to the following factors.
First is the physiological role of C-reactive protein (CRP). CRP is a component of non-specific immune response which can be found in early stages after antigen enters the body and acts as an opsonin by stimulating phagocytosis of neutrophils and cells of monocyticmacrophage system. It is known that C-reactive protein increases the mobility of leukocytes. When it is fixed with lymphocytes, it influences their functional activity by initiating reactions of precipitation, agglutination, phagocytosis and fixing the complement. The products of proteolysis of CRP, a CRP monomer and tuftsyn-like peptides-cause the increase of producing oxygen-anion, increase of activity of myeloperoxidase and adhesive properties, are chemattractants and moreover, they are regulators of proliferation of T-lymphocytes and Blymphocytes.
The complexes of C-reactive protein with ligands fixed on membranes of microorganisms and damages cells cause activation of cascade of the complement system in a classic way (fixing with C lq subunit of C l-fraction) and an alternate way. Another important function of CRP is obtained during this: to promote removal of bioactive substances from the system which are formed when own cell membranes are damaged, i.e., to improve opsonization of potential autoantigens [15]. Thus, the above described allows to assume that the increase of CRP concentration in myasthenia might be a reaction to the presence of autoantigen determinants in patients with myasthenia and is manifested as one of the factors of suppressing of autoimmune process.
Second, the intensification of the phagocytosis process can be explained by non-traditional interpretation of haptoglobin as one of opsonins of phagocytosis (the concentration of haptoglobin in all groups of patients with various phenotypes of myasthenia is increased) (Table 3).
Haptoglobin is a glikoprotein of blood plasma forming a complex with hemoglobin which practically is uncapable of dissociation. At present, it was demonstrated that free haptoglobin and its complexes with hemoglobin play an important role not only in supporting the iron reserves but also in controlling local inflammatory processes. Haptoglobin decreases ferment reserves and metabolism of phagocytes, which negatively influences the stimulation, inhibits the respiratory explosion by hydrolysis of peroxides which are released in the process of phagocyte action [16].
The readings of a spontaneous NBT-test (percentage of positive cells and ACKspont) were changing depending on the change of concentration of haptoglobin: in MH the concentration of haptoglobin is maximally decreased compared to all groups, the readings of a spontaneous NBT-test (percentage of positive cells and ACKspont) were decreased. The readings of a stimulated NBT-test didn’t change that abruptly, because neutrophil granulocytes were already stimulated due to the increased concentration of haptoglobin and further stimulation was impossible due to the depletion of enzymatic reserve.
Third, in all groups of patients with various phenotypes of myasthenia a decreased concentration of ceruloplasmin was observed (Table 3). Sokolov (2015) showed that in low concentration, ceruloplasmin causes increase of phagocytic index, while in high concentrations ceruloplasmin causes its decrease [17]. The mechanism of ceruloplasmin action is connected to its ability to form complexes with myeloperoxidase and lactoferrin of neutrophil granulocytes (i.e., the basis of inhibition of respiratory explosion of neutrophil granulocytes is SOD-like activity of ceruloplasmin, which also leads to impossibility of neutrophil granulocytes stimulation and is in agreement with the NBT test results (Table 2). These properties of ceruloplasmin are likely to manifest themselves in its interaction with the phagocyte system of neutrophil to the most degree in patients with various phenotypes of myasthenia.
Conclusions
In patients with myasthenia of all clinical phenotypes is found tension of the system of non-specific resistance of the body. Its peculiarity is the activation of phagocytosis system with the increase of phagocytosis index and spontaneous enzyme production of phagocytes, as well as decreased ability to stimulate in NBT-test.
In patients with myasthenia when a secondary autoimmune process is developed which originates in peripheral lymphoid tissue, a cascade of inflammatory reactions is induced which is accompanied by a considerable increase of concentration of C-reactive protein in patients of all studied groups, especially obvious in the MH group with hyperplasia of the thymus.
An insignificant increase of concentration of C3 fragment of the complement is observed which can testify that the complement system is activated not enough either in a classic or alternative way, which can also be one of the causes of developing immunocomplex causes of myasthenia.
On the one hand, haptoglobin in an increased concentration in all groups causes activation of phagocytosis, just like opsonin, including spontaneous formation of oxygen-anions. On the other hand, haptoglobin inhibits respiratory explosion of phagocytes and prevents the increase of formation of ferments in a stimulated NBT-test.
A decreased ceruloplasmin concentration contributes to the increase of phagocytic activity of neutrophil granulocytes. On the one hand, ceruloplasmin in low concentration helps to increase a phagocytic index and on the other hand, SOD-like activity of ceruloplasmin additionally inhibits a respiratory explosion of neutrophil granulocytes.
References
- Carr AS, Cardwell CR, McCarron PO, McConville J (2010) A systematic review of population based epidemiological studies in Myasthenia Gravis. BMC Neurol 10: 46.
- Boyko VV, Klimova EM, Kudrevich AN (2008) Treatment of myasthenia gravis taking into account immuno physiological phenotypes. Kharkiv: Publishing Scheinina EV, Kharkiv, Ukraine.
- http://www.myasthenia.ru/index.php?id=1
- Klimova EM, Boyko VV, Drozdova LA, Kordon TI, Kostya UP, et al. (2014) Features of the immuno physiological responses in patients with different clinical types of myasthenia gravis. Kharkiv surgical school 3: 46-53.
- Jain S, Gautam V, Naseem S (2011) Acute-phase proteins: As diagnostic tool. J Pharm BioalliedSci 3: 118-127.
- Muniz-Junqueira MI, Pecanha LM, Silva-Filho VL, Cardoso MC, Tosta CE (2003) Novel microtechnique for assessment of postnatal maturation of the phagocytic function of neutrophils and monocytes. ClinDiagn Lab Immunol 10: 1096-1102.
- Mayanskyy AN, Mayanskyy DN (1983) Essays on neutrophil granulocyte and macrophage. Novosybyrskoeotdelenie publishing house, Novosibirsk, Russia.
- Senju O, Takagi Y, Uzawa R, Iwasaki Y, Suzuki T, et al. (1986) A new immuno quantitative method by latex agglutination--application for the determination of serum C-reactive protein (CRP) and its clinical significance. J Clin Lab Immunol 19: 99-103.
- Plancke Y, Dautrexvaux M, Biserte G (1977) Change of human hemopexin isoelectric point upon heme binding. FEBS Lett 78: 291-294.
- Ravin HA (1961) Improved colometric enzymatic ceruloplasmin assay. J Lab Clin Med 58: 161-168.
- Nilsson B, Nilsson EK (2012) Complement Diagnostics: Concepts, Indications, and Practical Guidelines. Clinical and Developmental Immunology 962702.
- Kogan AX (1999) Phagocyte-dependent oxygen free radical autoaggression mechanisms in the pathogenesis of Internal Medicine.
- Peng X (2004) Research progress of the etiology and pathogeneses of myasthenia gravis.
- Huang H, Pan H, Wang H (2016) “Warming yang and invigorating qi” acupuncture alters acetylcholine receptor expression in the neuromuscular junction of rats with experimental autoimmune myasthenia gravis. Neural Regeneration Research. 11: 465-468.
- Rodriguez W, Mold C, Kataranovski M, Hutt JA, Marnell LL, et al. (2007) C-reactive protein-mediated suppression of nephrotoxic nephritis: role of macrophages, complement, and Fc receptors. J Immunol 178: 530-538.
- Oh SK, Pavlotsky N, Tauber AI (1990) Specific binding of haptoglobin to human neutrophils and its functional consequences. J LeukocBiol 47: 142-148.
- Sokolov AV, Zakharova ET, Kostevich VA, Samygina VR, Vasilyev VB (2014) Lactoferrin, myeloperoxidase, and ceruloplasmin: complementary gearwheels cranking physiological and pathological processes. Biometals 27: 815 - 828.
Citation: Klimova EM, Kalashnikova JV (2016) The Role of Acute Phase Proteins in Induction of Tension of Nonspecific Resistance System in Various Clinical Phenotypes of Myasthenia. J Clin Exp Pathol 6:300. DOI: 10.4172/2161-0681.1000300
Copyright: © 2016 Kalashnikova JV, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3591
- [From(publication date): 0-2016 - Dec 19, 2024]
- Breakdown by view type
- HTML page views: 2877
- PDF downloads: 714