Research Article Open Access
The Risk of Ileocolonic Perforation in Patients with Behet's Disease: Report of Three Cases and Review of the Literature
Mehmet Bektas1*, Cagdas Kalkan1, Irfan Soykan1, Ayse Boyvat2, Berna Savas3, Ethem Gecim4, Onur Keskin1, Ekin Kırcali1, Ali Tuzun1 and Necati Ormeci11Ankara University School of Medicine, Department of Gastroenterology, Ankara-Turkey
2Ankara University School of Medicine, Department of Dermatology, Ankara- Turkey
3Ankara University School of Medicine, Department of Pathology, Ankara-Turkey
4Ankara University School of Medicine, Department of Surgery, Ankara-Turkey
- *Corresponding Author:
- Mehmet Bektas
Ankara University School of Medicine
Department of Gastroenterology, Ibn-iSina Hospital
Sihhiye, Ankara-Turkey 06100
Tel: +903125082150
Fax: +90 312 363 6213
E-mail: mbektas@medicine.ankara.edu.tr
Received date: March 22, 2014; Accepted date: April 25, 2014; Published date: April 30, 2014
Citation: Bektas M, Kalkan C, Soykan I, Boyvat A and Savas B, et al., (2014) The Risk of Ileocolonic Perforation in Patients with Behçet's Disease: Report of Three Cases and Review of the Literature. J Gastroint Dig Syst 4:184. doi:10.4172/2161-069X.1000184
Copyright: © 2014 Bektas M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Introduction/Purpose: Intestinal Behcet’s disease may cause serious complications. Massive hemorrhage, fistulisation and intestinal perforation are encountered complications in approximately 50% of patients suffering from intestinal Behcet’s disease. Currently, there is not enough data inquiring iatrogenic ileocolonic perforation during colonoscopy in patients with intestinal Behcet’s disease; therefore we aimed to study intestinal Behcet’s disease patients who suffered perforation during or after colonoscopy. Methods: A total of 2615 colonoscopic examinations were performed between May 2002 and December 2007. Of these 2615 patients, main indication for colonoscopy was intestinal Behcet’s disease in 135 patients. Results: In total 135 patients with Behcet’s patients were assessed with colonoscopy due to presumed ileocolonic involvement. 8 out of 135 (5.9%) patients had ileal and colonic ulcers. 3 patients (2.22%) had iatrogenic perforation, 2 of whom had profound ulcers in proximal colon and ileum. The third case had ulcers in sigmoid colon, descending and transverse colon segments. All these 3 patients had undergone surgical intervention including ileal resection and right hemicolectomy. Discussion: Colonoscopic examination is commonly used in Behcet’s disease not only for diagnostic purposes but also for surveillance of intestinal involvement in Behcet’s disease. Volcano-shaped ulcers are specially inclined to perforate. Both clinicians and endoscopists should be alert against barotrauma applied during colonoscopy may cause perforation. Also patients should be followed-up necessarily and in case of abdominal pain after colonoscopic examination, colonic perforation should always be kept in mind.f
Keywords
Behcet’s disease; Colonoscopy; Ileocolonic perforation
Introduction
Behcet’ s disease (BD), is a multisystem inflammatory disorder characterized with repetitious oral and genital ulcers, skin lesions and relapsing ocular lesions which may affect nervous system, joints, blood vessels and sometimes gastrointestinal system [1-3]. Gastrointestinal involvement rates vary between 3 to 60 per cent in different countries [4-11].
Intestinal lesions of BD may come into the picture in a large scale from simple mucosal inflammation to infarct or ischemia due to small or large vessel involvement. These findings may vary from non-specific colitis to diffuse ulcers [12]. These lesions mostly arise from the ileocaecal segment and colonic involvement is seen less frequently [13]. Intestinal BD is an important morbidity and mortality reason depending on serious complications it causes [14,15]. Massive hemorrhage, fistulisation and intestinal perforation are encountered complications in approximately 50 % of patients suffering from intestinal BD [14,16,17]. Free perforation is a state with a poor prognosis and may increase panperitonitis which is a complication requiring emergent operation [14,18,19]. But there is no data about iatrogenic perforation during the colonoscopy for intestinal BD patients. In the current study, BD patients who experienced perforation during or after colonoscopy procedure were retrospectively analyzed.
Materials and Methods
135 patients with BD were assessed with colonoscopy to scan for lower gastrointestinal system involvement between May 2002 and December 2007. All of the participants corresponded the diagnostic criteria defined by International Study Group for Behcet’s Disease [20-23]. The patients with at least two or more active clinical symptoms related to BD were grouped as active BD group whereas the second group of patients was assessed as inactive BD group who had no symptom other than repetitious oral ulcers at least until one month ago [23-25].
Preparation for colonoscopy was done using Fleet phospho-soda 90 mL (C.B. Fleet Co., Inc. Lynchburg, VA, USA) for each patient. Premedication sedatives were used midazolam, meperidine and propofol. All colonoscopies were done by an experienced endoscopist (M.B.) using an advanced imaging technique videocolonoscopy (Fujinon E400 Tokyo, Japan). 2480 colonoscoy were done in the same time period because of other indications. In the current study, the BD patients who suffered from perforation during or after colonoscopy were retrospectively analyzed.
Results
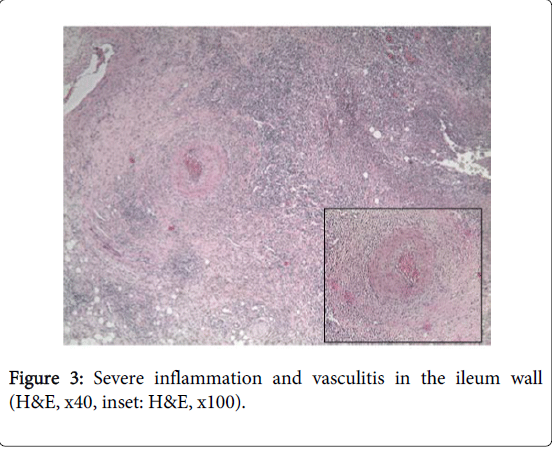
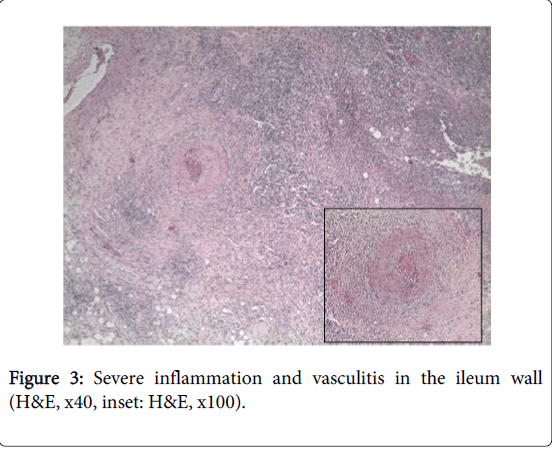
We included 77 female, 58 male BD patients whose mean age was 35.4 (between 18 and 69). Eight (5.9%) of 135 patients had ileal and colonic ulcers and the rest (127 cases) had normal colonoscopic examination. These patients had hematochezia, abdominal pain as gastrointestinal symptoms and anemia as laboratory finding. Some of the ulcers were reported to be superficial aphthous lesions whereas others were defined to be profound ulcers. 3 patients out of 8 (2.2%) had ileal and colonic ulcers; on the other hand the other 5 (3.7%) only had colonic involvement. The biopsies were taken from all ileal and colonic lesions for histopathological examination. The results of the biopsy materials revealed vasculitis. The characteristics of the patients were summarized in Table 1. Iatrogenic colon perforation during colonoscopy was encountered in 3 male patients. The mean age of whom was 33.6 (between 18- 56) years.
| No | Age | Sex | OU | GU | A | PT | U | PPE | EN | Symptom | Colonoscopy | Perforation |
| 1 | 18 | M | + | + | + | + | - | - | + | Hematochesia | Colonic ulcer | Ileum |
| 2 | 26 | M | + | + | - | + | + | + | - | Hematochesia | Ileal-colonic ulcer | Ileum |
| 3 | 56 | M | + | + | - | - | + | + | + | Hematochesia | Colonic ulcer | Ascending colon |
| 4 | 53 | F | + | + | - | + | - | + | - | Hematochesia | Colonic ulcer | None |
| 5 | 25 | F | + | + | + | + | - | + | - | Anemia | Ileal-colonic ulcer | None |
| 6 | 52 | F | + | + | - | + | + | + | - | Hematochesia | Colonic ulcer | None |
| 7 | 69 | M | + | + | - | + | + | + | + | Anemia | Colonic ulcer | None |
| 8 | 34 | M | + | + | + | + | - | + | - | Anemia | Ileal-colonic ulcer | None |
Table 1: Demographics of the patients who had ulcers as a finding of colonoscopic evaluation OU=Oral ulceration; GU = Genital ulceration; A=Arthritis; PT=Pathergy test; U=Uveitis; PPE=Papulopustular eruptions; EN=Erythema nodosum
2480 colonoscopy were done in the same time period because of other indications such as constipation, abdominal pain, diarrhea, inflammatory bowel disease, weight loss, rectal bleeding and iron deficiency anemia. In these, 240 (9.17%) patients were diagnosed with Crohn’s disease, 276 (10.5%) had ulcerative colitis, 46 (1.75%) had colo-rectal cancer. None of those groups had colonoscopic perforation as a complication.
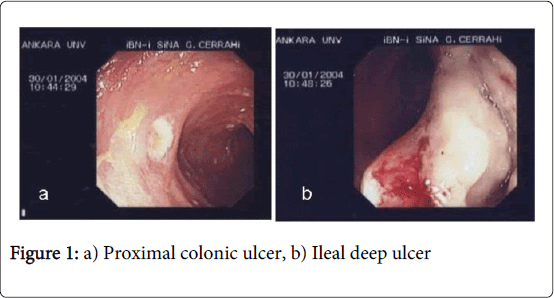
In all patients with BD except of 3 iatrogenic perforation patients were entered to terminal ileum. However2 patients of 3 perforated cases were examined until ceacum. The profound ulcers were seen in theproximal colon (Figure 1). The third case’s colon was examined up until mid-transverse colon and profound ulcers were observed through sigmoid, descending and transverse colon. Abdominal distention, pain, desaturation, hypotension and tachycardia developed during the procedure in all three patients. Physical examination revealed defense and rebound findings. The abdominal X- rays results were reported free intraperitoneal air. All patients were operated on the same day. Two of the perforations were seen in ileum and one in ascending colon during intraoperative examination. Ileal resection and hemicolectomy were applied to all cases (Figure 2) and the histopathological examination of all three resection materials revealed vasculitis (Figure 3).
Discussion
Intestinal involvement of BD is seen in between 1 to 60% of all patients [14,16,17]. Intestinal BD may be diagnosed in a patient if she/ he correspond to the criteria for BD by systemic findings and typical ulcers are seen either in small intestine or colon [15-17]. Documentation of typical ulcerative lesions with objective modalities is done in only 3- 25% of BD patients [12,14]. In this study out of 135 patients only 8 (5.9%) of whom were determined to have ileocolonic involvement; 4 (2.9%) of whom had superficial aphthous ulcers and the other 4 (2.9%) had volcano-shaped profound ulcers. Köklü et al. had reported endoscopic colitis in only 2% had endoscopic colitis whereas the given rate increased up to 15% with histopathological examination in 50 BD patients [19].
Intestinal BD may cause serious complications. Massive hemorrhage, fistulisation and intestinal perforation are encountered complications in approximately 50% of patients suffering from intestinal BD. Free perforation can lead to panperitonitis, requiring emergent operation with a poor prognosis [14,18,19]. The studies reveal that free intestinal perforation is more frequently seen in far eastern countries [26,27]. The pathophysiology of perforation in intestinal BD is not really clear; nevertheless we have put forth the following into consideration: 1.Typical intestinal BD ulcers are usually large, separate and excavated in shape [28-31]. 2. Combined intestinal dilatation may contribute to perforation. High intraluminal pressured intestinal distention proximal to obstruction segment may increase perforation risk [32-34]. 3. Long term steroid use may be related to intestinal perforation development. Steroid treatment may develop peritonitis via inhibiting the closing process of perforation [35].
Some risk factors for intestinal perforation are defined in the literature which may be listed as follows: young age at the time of diagnosis, a history of operation and volcano shaped intestinal ulcers [36-39]. Kim et al. were found to cause of volcano shaped ulcers more often than other ulcer types for spontaneous intestinal perforation [33]. In our study on the other hand, all patients with intestinal perforation had either volcano shaped or profound ulcers. There was no usage of steroid history of in these patients. The perforated cases were aged between 18 and 56; 3 of them were evaluated because of hematochezia and 2 of their colonoscopies revealed volcano shaped ulcers in both ileum and proximal colon whereas the other one had profound ulcers in sigmoid, descending and transverse colon. Another study, Moon et al. 33 patients (25.6%) out of 129 symptomatic intestinal Behcet’s were diagnosed with intestinal perforation; it was emphasized that all cases were operated and the age interval was between 12 and 70, mean age of the group was 33.8 years [38]. In this study, there were no history of acute abdominal pain and free perforation from colon and ileumin our BD patients. All perforations were occurred after colonoscopic procedure. Our experience is the first documentation that highlights the high risk of ileocolonic perforation during colonoscopic procedure in intestinal BD.
Ileal segmental resections and right hemicolectomy preferred for spontaneous perforation in order to decrease both perforated intestinal BD incidence and relapse rates [18-19]. In a study conducted with 7 cases in 1991 by Sayek et al. 6 cases were applied right hemicolectomy and ileal resection whereas the last patient was applied right hemicolectomy only secondary to intestinal anastomosis leakage [18]. Many other studies composed of small surgical series have evaluated perforation patients after the incident in means of relapse after operation and yielded the results as follows: a history positive for intestinal perforation and fistulisation increases risk for re-perforation; and the suggested length of resection was controversial [40]. Kim et al determined that relapse rates were 13% (3 out of 23 patients) and 50 % (8 out of 16), in medical treatment and operation groups relatively [33]. Our patients were applied ileal resection and right hemicolectomy, following a similar surgical fashion; and no secondary surgical procedure was necessary. All resection materials of three perforated patients were proved to have vasculitis on histopathological examination.
It is also important to acquire full remission in perforated cases during early post-operative period in view of preventing relapses. As in inflammatory bowel diseases, sulphasalazine and steroids are preferred first line treatment choices [41-46]. Most systemic or local medications are either given alone, or combined with colchicine and steroids [45-47]. In our series we were able to achieve remissions with colchicine, corticosteroid and azathioprine therapy, and no exacerbation experienced during our 3-year follow up.
Endoscopic procedures such as gastroscopy and colonoscopy are widely use for the diagnosis of gastrointestinal system disease. Colonic perforation resulting from colonoscopic and sigmoidoscopic procedures is a rare but serious complication with high rates of morbidity and mortality [48-51]. The frequency of perforations after colonoscopy is estimated to be 0.03% to 0.8% for diagnostic colonoscopy and 0.15% to 3% for therapeutic colonoscopy [52]. Perforations that occur during diagnostic colonoscopy are due to direct mechanical penetration with the instrument tip, sharp flexion of the colonoscope, high pressure applied when a loop is formed or barotrauma as a result of aggressive gas insufflations [53-54]. In a retrospective study, the most common underlying cause for bowel perforation was direct mechanical injury of the colonic wall by the colonoscope. It occurred in patients with diverticular disease or a strictured, severely diseased colonic segment. These risk factors were in accordance with those noted in the literature [55-56]. The most frequent site of perforation was the sigmoid colon, as in other studies [57-60]. This may be explained by its anatomical characteristics of frequent redundancy or narrowing from diverticular disease or adhesions after previous pelvic operations [60].
In this study, iatrogenic colon perforation did notoccur in Crohn’s disease andulcerative colitis patients. There were no abdominopelvic operation history of BD patients and colonic diverticula were not seen during the colonoscopic examination in this group. We thought that barotrauma induced perforation for all perforations were occurred proximal colon.
In conclusion, colonoscopy is a scanning modality which is not only diagnostic but also may be used periodically during follow- ups, or to display relapses responsive to medical treatment. Perforation may develop during colonoscopy procedure. Especially, discrete ulcers typically have a round or oval ‘‘punched-out’’ appearance and with a tendency to bleed or perforate. For these reasons during colonoscopy low pressure of air should be applied for minimal barotrauma and maximum caution for perforation should be shown during follow-up after the procedure.
References
- Behcet H (1937) Über rezidivierende, aphthose durch ein Virus verursachte Geschwure am Mund, am Auge und an den Genitalien. Dermatol Wochenschr 105:1152-1157.
- Kobayashi K, Ueno F, Bito S, Iwao Y, Fukushima T, et al. (2007) Development of consensus statements for the diagnosis and management of intestinal Behçet's disease using a modified Delphi approach. J Gastroenterol 42: 737-745.
- Sakane T, Takeno M, Suzuki N, Inaba G (1999) Behçet's disease. N Engl J Med 341: 1284-1291.
- al-Aboosi MM, al Salem M, Saadeh A, al-Jamal M, Hijawi M, et al. (1996) Behçet's disease: clinical study of Jordanian patients. Int J Dermatol 35: 623-625.
- Al-Otaibi LM, Porter SR, Poate TW (2005) Behçet's disease: a review. J Dent Res 84: 209-222.
- Jankowski J, Crombie I, Jankowski R (1992) Behçet's syndrome in Scotland. Postgrad Med J 68: 566-570.
- Shimizu T, Ehrlich GE, Inaba G, Hayashi K (1979) Behçet disease (Behçet syndrome). Semin Arthritis Rheum 8: 223-260.
- Chen YC, Chang HW (2001) Clinical characteristics of Behçet's disease in southern Taiwan. J Microbiol Immunol Infect 34: 207-210.
- Tunc R, Keyman E, Melikoglu M, Fresko I, Yazici H (2002) Target organ associations in Turkish patients with Behçet's disease: a cross sectional study by exploratory factor analysis. J Rheumatol 29: 2393-2396.
- al-Dalaan AN, al Balaa SR, el Ramahi K, al-Kawi Z, Bohlega S, et al. (1994) Behçet's disease in Saudi Arabia. J Rheumatol 21: 658-661.
- Barnes CG (2006) Treatment of Behcet's syndrome. Rheumatology (Oxford) 45: 245-247.
- Bayraktar Y, Ozaslan E, Van Thiel DH (2000) Gastrointestinal manifestations of Behcet's disease. J Clin Gastroenterol 30: 144-154.
- Takada Y, Fujita Y, Igarashi M, Katsumata T, Okabe H, et al. (1997) Intestinal Behçet's disease--pathognomonic changes in intramucosal lymphoid tissues and effect of a "rest cure" on intestinal lesions. J Gastroenterol 32: 598-604.
- Kasahara Y, Tanaka S, Nishino M, Umemura H, Shiraha S, et al. (1981) Intestinal involvement in Behçet's disease: review of 136 surgical cases in the Japanese literature. Dis Colon Rectum 24: 103-106.
- Baba S, Maruta M, Ando K, Teramoto T, Endo I (1976) Intestinal Behçet's disease: report of five cases. Dis Colon Rectum 19: 428-440.
- Ketch LL, Buerk CA, Liechty D (1980) Surgical implications of Behçet's disease. Arch Surg 115: 759-760.
- Smith JA, Siddiqui D (2002) Intestinal Behçet's disease presenting as a massive acute lower gastrointestinal bleed. Dig Dis Sci 47: 517-521.
- Sayek I, Aran O, Uzunalimoglu B, Hersek E (1991) Intestinal Behçet's disease: surgical experience in seven cases. Hepatogastroenterology 38: 81-83.
- Oshima Y, Shimizu T, Yokohari R, Matsumoto T, Kano K, et al. (1963) Clinical Studies on Behçet's Syndrome. Ann Rheum Dis 22: 36-45.
- Köklü S, Yüksel O, Onur I, Unverdi S, BiyikoÄŸlu I, et al. (2010) Ileocolonic involvement in Behçet's disease: endoscopic and histological evaluation. Digestion 81: 214-217.
- Bradbury AW, Milne AA, Murie JA (1994) Surgical aspects of Behçet's disease. Br J Surg 81: 1712-1721.
- Wullstein C, Köppen M, Gross E (1999) Laparoscopic treatment of colonic perforations related to colonoscopy. Surg Endosc 13: 484-487.
- Young HS, Keeffe EB (1998) Complications of gastrointestinal endoscopy. In: Sleisenger & Fordtran’s gastrointestinal and liver diseases. 6th ed. Philadelphia: WB Saunders, 301-309
- Orsoni P, Berdah S, Verrier C, Caamano A, Sastre B, et al. (1997) Colonic perforation due to colonoscopy: a retrospective study of 48 cases. Endoscopy 29: 160-164.
- [No authors listed] (1990) Criteria for diagnosis of Behçet's disease. International Study Group for Behçet's Disease. Lancet 335: 1078-1080.
- Brodie TE, Ochsner JL (1973) Behçet's syndrome with ulcerative oesophagitis: report of the first case. Thorax 28: 637-640.
- Gamble CN, Wiesner KB, Shapiro RF, Boyer WJ (1979) The immune complex pathogenesis of glomerulonephritis and pulmonary vasculitis in Behçet's disease. Am J Med 66: 1031-1039.
- Bechgaard P (1940) Et tilfaelds af recidiverende aphtøs stomatitis ledsaget af conjunctivitis og ulcerationer paa genitalia oghud. Ugeskr Laeger. 102:1019-1023.
- Korman U, Cantasdemir M, Kurugoglu S, Mihmanli I, Soylu N, et al. (2003) Enteroclysis findings of intestinal Behcet disease: a comparative study with Crohn disease. Abdom Imaging 28: 308-312.
- Lee CR, Kim WH, Cho YS, Kim MH, Kim JH, et al. (2001) Colonoscopic findings in intestinal Behçet's disease. Inflamm Bowel Dis 7: 243-249.
- Chou SJ, Chen VT, Jan HC, Lou MA, Liu YM (2007) Intestinal perforations in Behçet's disease. J Gastrointest Surg 11: 508-514.
- Lee SK, Kim BK, Kim TI, Kim WH (2009) Differential diagnosis of intestinal Behçet's disease and Crohn's disease by colonoscopic findings. Endoscopy 41: 9-16.
- Kim JS, Lim SH, Choi IJ, Moon H, Jung HC, et al. (2000) Prediction of the clinical course of Behçet's colitis according to macroscopic classification by colonoscopy. Endoscopy 32: 635-640.
- Greenstein AJ, Mann D, Sachar DB, Aufses AH Jr (1985) Free perforation in Crohn's disease: I. A survey of 99 cases. Am J Gastroenterol 80: 682-689.
- Greenstein AJ, Sachar DB, Mann D, Lachman P, Heimann T, et al. (1987) Spontaneous free perforation and perforated abscess in 30 patients with Crohn's disease. Ann Surg 205: 72-76.
- Katz S, Schulman N, Levin L (1986) Free perforation in Crohn's disease: a report of 33 cases and review of literature. Am J Gastroenterol 81: 38-43.
- Turan M, Sen M, Koyuncu A, Aydin C, Arici S (2003) Sigmoid colon perforation as an unusual complication of Behçet's syndrome: report of a case. Surg Today 33: 383-386.
- Moon CM, Cheon JH, Shin JK, Jeon SM, Bok HJ, et al. (2010) Prediction of free bowel perforation in patients with intestinal Behçet's disease using clinical and colonoscopic findings. Dig Dis Sci 55: 2904-2911.
- Toynton SC (1994) Behçet's syndrome: an unusual cause of ileal perforation. J Clin Gastroenterol 19: 84-85.
- Isik B, Ara C, Kirimlioglu H, Sogutlu G, Yilmaz M, et al. (2005) Single or multiple perforations with varying locations as a complication of intestinal Behçet's disease: report of three cases. Scand J Gastroenterol 40: 599-603.
- Iida M, Kobayashi H, Matsumoto T, Okada M, Fuchigami T, et al. (1994) Postoperative recurrence in patients with intestinal Behçet's disease. Dis Colon Rectum 37: 16-21.
- Choi IJ, Kim JS, Cha SD, Jung HC, Park JG, et al. (2000) Long-term clinical course and prognostic factors in intestinal Behçet's disease. Dis Colon Rectum 43: 692-700.
- Lee KS, Kim SJ, Lee BC, Yoon DS, Lee WJ, et al. (1997) Surgical treatment of intestinal Behçet's disease. Yonsei Med J 38: 455-460.
- Naganuma M, Iwao Y, Inoue N, Hisamatsu T, Imaeda H, et al. (2000) Analysis of clinical course and long-term prognosis of surgical and nonsurgical patients with intestinal Behçet's disease. Am J Gastroenterol 95: 2848-2851.
- Toda K, Shiratori Y, Yasuda M, Enya M, Uematsu T, et al. (2002) Therapeutic effect of intraarterial prednisolone injection in severe intestinal Behçet's disease. J Gastroenterol 37: 844-848.
- Beales IL (1998) Gastrointestinal involvement in Behçet's syndrome. Am J Gastroenterol 93: 2633.
- Hassard PV, Binder SW, Nelson V, Vasiliauskas EA (2001) Anti-tumor necrosis factor monoclonal antibody therapy for gastrointestinal Behçet's disease: a case report. Gastroenterology 120: 995-999.
- Anderson ML, Pasha TM, Leighton JA (2000) Endoscopic perforation of the colon: lessons from a 10-year study. Am J Gastroenterol 95: 3418-3422.
- Carpio G, Albu E, Gumbs MA, Gerst PH (1989) Management of colonic perforation after colonoscopy. Report of three cases. Dis Colon Rectum 32: 624-626.
- Garbay JR, Suc B, Rotman N, Fourtanier G, Escat J (1996) Multicentre study of surgical complications of colonoscopy. Br J Surg 83: 42-44.
- Jentschura D, Raute M, Winter J, Henkel T, Kraus M, et al. (1994) Complications in endoscopy of the lower gastrointestinal tract. Therapy and prognosis. Surg Endosc 8: 672-676.
- Wullstein C, Köppen M, Gross E (1999) Laparoscopic treatment of colonic perforations related to colonoscopy. Surg Endosc 13: 484-487.
- Young HS, Keeffe EB (1998) Complications of gastrointestinal endoscopy. In: Sleisenger & Fordtran’s gastrointestinal and liver diseases. 6th ed. Philadelphia: WB Saunders 301-309.
- Orsoni P, Berdah S, Verrier C, Caamano A, Sastre B, et al. (1997) Colonic perforation due to colonoscopy: a retrospective study of 48 cases. Endoscopy 29: 160-164.
- Hunt RH (1983) Towards safer colonoscopy. Gut 24: 371-375.
- Macrae FA, Tan KG, Williams CB (1983) Towards safer colonoscopy: a report on the complications of 5000 diagnostic or therapeutic colonoscopies. Gut 24: 376-383.
- Farley DR, Bannon MP, Zietlow SP, Pemberton JH, Ilstrup DM, et al. (1997) Management of colonoscopic perforations. Mayo Clin Proc 72: 729-733.
- Hall C, Dorricott NJ, Donovan IA, Neoptolemos JP (1991) Colon perforation during colonoscopy: surgical versus conservative management. Br J Surg 78: 542-544.
- Dafnis G, Ekbom A, Pahlman L, Blomqvist P (2001) Complications of diagnostic and therapeutic colonoscopy within a defined population in Sweden. Gastrointest Endosc 54: 302-309.
- Damore LJ 2nd, Rantis PC, Vernava AM 3rd, Longo WE (1996) Colonoscopic perforations. Etiology, diagnosis, and management. Dis Colon Rectum 39: 1308-1314.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14734
- [From(publication date):
June-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10179
- PDF downloads : 4555