The Risk Factors for Antenatal Bleeding in Pregnancy with Placenta Previa
Received: 09-Dec-2017 / Accepted Date: 28-Dec-2017 / Published Date: 30-Dec-2017 DOI: 10.4172/2376-127X.1000362
Abstract
Objective: The majority of previa-related bleeding is due to an adhesive placenta. The risk factors are already well known. Although antenatal bleeding in women with placenta previa is another problem, the risk factors have not been identified. Our aim is to investigate the risk factors for antenatal bleeding in women with placenta previa.
Methods: This was a retrospective study of postpartum women who received an ultrasound diagnosis of placenta previa. Included women were divided into two groups based on whether they had antenatal bleeding or not. Sonographic images were reviewed. Parameters assessed included loss of the retroplacental clear zone, irregularity of uterine-bladder interface, number of lacunar spaces, vasa previa and increased vascularity around placenta. We also assessed the type of placenta previa, placenta location, cervical length at third trimester and obstetric histories. Statistical analyses were performed using a t-test, X2 test and logistic regression test.
Results: Of 109 patients included, 55 (50.5%) experienced antenatal bleeding. There was no significant difference in maternal age between the two groups (P=0.903). Obstetric histories, cervical length at third trimester and sonographic findings were not significantly different.
Conclusion: Prediction of antenatal bleeding in placenta previa using obstetrical history and sonographic finding is difficult.
Keywords: Placenta previa; Antenatal bleeding; Ultrasound
Introduction
Maternal mortality has declined substantially, but it is still reported as 1.7% [1]. Antenatal and postnatal bleeding are major causes of maternal mortality. Particularly, placenta previa causes massive hemorrhage. The incidence of placenta previa increases with an increase of cesarean deliveries. The rate of placenta previa is increasing, presenting in 1.3% of pregnancies [2]. Bleeding in placenta previa is often associated with placental adhesion. In this case, bleeding occurs after the placenta has fallen post-delivery and the amount of bleeding may vary depending on the degree of adhesion. Therefore, many studies on placenta previa have been focused on the placenta accreta. Many studies have been carried out to predict placenta accreta associated with placenta previa. Placenta accreta-associated bleeding occurs postpartum, so adequate explanation and preparations for bleeding before surgery can prepare for excessive bleeding. However, the incidence of placenta previa-associated antenatal hemorrhage is reported at 1%. Most of the antenatal hemorrhage occurs suddenly without any symptoms. The antenatal hemorrhage may lead directly to preterm labor, which even affects neonatal prognosis. Gibbins et al. reported that placenta previa is an independent risk factor for maternal hemorrhagic morbidity, although it is not associated with placental adhesion [3].
In this study, we evaluated the risk factors for antenatal bleeding in placenta previa.
Materials and Methods
This study retrospectively analyzed maternal records from January 2012 to December 2014 of women who delivered at the Department of Obstetrics and Gynecology, Haeundae Paik Hospital, Inje University. This study included pregnant women who were diagnosed with placenta previa after 24 weeks of gestation and who gave birth at this hospital. Only singleton pregnancies were included.
The exclusion criteria are as follows: (1) Previous vaginal bleeding in the current pregnancy, (2) multiple gestation, (3) previous or current history of preterm labor, ruptured membrane, incompetent internal os of cervix, (4) fetal growth restriction or fetal congenital anomalies, (5) cause of preterm birth was not related to placenta previa, such as maternal medical complications, (6) diagnosis with previa after 24 gestational weeks but the placenta was raised to the fundus in the third trimester of pregnancy and (7) patients who were not able to confirm ultrasonographic findings using picture archiving and communication system (PACS). Women included in the study were divided into the bleeding group and control group based on the presence or absence of antenatal hemorrhage.
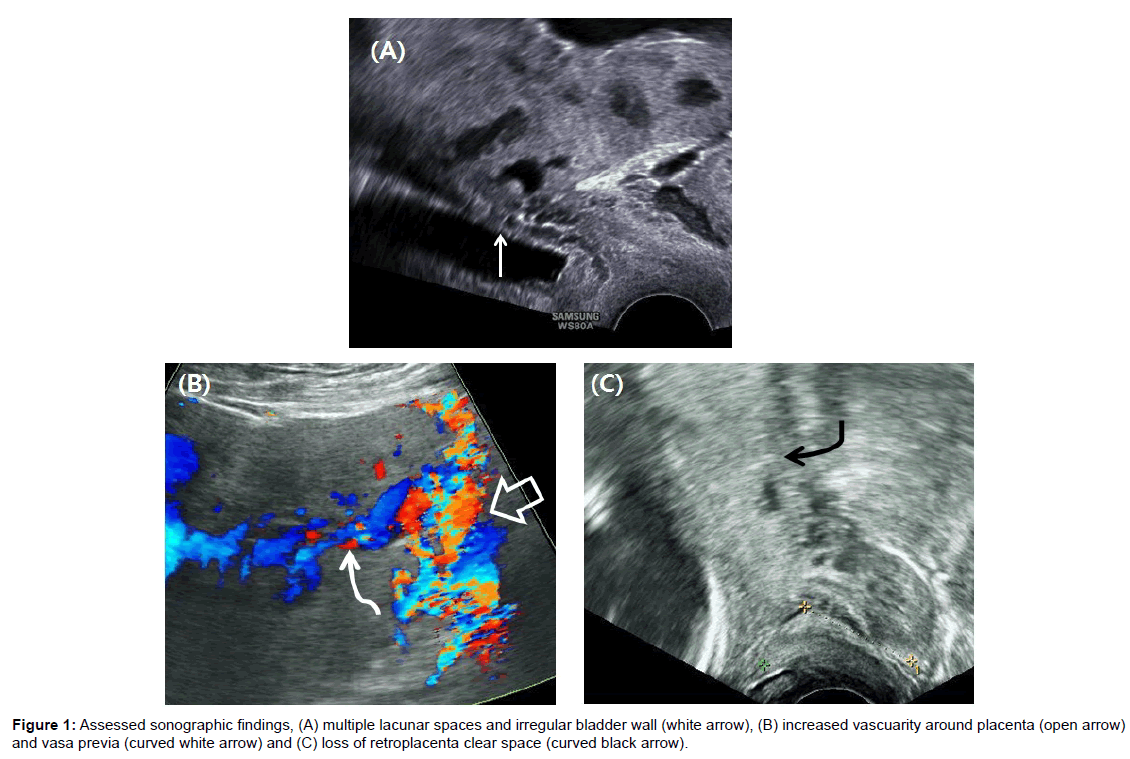
All ultrasound examinations had been performed using an RIC5-9-F transvaginal probe (2.0-5.0 MHz) and a C1-5-D transabdominal probe (4.0-9.0 MHz, Voluson E8, GE Healthcare, Kretztechnik, Zipf, Austria) during pregnancy. Grayscale imaging and color Doppler imaging were used. All antenatal ultrasound pictures had been stored in PACS. The stored pictures were reviewed by an obstetric expert (author). The factors analyzed for predicting antenatal bleeding were as follows: Parity, maternal age at delivery, previous cesarean history, location of placenta, severity of the placenta previa (complete versus partial previa), cervical length less than 3 cm during the third trimester, vasa previa, loss of retroplacental clear zone, multiple lacunar space more than 3, increased vascularity around the placenta and irregularity of the uterine-bladder interface. The ultrasound findings were diagnosed according to following criteria. If a major portion of the placenta covered the anterior lower uterine segment, the placenta was considered to be anterior. A complete placenta previa was defined as the placenta covering the os by more than 2 cm. All placenta previa patients were measured for cervical length at every regular follow-up after diagnosis. The cervical length was chosen as the last measured length just before birth. The decidua basalis between the placenta and the myometrium should be seen as anechoic line at the ultrasound imaging. In the case of placental adhesion, this line may be lost. These cases are referred to as loss of the retroplacental clear zone. Multiple lacunar spaces are defined when there are three or more anechoic areas of various shapes and sizes in the placenta (Figure 1).
Statistical analysis was performed with a t-test and X2 test using the SPSS program. Statistical significance was defined as a p-value lower than 0.05.
Results
During the study period, there were 1391 patients who delivered, among them, there were 116 patients who were diagnosed with placenta previa. Seven cases were excluded from this study according to exclusion criteia. A total of 109 placenta previa patients were included in the study, of which 55 (50.0%) experiences antenatal bleeding.
Demographics of the included women are presented in Table 1. There was no significant difference in maternal age between two groups (33.1 years old versus 32.9 years old, P=0.903). There was no statistically significant difference between the antenatal bleeding group and the control group, including parity, severity of placenta previa, location of the placenta, vasa previa and prior cesarean history. Short cervical length of less than 3 cm in the third trimester was not associated with antenatal bleeding. The ultrasound findings that can predict postpartum bleeding such as loss of retroplacental clear space, lacunar space of more than three, increased vascularity around placenta and irregularity of uterinebladder interface were not significantly different between the antenatal bleeding group and control group (Tables 1 and 2).
| Basic characteristics | YES | NO | P |
|---|---|---|---|
| n=55 | n=54 | ||
| Maternal age | 33.1 | 32.9 | 0.903 |
| Previa totalis (n=50) | 29 | 26 | 0.268 |
| Anterior placenta (n=26) | 15 | 11 | 0.164 |
| Multigravida (n=49) | 29 | 20 | 0.073 |
| Prior caesarean delivery (n=17) | 9 | 8 | 0.517 |
| Gestational age at delivery | 33.7 | 37.2 | <0.001 |
Table 1: The basic dermographics of included women.
| Risk factor for antenatal bleeding | YES | NO | P | |
|---|---|---|---|---|
| n=55 | n=54 | |||
| Short cervical length at 3rd trimester1680.273 | ||||
| Vasa previa (n=11) | 7 | 4 | 0.274 | |
| Retroplacental clear space (n=84) | 39 | 45 | 0.094 | |
| Lacunar space >3 (n=19) | 10 | 9 | 0.518 | |
| Increased vascularity (n=66) | 33 | 33 | 0.531 | |
| Irregularity of uterine-bladder interface (n=43) | 26 | 17 | 0.186 | |
Table 2: The comparison of ultrasound findings between two groups.
Discussion
Antepartum and postpartum hemorrhage are very important and dangerous problems in placenta previa. Placenta previa is diagnosed when the placenta covers the cervix after 20 weeks of gestation. Although placenta previa is diagnosed during early pregnancy, the placenta goes up to the uterine fundus as the pregnancy progresses. In the late pregnancy, the blood circulation in the uterine fundus increases and the placenta grows toward the uterine fundus. The placenta, which is implanted in the lower part of the uterus, is degenerated and depressed due to malnutrition, called trophotropism. The lower part of the uterus expands and the distance between the placenta and uterus increases as the pregnancy progresses. However, if the placenta adheres to the uterine muscle layer, the placenta cannot rise and remains in the lower uterus, becoming placenta previa. Histologically, placenta adhesion is associated with a partial loss of the basal decidual membrane or abnormal development of the fibrin layer (Nitabuch layer). If a previous cesarean section was performed, there is a problem of angiogenesis in the previous operation site that may cause partial hypoxia. This hypoxia leads to incomplete decidualization and abnormal trophoblast invasion that can cause placental adhesion [4]. There have been many studies to predict placental adhesion during pregnancy [5-8]. There are several sonographic findings that can predict placental adhesion to the uterine myometrium beyond the nitabuch layer. These sonographic findings included location of the placenta, loss of the retroplacenta clear space, multiple lacunar spaces, irregularity of the uterine-bladder interface and bridging vessels, thin myometrial thickness and increased vascularity around placenta. Rac et al. tried to quantitatively predict placental adhesion by showing these sonographic findings as PAI (placenta accreta index) scores [9]. The parameters, including prior cesarean deliveries, lacunar spaces, sagittal smallest myometrial thickness, anterior placenta previa, bridging vessels, constitute the PAI score. This scoring system may be useful for predicting the risk of placenta accreta, but it does not reflect the risk of antenatal bleeding. Recently, many attempts have been made to detect the extent of placental invasion through uterine muscle layer through magnetic resonance image (MRI) [6,10,11]. However, the cost and inconvenience of MRI should be considered.
Conclusion
Many studies have been done to predict postpartum hemorrhage. Therefore, if the uterine accreta is predicted by prenatal ultrasonography or MRI, the severity of accreta can be predicted. Depending on the findings, a physician can prepare for a large amount of bleeding. Bleeding associated with placenta accreta occurs after placental extraction, so bleeding begins after delivery. Even if the degree of bleeding is not predicted, the timing of the bleeding can be predicted. This possibility is a significant difference between antenatal bleeding and postnatal bleeding with placenta previa. The time at which antenatal bleeding begins cannot be predicted. Preparing for the blood, fluid and manpower is one of the best ways to reduce bleeding complications. Therefore, predicting the timing and severity of bleeding is very important. The mechanism of antenatal bleeding in placenta previa is different than with postnatal bleeding in placenta previa. In other words, antepartum bleeding is not related to placenta accreta. When the placenta is implanted in the lower part of the uterus, which has a thin muscle layer, the placenta easily falls away from the uterine myometrium, even with mild contraction and effacement of the uterus. Abnormal placentation and a poor blood supply from the uterine wall in the lower segment may cause antenatal bleeding [12]. If a small uterine contraction occurs, a small amount of hemorrhage occurs in the placenta with poor placentation and this small amount of hemorrhage induces detachment of the surrounding placenta, resulting in massive bleeding. Therefore, bleeding cannot be predicted in the same way as with uterine accreta. Hasegawa et al. reported similar results on whether sonographic findings could predict prenatal bleeding. They compared the sonographic findings in patients who required an emergency cesarean section due to uncontrollable antenatal bleeding with those of patients who did not. No sonographic finding could predict antenatal bleeding and the eventual need for an emergency cesarean section. In this study, the incidence of antenatal bleeding in placenta previa was 56%, which is similar to that of our study [13]. Preterm labor can promote antenatal bleeding, because the mechanism of antenatal bleeding in placenta previa is related to poor placentation rather than placental adhesion. Therefore, sonographic findings predicting preterm labor may be more meaningful for antenatal hemorrhage than sonographic findings predicting placental adhesion. Thus, it has been reported that cervical length in the third trimester of pregnancy is helpful for predicting antenatal bleeding [12,14,15]. However, Hasegawa et al. did not attempt to measure cervical length [13]. Zaitoun et al. studied the relationship between cervical length and clinical outcome in cases of complete placenta previa. A short cervical length of less than 3 cm could predict the risk of antenatal hemorrhage (p=0.004). However, a short cervical length of less than 3 cm had no significant effect on cesarean hysterectomy and peripartum blood transfusion in their study [15]. Shin et al. also reported the effect of cervical length on placenta previa. According to their report, cervical length was not significantly different between the bleeding group and control group until 31 gestational weeks. After that, cervical length in the bleeding group decreased abruptly. This serial change in cervical length was significantly associated with antenatal bleeding [14]. In our study, uterine cervical length measurement during the third trimester of pregnancy was not predictive of antenatal bleeding. This finding may be due to the low number of cases or the retrospective nature of this study. The patients were referred to our hospital because of heavy bleeding and underwent emergency operation immediately were excluded from the study because their ultrasound findings were not stored in the PACS. In addition, patients diagnosed with placenta previa and who gave a birth at another hospital were also excluded. The timing of the measurement of cervical length was determined by the timing of antenatal bleeding. In the future, a well-controlled study is needed on whether antenatal bleeding in placenta previa can be predicted by measurement of cervical length.
Matsubara et al. reported that the placental location may affect the amount of bleeding in placenta previa [8]. However, in this study, placental location did not show any significant difference between the bleeding group and the control group.
Limitations
The limitation of this study is that this is a retrospective study in a single center and the number of included cases is small. However, unlike postpartum bleeding that occurs after placenta removal, antenatal bleeding cannot be predicted, so it is very meaningful to try to find a predictable factor. In this study, antepartum bleeding could not be predicted by ultrasonographic findings that could predict postpartum bleeding in placenta previa. More controlled studies will be needed to determine if antenatal bleeding can be predicted by cervical length measurement, patient history or ultrasonographic findings.
Acknowledgement
This study was supported by a 2011 Inje University research grant.
References
- Alkema L, Chou D, Hogan D, Zhang S, Moller AB, et al. (2015) Global, regional and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 387: 462-474.
- Grobman WA, Gersnoviez R, Landon MB, Spong CY, Leveno KJ, et al. (2007) Pregnancy outcomes for women with placenta previa in relation to the number of prior cesarean deliveries. Obstet Gynecol 110: 1249-1255.
- Gibbins KJ, Einerson BD, Varner MW, Silver RM (2017) Placenta previa and maternal hemorrhagic morbidity. J Mater Fetal Neonatal Med 21: 1-6
- Wortman AC, Alexander JM (2013) Placenta accreta, increta and percreta. Obstet Gynecol Clin N Am 40: 137-154.
- D'Antonio F, Iacovella C, Bhide A (2013) Prenatal identification of invasive placentation using ultrasound: Systemic review and meta-analysis. Ultrasound Obstet Gynecol 42: 509-517.
- Shetty MK, Dryden DK (2015) Morbidly adherent placenta: Ultrasound Assessment and supplemental role of magnetic resonance imaging. Semin Ultrasound CT MR 36: 324-331.
- Rac MW, Moschos E, Wells CE, McIntire DD, Dashe JS, et al. (2016) Sonographic findings of morbidly adherent placenta in the first trimester. J Ultrasound Med 35: 263-269.
- Matsubara S, Baba Y, Takahashi H (2017) Placenta previa and hemorrhage: The placental location may be an important determinant of the bleeding amount. J Matern Fetal Neonatal Med 20: 1-2.
- Rac MW, Dashe JS, Wells CE, Moschos E, McIntire DD, et al. (2015) Ultrasound predictors of placental invasion: The placenta accreta index. Am J Obstet Gynecol.
- Tanimura K, Yamasaki Y, Ebina Y, Deguchi M, Ueno Y, et al. (2015) Prediction of adherent placenta in pregnancy with placenta previa using ultrasonography and magnetic resonance imaging. Eur J Obstet Gynecol Reprod Biol 187: 41-44.
- Lim G, Horowitz JM, Berggruen S, Ernst LM, Linn RL, et al. (2016) Correlation of probability scores of placenta accreta on magnetic resonance imaging with hemorrhagic morbidity. J Clin Anesth 34: 261-269.
- Hasegawa J, Nakamura M, Hamada S, Matsuoka R, Ichizuka K, et al. (2012) Prediction of hemorrhage in placenta previa. Taiwan J Obstet Gynecol 51: 3-6.
- Hasegawa J, Higashi M, Takahashi S, Mimura T, Nakamura M, et al. (2011) Can ultrasonography of the placenta previa predict antenatal bleeding? J Clin Ultrasound 39: 458-462.
- Shin JE, Shin JC, Lee Y, Kim SJ (2016) Serial change in cervical length for the prediction of emergency cesarean section in placenta previa. PLoS 11: e0149036.
- Zaitoun MM, El-Behery MM, El-Hameed AAA, Soliman BS (2011) Does cervical length and the lower placental edge thickness measurement correlates with clinical outcome in cases of complete placenta previa? Arch Gynecol Obstet 284: 867-873.
Citation: Cho H (2017) The Risk Factors for Antenatal Bleeding in Pregnancy with Placenta Previa. J Preg Child Health 4: 362. DOI: 10.4172/2376-127X.1000362
Copyright: ©2017 Cho H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6947
- [From(publication date): 0-2017 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 6166
- PDF downloads: 781