Research Article Open Access
The Retro-Cerebellar Arachnoidal Cyst: Prognosis and Literature Review
Bagnan JAT1, Aboubakar F1, Olatoundji Z1, Latoundji C1, Obossou AAA2*, Salifou K2, Hounkponou ANF2, Sidi IR2, Vodouhe MM2 and Perrin RX11Department for Mother and Child Care, Faculty of Health Sciences of the University of Abomey-Calavi, Bénin
2Department for Mother and Child Care, Faculty of Medicine, University of Parakou, Benin
- Corresponding Author:
- Awadé Afoukou Achille Obossou
Department for Mother and Child Care
Faculty of Medicine, University of Parakou, Bénin
Tel: 22995853279
E-mail: awadefr2000@yahoo.fr
Received date: May 26, 2017; Accepted date: May 29, 2017; Published date: May 31, 2017
Citation: Bagnan JAT, Aboubakar F, Olatoundji Z, Latoundji C, Obossou AAA, et al. (2017) The Retro-Cerebellar Arachnoidal Cyst: Prognosis and Literature Review. J Preg Child Health 4:330. doi:10.4172/2376-127X.1000330
Copyright: © 2017 Bagnan JAT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Arachnoid cysts are collections of cerebrospinal fluid developed within the arachnoid. The arachnoid cyst of the posterior fossa is sometimes responsible for neurological, motor, severe and irreversible disorders. We report a case of an arachnoid retro cerebellar cyst’s antenatal diagnosis on a fetus during an ultrasound performed at 33 WG and confirmed by a MRI at day of life. Treatment consisted of ventriculoperitoneal Shunt at six months of life with immediate decrease of the cyst volume. The eleven-month control found a complete resorption of the arachnoid cyst but a minor psychomotor retardation. It results that the prognosis is mainly related to the presence of associated lesions whose research requires the availability of magnetic resonance imaging.
Keywords
Retro-cerebellar arachnoid cyst; Antenatal diagnosis; Magnetic resonance imaging
Introduction
Arachnoidal cysts, collections of cerebrospinal fluid developed inside the arachnoid, represent the most common cerebral malformation [1]. A retrospective study among 1000 asymptomatic healthy adult volunteers reveals an incidence of 3/1000 [2]. In children, two thirds of arachnoidal cysts are located in the sylvian fissure (lateral cerebral sulcus) but the location in the posterior fossa seems less common [3].
The arachnoidal cyst of the posterior fossa can sometimes cause neurological motor, severe and irreversible disorders. The antenatal diagnosis of an arachnoidal cyst can therefore lead to a medical termination of pregnancy requested by the couple or advised by the doctor. The absence of the diagnosis of an arachnoidal cyst of the posterior fossa raises the issue of the management of the fetus or even the new-born baby. We report a case of a retro-cerebellar arachnoidal cyst in a patient aged 34 during an antenatal diagnosis.
Framework and Method
The case in question was monitored over a period of 17 months from 27 March 2015 to 10 September 2016. A sonographer we refer to in private practice in Cotonou, Benin carried out the antenatal diagnosis. The management and the monitoring after the delivery were performed by the Hôpitald’Instruction des Armées in Cotonou in collaboration with Pierre Wertheimer Hospital in Lyon, France.
Clinical Case
The patient is Mrs. X, aged 34 monitored in prenatal consultation. She is pregnant for the third time and has given birth for the second time. She had her first pregnancy in 2005. It evolved in unremarkable condition and led to a full term delivery of a live and healthy female sex baby. After a seven year secondary infertility, she got pregnant again in 2012 and had a spontaneous abortion at two months of pregnancy. She got her third pregnancy in 2015. The last menstrual period was not known.
The parents are not consanguineous. The father is 37 years old and he is healthy. The ultrasound dating has shown a mono fetal pregnancy of 9 weeks and 2 days amenorrhea with a craniocaudal length of 26.5 mm.
At the beginning of the pregnancy, the biological check-up is unremarkable, the mother being protected against rubella and toxoplasmosis. HIV status and syphilis serology are negative. No stigma of hepatitis B and C is found.
The pregnancy monitoring has been regular with 5 prenatal consultations, 3 doses of intermittent preventive anti-malarial treatment, 2 doses of tetanus vaccine.
Ultrasounds done at 20 and 26 weeks amenorrhea have shown a good fetal vitality with no morphological anomaly seen.
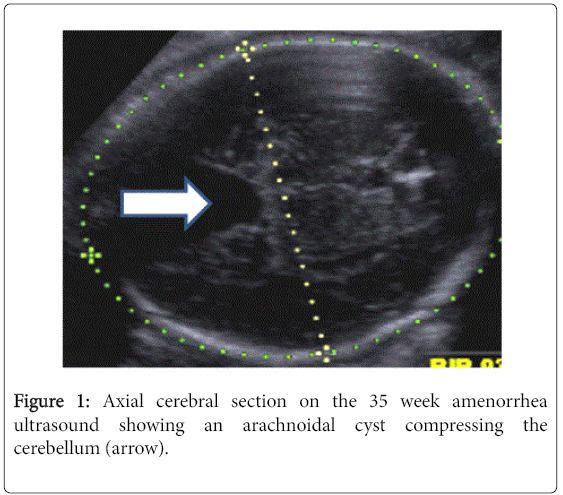
The ultrasound at 32 weeks amenorrhea has disclosed a large fluid image of the posterior fossa accounting for the prescription of an ultrasound by a sonographer we refer to. It is carried out at 35 weeks amenorrhea and has revealed a retro-cerebellar arachnoidal cyst (Figure 1). Furthermore, the fetus had a good vitality. The amount of amniotic fluid was normal and biometrics was in accordance with gestational age, close to 80th percentile for all measurements.
A fetal MRI was carried out, but was inconclusive because of the presence of numerous artefacts due to fetal mobility. The pregnant woman vaginally delivered a female sex baby crying immediately after 37 weeks and 1 day amenorrhea. The neurological examination of the new born baby was normal.
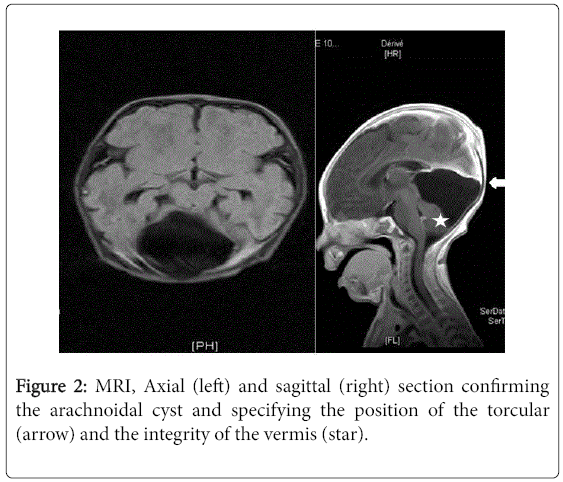
An MRI performed at the 8th Day (Figure 2) of life brings forward:
A sus and retro-cerebellar large fluid formation.
Contrasting with a cerebellar hypotrophy.
Compression of the cerebellum with no sign of engagement.
There is neither hydrocephaly nor brain localization.
The examination at two weeks of life makes it possible to notice
The absence of hint of convulsion.
The absence of other neurological warning signs.
The general condition is good.
The absence of scalp anomaly.
The weight is 2,950 g, the size is 48 cm and the HC is 35 cm.
The neurological exam aims at:
- The absence of intracranial hypertension signs.
- Primitive reflexes are present and symmetric.
An evacuation on health grounds for a surgical management was carried out at six months to Pierre Wertheimer Neurological and Neurosurgical Hospital in Lyon. The diagnosis of obstructive hydrocephalus by the arachnoidal cyst of the posterior fossa was made.
A surgical treatment by aventriculo-peritoneal shunt valve was carried out.
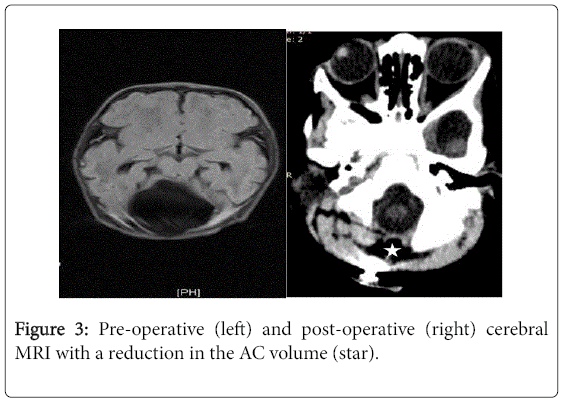
The post-operative MRI at six months showed a reduction in the arachnoidal cyst volume (Figure 3). The neurological examination at 11 months revealed discreet psychomotor development retardation. However, the prognosis was good as for the continuation of the psychomotor development. Monitoring, which was previously done half-yearly, would be annual from now on. The MRI at 11 months showed a total resorption of the retro cerebellar arachnoidal cyst.
Discussion
Antenatally, the malformations of the posterior fossa are detected by ultrasound, most often because of a fluid anomaly of the posterior fossa [1,2]. The MRI must show at 25 weeks amenorrhea the anatomical disposition of the final posterior fossa [3]. It is now routinely and ideally carried out by the 30thweek amenorrhea. Cysts are often suspected and diagnosed antenatally by means of obstetrical ultrasound and, for many years the fetal MRI has enabled to go forward in the diagnosis [4].
In this patient’s case, the ultrasound diagnosis was performed late and done at 35 weeks amenorrhea, confirmed by the MRI performed at 8 days of neonatal life. The MRI performed antenatally was not conclusive either. The belated discovery could be accounted for by the lack of experience of the former sonographer, the performance of the ultrasound machine or the small size of the lesion during the ultrasounds of the 2nd quarter. Furthermore, the difficulties faced during the fetal MRI were also a cause of delay in the diagnosis.
We traced during our clinical observation a retro cerebellar, median arachnoidal cyst of the posterior fossa with a compression of the cerebellum. In children, two thirds of arachnoidal cysts are located in the sylvian fissure (lateral cerebral sulcus) and those of the posterior fossa seem less common [5]. The predominance of the supratentorial localization is found in Pierre-Kahn et al.’s study including 54 fetuses but the majority of them being interhemispheric arachnoidal cysts. Twenty-two percent of arachnoidal cysts were found in the posterior fossa [6].
The cerebellar hypotrophy associated is in the case of our patient the only sign which does not form part of the classical signs of arachnoidal cysts. The arachnoidal cyst is an anechoic mass with no vascularization in color Doppler ultrasound. Generally single but can be polylobed, median or lateralized, with sharp and geometrical contours, it is sometimes bulky with a mass effect raising the tentorium cerebelli, distorting the cerebellar hemispheres (but without compressing them really) and may lead to hydrocephalus.
The cerebellar vermis is normal. Apart from a compressive process, the FV (Fourth Ventricle) has a normal appearance [7].
In literature, five clinical cases [8-11] describe the outcomes of patients who have an arachnoidal cyst discovered antenatally. In four cases out of five, the child has a normal development, with follow-up times ranging from six months to three years. The prognosis of retro cerebellar arachnoidal cyst is generally considered as good in literature [10].
However, it seems that we must be more prudent due to the presence of an AC of the posterior fossa than that of a sus-tentorial AC as far as the neurodevelopmental prognosis is concerned. The anteand post-natal evolution of arachnoidal cysts whose discovery is antenatal is characterized by an increase in the volume of the arachnoidal cyst and the appearance of hydrocephalus which may occur at any time.
In our case:
The inconclusive MRI antenally did not allow an opinion on the presence or not of cerebral damage associated which may cause to guard the antenatal prognosis. However, it was considered relatively favorable on account of the absence of hydrocephalus in spite of a bulky arachnoidal cyst.
The prognosis was somewhat tempered in the antenatal period due to the identification by the MRI performed at 8 days of life, of a cerebellar hypotrophy. However, literature review underlines the difficulty, even with an MRI to confirm a cerebellar hypotrophy because, to distinguish between compression and cerebellar hypoplasia may be sometimes very difficult [8].
For our patient, the antenatal evolution was unremarkable despite a relatively belated diagnosis and the prognosis was favourable on account of the absence of hydrocephalus and despite a bulky arachnoidal cyst.
But between six and nine months, the neurological examination revealed a slight retardation in psychomotor development which accounted for the establishment of physiotherapy.
As far as the therapeutic approach is concerned, no approach is accepted unanimously. If it is now acknowledged by everyone that surgery must only be performed for symptomatic cysts and that no treatment must be offered for asymptomatic cysts unexpectedly discovered, even if they have a large volume, the therapy offered comprises two main options:
• Exeresis with resection of cyst walls.
• Fluid shunt of the cyst.
• This therapy also depends on the location of the arachnoidal cyst.
In our case the child benefitted from a ventriculo peritoneal shunt. The immediate post-operative MRI performed showed reduction in the cystic volume and the other one performed during examination five months after surgery, showed a total resorption of the arachnoidal cyst. Furthermore, the neurological exam done concurrently with the MRI during the examination revealed an improvement of the psychomotor development but persistence was slightly late. Faced with a retro cerebellar AC, surgical treatment is considered necessary due to the large volume and the presence of clinical signs [9] and the prognosis is usually good after surgical shunt [7]. These data are in accordance with our observation. The surgical indication and the technique used are in conformity with those described in literature [11].
Conclusion
The retro cerebellar arachnoidal cyst is an unusual disease whose antenatal discovery makes it difficult to give enlightened information to parents. We must mention that in the ultrasound, before a fluid image of the posterior fossa, the MRI is essential to confirm the diagnosis and seek for associated cerebral damage. The prognosis, although considered as generally good in literature, is closely related to its volume but especially to the presence of cerebral damage associated, sources of important disorders of the psychomotor development.
References
- Bromley B, Nadel AS, Pauker S (1994) Closure of the cerebellar vermis: Evaluation with second trimerster US. Radiology 193: 761-763.
- Laing FC, Frates MC, Brown DL (1994) Sonography of the fetal posterior fossa: False appearence of mega-cisterna magna and Dandy Walker variant. Radiology 192: 247-251.
- Garel C (2000) The development of the fetal brain, Atlas MRI and biometrics. Sauramps Medical Montpellier.
- Whitby EH, Paley MN, Sprigg A, Rutter S, Davies NP, et al. (2004) Comparison of ultrasound and magnetic resonance imaging in 100 singleton pregnancies with suspected brain abnormalities. BJOG 111: 784-792.
- Osalakkal JA (2002) Intracranial arachnoid cysts in children: A review of pathogenesis, clinical features and management. Pediatr Neurol 26: 93-98.
- Pierre-Kahn A, Hanlo P, Sonigo P, Parisot D, McConnel RS (2000) The contribution of prenatal diagnosis to the understanding of malformative intracranial cysts: State of the art. Child NervSyst 16: 619-626.
- Bourgeot P, Masgenêt GB, Robert Y (2014) Véronique Houfflin-Debarge Yves Ardaensécho Ultrasound in obstetric practice. Elsevier Masson, p: 327.
- Camus HL (2010) Becoming children with an arachnoid cyst for antenatal diagnosis. J Radiol 91: 1129-1134.
- Paladini D, Volpe P(2007) Ultrasound of congenital fetal anomalies, Differential Diagnosis and Prognostic Indicators. UK Informa, p: 37.
- Adamsbaum C (2002) Antenatal diagnosis of anomalies isolated from the posterior fossa: an attempt at a simplified approach. J Radiol 88: 321-328.
- Peter JC, Fieggen G (1999) Congenital malformations of the brain – a neurosurgical perspective at the close of the twentieth century. Childs Nerv Sys 15: 635-645.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 10845
- [From(publication date):
June-2017 - Dec 18, 2024] - Breakdown by view type
- HTML page views : 10012
- PDF downloads : 833