Research Article Open Access
The Reality of Patients Requiring Prolonged Mechanical Ventilation: A Retrospective Multicenter Cohort Study
Sérgio Henrique Loss1, Roselaine Pinheiro de Oliveira2,3,6, Juçara Gasparetto Maccari2,4, Augusto Savi2, Marcio Manozzo Boniatti1, Márcio Pereira Hetzel3, Daniele Munaretto Dallegrave3, Patrícia de Campos Balzano1, Eubrando Silvestre Oliveira1, Jorge Amilton Höher3,5, André Peretti Torelly4 and Cassiano Teixeira2,3,5*1Department of Critical Care, Mãe de Deus Hospital, Brazil
2Department of Critical Care, Moinhos de Vento Hospital, Brazil
3Department of Critical Care, Central ICU of Santa Casa Hospital, Brazil
4Department of Critical Care, Santa Rita ICU of Santa Casa Hospital, Brazil
5Federal University of Health Sciences of Porto Alegre, Brazil
6University of Santa Cruz do Sul, Brazil
- *Corresponding Author:
- Cassiano Teixeira
Riveira, 355/403
Porto Alegre, RS-Brasil
Zip-Code: 90670-160
Tel: +55 (51) 3312.2608
E-mail: cassiano.rush@gmail.com
Received date: May 20, 2014; Accepted date: September 28, 2014; Published date: October 6, 2014
Citation: Loss HS, de Oliveira RP, Maccari JG, Savi A, Boniatti MM et al. (2014) The Reality of Patients Requiring Prolonged Mechanical Ventilation: A Retrospective Multicenter Cohort Study. J Palliat Care Med 4:192. doi:10.4172/2165-7386.1000192
Copyright: © 2014 Loss HS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Context: The number of patients requiring prolonged mechanical ventilation (PMV) has increased over the last decade, generating a large population of chronically ill patients. Objective: To establish the incidence of PMV in four Intensive Care Units (ICUs), and to report different characteristics, hospital outcomes, and the impact of costs and services of PMV patients (mechanical ventilation dependency = 21 days) compared with non-PMV patients (mechanical ventilation dependency < 21 days). Design, Setting, and Patients: A retrospective multicenter cohort study, including all patients admitted to four ICUs. Main Outcome Measures: Length of stay in the ICU, hospital, complications during ICU stay, and ICU and hospital mortality. Results: During study period, there were 5,287 admission episodes to the ICUs. Forty-one point five percent of these patients needed ventilatory support (n=2,197), and 218 met criteria for PMV (9.9%). Some complications developed during ICU stay, such as muscle weakness, pressure ulcers, bacterial nosocomial sepsis, candidemia, pulmonary embolism, and hyperactive delirium, were associated with a significantly higher risk of PMV. PMV patients had a significant increase in ICU mortality (absolute difference=14.2%, p<0.001), and in hospital mortality (absolute difference=19.1%, p<0.001); PMV group spent more days in the hospital after ICU discharge (26.9 ± 29.3 vs. 10.3 ± 20.4, p<0.001) and with higher costs. Conclusions: the classification of chronically critically ill patients according to the definition of PMV adopted by our study (mechanical ventilation dependency =21 days) identified patients with high risk for complications during ICU stay, high ICU and hospital stay, high death rates, as well as higher costs.
Keywords
Prolonged mechanical ventilation; Prognosis; Mortality
Introduction
The advances in intensive care have enabled more patients to survive an acute critical illness. However, these advances have also created a large and growing population of patients with prolonged dependence on mechanical ventilation (MV) and other intensive care therapies [1-3]. Most patients require short periods of respiratory support, but a minority requires prolonged MV (PMV), which has been defined as a period of 21 days for =6 hours/day on MV [4]. The requirement for a period of MV usually mandates admission to an ICU, and PMV is included in the term ‘‘chronically critically ill’’ described in a 1985 study by Girard and Raffin et al. that focused on patients who survived an initial episode of critical illness but remained dependent on intensive care; in other words, they were patients who neither died in the acute period of intensive care unit (ICU) treatment nor recovered [5].
The hallmark of chronic critical illness (CCI) is respiratory failure requiring prolonged dependence on MV, and the number of patients requiring ventilatory support is predicted to increase, in particular those who are elderly or with comorbidities (e.g., chronic obstructive pulmonary disease [COPD], cancer and sepsis), leading to a likely increase in the incidence of PMV [6]. CCI is a devastating condition for patients, their families, and for the health care system as a whole [3,6-8]. Trends in the numbers of patients requiring PMV are of interest to health service planners because they consume a disproportionate amount of health care resources, and have high illness costs [9-11].
The heterogeneous available data on patient outcomes and CCI definitions indicate considerable variations between the populations studied [12]. Single-center studies [6,13-17] indicate that approximately 3 to 11% of patients receiving MV meet the criteria for ventilatory dependency for more than 21 days; nevertheless, multicenter studies using this stricter definition of PMV have not been performed until now [18]. Therefore, the aim of this cohort study is to establish the incidence of PMV in four ICUs, and to report different characteristics, hospital outcomes, and the impact of costs and services of PMV patients (MV dependency = 21 days) compared with non-PMV patients (MV dependency <21 days).
Patients and Methods
Design
We performed a retrospective cohort study using an ICU database prospectively and routinely collected by ICU staff of four institutions. The Research Ethics Committees of four institutions waived the need for formal ethical review. Patient confidentiality was ensured as the dataset was fully anonymized.
Setting
Each hospital has a “closed” adult general mixed medical/surgical ICU with specialist intensive care staff. The number of ICU beds included in this study was 93 (ICU-1 [Moinhos de Vento Hospital – 31 beds], ICU-2 [Central-ICU of Santa Casa Hospital – 18 beds], ICU-3 [Santa Rita Hospital – 10 beds], and ICU-4 [Mãe de Deus Hospital – 34 beds]), and data were collected during 26 months [Apr-2008 to Jun-2010]
Database
All data were entered prospectively by clinical staff and include demographics (gender, age, body mass index [BMI]); cause of ICU admission; admission source; disease severity scores (Acute Physiology and Chronic Health Evaluation [APACHE] II scoring at 24 h, and Sepsis-related Organ Failure Assessment [SOFA], Therapeutic Intervention Scoring System [TISS], and Glasgow Coma Score [GCS] at admission and at discharge); documented preexisting chronic diseases and severity of underlying medical conditions were recorded and classified by Charlson Index, number of comorbidities, and McCabe score (as nonfatal - score 1, ultimately fatal - score 2, or fatal - score 3]; presence of infection, sepsis. Organ support data during ICU stay (e.g. renal replacement therapy [RRT], vasoactive therapy, and need for parenteral nutrition), and need for unscheduled surgery or tracheotomy were entered on a daily basis during an admission episode. Complications during ICU hospitalization, ICU length of stay (LOS), hospital LOS, days on MV, survival status at ICU and at hospital discharge were also recorded.
During the follow-up, all patients on MV received respiratory and motor physiotherapy. All units used daily interruption of sedation and weaning protocol based on tolerance at spontaneous breathing trial. Tracheotomy was performed according to the attending physician. Non-invasive ventilation was available in all units. RRT in the four units could be performed by continuous hemofiltration or intermittent hemodialysis in more stable patients.
We calculated an average daily cost per capita in a sample of patients (non-PMV=425 and PMV=28) for evaluation of resource utilization. The obtained value was multiplied by ICU LOS (ICU cost) and hospital LOS (hospital cost).
Statistical analysis
Patient characteristics were presented as number and percentage, mean and standard deviation (SD). Characteristics were described for PMV and non-PMV groups, and compared with the following tests: t-test for normally distributed data, Mann-Whitney U test for non-normally distributed data, and chi-squared test for categorical variables. Trends were analyzed using chi-squared test for categorical variables. The association between PMV status and diagnostic category was assessed using odds ratio (OR). A multivariate analysis was performed to determine the risk factors for evolution to chronic critical illness using backward stepwise multiple logistic regression. Factors with a value of p = 0.01 (as determined by a univariate analysis) were selected for the model. Confidence intervals (CI) for incidence rates were derived using the Poisson distribution. A significance level of 1% was used for analyses and 95% CI were presented (unless stated). All analyses were undertaken using SPSS v18.
Results
During study period, there were 5,287 admission episodes to the four ICUs (ICU1=3,345, ICU2=603, ICU3=886, and ICU4=453). Readmissions were excluded from the analysis. Forty-one point five percent of these patients needed ventilatory support (n=2,197), and 218 (9.9%) met criteria for PMV (ICU1=112, ICU2=40, ICU3=38, and ICU4=28). Baseline characteristics of patients are showed in Table 1.
| Characteristic | PMV (n=218) | Non-PMV (n=1,979) | P | OR (95% CI) |
|---|---|---|---|---|
| Male gender (%) | 103 (47.2) | 1,088 (55) | 0.03 | 0.73 (0.55-0.97) |
| Age, years | 66.6±17.4 | 65.7±17.3 | ns | |
| Age group ≥65 years | 123 (56.4) | 1,163 (58.8) | ns | |
| BMI, Kg/m2 | 25.4±5.6 | 25.4±4.9 | ns | |
| At ICU admission | ||||
| Source (%) | ||||
| Ward | 78 (35.7) | 619 (31.3) | ns | |
| Emergency room | 56 (25.6) | 466 (23.5) | ns | |
| Operating room | 36 (16.5) | 543 (27.4) | <0.0001 | 0.52 (0.36-0.76) |
| Transfer | 26 (11.9) | 230 (11.6) | ns | |
| Others | 22 (10.3) | 121 (6.2) | ns | |
| Preexisting chronic diseases and severity of underlying medical conditions | ||||
| Comorbidities (%) | ||||
| Heart failure | 33 (15.1) | 264 (13.3) | ns | |
| COPD | 30 (16.9) | 241 (14.4) | ns | |
| End-stage renal failure | 8 (4.5) | 84 (5) | ns | |
| AIDS | 16 (7.3) | 89 (4.5) | ns | |
| Cancer | 79 (36.2) | 703 (35.5) | ns | |
| Peripheral vascular disease | 30 (13.8) | 227 (11.5) | ns | |
| Cirrhosis | 2 (1.6) | 34 (3.5) | ns | |
| Neuromuscular disease | 8 (6.6) | 37 (3.8) | ns | |
| Number of preexisting diseases (%) | ||||
| None | 65 (29.8) | 712 (26) | ns | |
| One | 109 (50) | 931 (47) | ns | |
| Two | 39 (17.9) | 288 (14.6) | ns | |
| More than two | 5 (2.3) | 48 (2.4) | ns | |
| Charlson index | 1.67±1.84 | 1.45±1.66 | ns | |
| McCabe score (%) | ||||
| 3 | 13 (8.6) | 88 (6.1) | ns | |
| 2 | 26 (17.1) | 172 (12) | ns | |
| 1 | 113 (74.3) | 1168 (81.6) | ns | |
| Reason for ICU admission (%) | ||||
| Surgical** | 41 (18.8) | 582 (29.4) | 0.001 | 0.54 (0.38-0.77) |
| Medical | 177 (81.2) | 1397 (70.6) | ||
| Respiratory | 90 (41.3) | 547 (27.6) | ns* | |
| Neurological | 39 (17.8) | 321 (16.2) | ns* | |
| Cardiovascular | 10 (4.6) | 212 (10.7) | ns* | |
| Trauma | 24 (11.1) | 162 (7.7) | ns* | |
| Gastrointestinal | 10 (4.6) | 114 (5.8) | ns* | |
| Renal | 4 (1.8) | 41 (2.1) | ns* | |
| Severity at ICU: day 1 | ||||
| APACHE II | 21.4±7.2 | 19.4±8.3 | ns | |
| GCS | 12.0±4.0 | 11.5±4.5 | ns | |
| SOFA | 5.3±3.7 | 5.1±3.5 | ns | |
| TISS | 26.5±7.4 | 26.1±7.8 | ns | |
| Presence of infection (%) | 134 (61.4) | 1004 (50.7) | <0.001 | 1.94 (1.40-2.69) |
| Diagnosis of severe sepsis (%) | 48 (22.0) | 354 (17.9) | 0.01 | 1.54 (1.07-2.21) |
| During ICU stay | ||||
| Organ support during ICU stay (%) | ||||
| Vasoactive drug use | 183 (83.9) | 1332 (67.3) | <0.001 | 2.54 (1.74-3.69) |
| RRT | 54 (24.8) | 235 (11.9) | <0.001 | 2.44 (1.74-3.42) |
| Parenteral nutrition support | 27 (12.4) | 131 (6.7) | 0.002 | 1.98 (1.27-3.07) |
| Tracheotomy need | 151 (69.2) | 168 (8.5) | <0.001 | 24.3 (17.4-33.7) |
| Need for unscheduled surgery | 62 (28.4) | 291 (14.7) | <0.001 | 2.3 (1.67-3.17) |
| DNR decision | 15 (6.9) | 138 (7.0) | ns | |
| At ICU discharge | ||||
| Severity at ICU discharge | ||||
| GCS | 13.5±2.52 | 14.2±1.79 | 0.01 | |
| SOFA | 3.01±4.03 | 2.64±4.18 | ns | |
| TISS | 10.8±11.07 | 10.6±10.12 | ns | |
| ICU death | 113 (51.8) | 744 (37.6) | <0.001 | 1.78 (1.35-2.36) |
| Hospital death | 142 (65) | 911 (44.9) | <0.001 | 2.23 (1.67-2.99) |
Table 1: Characteristics of the study subjects. *(Comparisons within group); **(not only at admission)
Comparison of PMV and non-PMV groups: at ICU admission
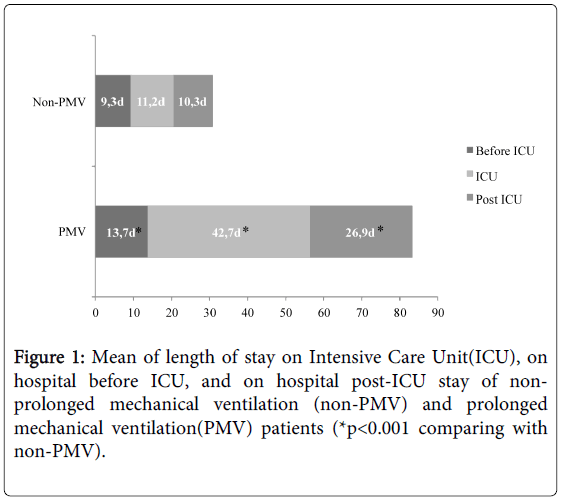
PMV patients were more likely to have ICU admissions for respiratory (41.3% vs. 27.6%, p<0.001) and infection (61.4% vs. 50.7%, p<0.001) causes (Table 1), and more prolonged hospital LOS before ICU admission (13.7 ± 44.3 days vs. 9.3 ± 21.6 days, p=0.01) (Figure 1). No difference was found in age, BMI, disease severity scores within 24 h of ICU admission, preexisting chronic diseases and severity of underlying medical con
Comparison of PMV and non-PMV groups: during ICU stay and at ICU discharge
PMV patients were more likely to receive organ support (vasoactive therapy [83.9% vs. 67.3%, p<0.001], RRT [24.8% vs. 11.9%, p<0.001] and parenteral nutrition [12.4% vs. 6.7%, p<0.001]), and underwent more unscheduled surgery (28.4 vs. 14.7%, p<0.001) and tracheotomy (69.2% vs. 8.5%, p<0.001) (Table 1).
Complications that developed during ICU stay, such as pressure ulcers (OR 9.18, 95%CI 6.64-12.7), muscle weakness (OR 6.99, 95% CI 4.94-9.82), infection (bacterial sepsis (OR 5.18, 95% CI 3.75-7.15), candidemia (OR 3.82, 95% CI 1.31-11.09) and pulmonary embolism (OR 3.71, 95% CI 1.43-9.63), were associated with a significantly higher risk of PMV (Table 2).
| Complications (%) | PMV (n=218) | Non-PMV (n=1979) | p | OR (95% CI) |
|---|---|---|---|---|
| Myocardial infarction | 5 (2.6) | 41 (2.3) | ns | |
| Cerebrovascular disease | 3 (2) | 37 (2.6) | ns | |
| Pulmonary embolism | 6 (5.4) | 17 (1.5) | 0.004 | 3.71 (1.43-9.63) |
| Muscle weakness | 71 (37.6) | 144 (7.9) | <0.001 | 6.99 (4.97-9.82) |
| ARDS | 37 (17.1) | 124 (6.3) | <0.001 | 3.07 (2.06-4.57) |
| Bacterial nosocomial sepsis | 129 (68.3) | 533 (29.3) | <0.001 | 5.18 (3.75-7.15) |
| Candidemia | 5 (5.4) | 12 (1.5) | 0.008 | 3.82 (1.31-11.09) |
| Upper gastrointestinal bleeding | 19 (10.1) | 59 (3.2) | <0.001 | 3.33 (1.94-5.71) |
| Hyperactive delirium | 27 (22.3) | 147 (15) | 0.03 | 1.62 (1.02-2.57) |
| Pressure ulcer | 86 (39.4) | 131 (6.6) | <0.001 | 9.18 (6.64-12.7) |
Table 2: Complications during ICU stay. (*p<0.001 comparing with non-PMV)
PMV patients spent more days in ICU (42.7 ± 25.9 vs. 11.2 ± 15.3, p<0.001), and in hospital after ICU discharge (26.9 ± 29.3 vs. 10.3 ± 20.4, p<0.001) than non-PMV patients (Figure 1). Prolonged MV patients had a significant increase in ICU mortality (absolute difference=14.2%, 95% CI 1.78 (1.35-2.36), p<0.001), and in hospital mortality (absolute difference=19.1%, 95% CI 2.23 (1.67-2.99), p<0.001) (Table 1).
Patterns of discharge from the ICU were worse in the PMV group, based on GCS evaluation (13.5 ± 2.52 vs. 14.2 ± 1.79, p=0.01).
The average daily cost per capita was US$737,00 for non-PMV and US$910,00 for PMV patients. As the length of stay was greater in the PMV group, their hospital cost was 3.3 times higher than non-PMV.
Discussion
In this analysis of a large, multicenter and retrospective cohort of MV patients, we found that patients who required PMV (MV support =21 days) had higher risk for complications during ICU stay, and higher death rates during ICU LOS and hospital LOS, as have high illness costs. It describes the first South American experience on the topic.
Between 3 to 10% of patients who require MV for acute conditions develop chronic critical illness [3,13-16]. Generalization of outcomes from published reports is complicated by variation in study populations described as CCI, in definitions of outcomes of interest, and in post-acute care practices that affect hospital use. A threshold period of MV, ranging from 2 to 30 days, has been used to define the majority of cohorts for longitudinal studies [8,18,19]. Martin et al. [7] evaluated patients requiring =10 days of MV, Combes et al. [20] studied the outcome and health-related quality of life of patients requiring =14 days of MV, while Carson et al. [21] and Cox et al. [22] evaluated the long-term prognosis of patients requiring =21 days of MV. To limit the heterogeneity of these cohorts and thereby improve comparability of outcomes across different studies, a consensus conference established a formal definition for PMV: at least 21 consecutive days on the ventilator for more than 6 hours/day [4]. Using this criterion, our data demonstrated 9.92% of CCI, varying according to the characteristics of patients in each ICU study (ICU1=8.8%; ICU2=12%; ICU3=9%; ICU4=15%). However, other authors have identified chronically critically ill patients by elective placement of a tracheotomy to facilitate prolonged ventilation and weaning efforts [14,22-25]. Referral for tracheotomy reflects the clinician’s judgment that the patient will neither wean nor die in the immediate future and, thus, provides a point of demarcation between acute and chronic critical illness that is both clinically meaningful and practical [26,27]. Cox et al. [22] revealed that these two suggested definitions for PMV, Diagnosis-Related Groups (DRGs) 541/542 (Medicare's definition: tracheotomy and MV =96 hours), and MV =21 days, select cohorts with similar baseline clinical characteristics and trends in survival, disposition and resource utilization. However, PMV defined by ventilation for =21 days can identify more specifically patients who are outliers in resource consumption among ventilated patients, which is why we chose to analyze the patients based on this definition [3,4].
Physicians and scoring systems are inaccurate in predicting morbidity and mortality at the time of ICU admission [28]. However, it is important to identify patients with a high risk of becoming chronic early enough to be able to manage them. In our study, surprisingly, preexisting chronic diseases and severity of underlying medical conditions were not associated with CCI, as well as age, BMI and source of admitted patient (nevertheless, it seemed that operating room as source of admission was protective in our study). On the other hand, a longer hospital stay before ICU admission and non-surgical admission (OR 1.8 (1.26-2.56), p<0.001) were associated with the evolution to CCI. Admission of patients for nonsurgical reasons has been previously identified as a factor associated with the evolution to chronic critical illness [3,23]. The severity scores have been considered predictors of prolonged MV [3,17,23,29]. Our data, at admission, are not consistent with this assumption. However, the multi-organ involvement is also related with mortality and, recently, Carson et al. [21] developed the ProVent score (need for a vasopressor and hemodialysis, presence of thrombocytopenia, and age =50 years) and showed a good discriminatory power to predict mortality in PMV patients.
Regardless of the definition of PMV, the main characteristics of this population are repeated episodes of shock and infection during their stays in the ICU [6]. This condition has been associated to persistent inflammation, immunosuppression and catabolism syndrome, or PICS – Persistent inflammation and catabolism syndrome [30]. Thus, CCI cannot simply be seen as an extension of an acute critical illness but, rather, as a complex syndrome characterized by metabolic, neuroendocrine, neuropsychiatric and immunological changes [3,31]. These include profound weakness attributed to myopathy, neuropathy, and alterations of body composition (loss of lean body mass, increased adiposity, and anasarca) [32]; increased vulnerability to infection, often with multi-resistant microbial organisms [33], brain dysfunction (coma or delirium) [34], neuroendocrine changes (loss of pulsatile secretion of anterior pituitary hormones, contributing to low target organ hormone levels and impaired anabolism) [35] and skin breakdown (pressure ulcers) [36]. Some of these conditions were evaluated and confirmed by our study (Tables 1 and 2).
Previous authors have found higher mortality in PMV patients [7,17,20,22,23], while others have not [6,22]. The reason for these discrepancies is probably related to the heterogeneity and intrinsic characteristics of studies' populations. However, it can be easily observed in most studies that CCI and PMV patients have worse courses and higher mortality. In our study, the ICU and hospital mortality in PMV patients was respectively 14.2% and 19.1%, absolutely higher than non-PMV patients.
The critical ill survivors have an ongoing morbidity, and actual evidence suggests that quality of life after intensive care admission is generally poor when compared to population data [36]. These morbidities include high incidence of psychological problems [37], cognitive dysfunction [38], impairments in pulmonary function [39], and development of neuromuscular complications of critical illness [40], which, in spite of a slow improvement over time, may be long-lasting. These problems are more incidents in chronic critical patients, and the need for PMV may also affect patient’s prognosis of the ability to perform activities of daily living [20]. According to some authors, 5% to 20% of ICU patients receive MV, and 25% of these require MV for more than seven days [41]. Nearly all patients with CCI leave the hospital with profound impairments of physical function, cognitive status, or both, and most of them, therefore, require institutional care [42]. In this scenario, identifying the predictors of a poor prognosis might help doctors choose more aggressive treatments or treatments that prioritize comfort [3,4]. In ICU’s where this study was conducted, PMV patients neither were grouped into dedicated care environments within the ICU (for reduced nurse to patient ratio) nor provided with focused care plans to better meet their needs (physiotherapy, respiratory therapy).
CCI is growing and becoming a serious problem for the health care system in many countries [3]. Although the CCI accounts for fewer than 10% of those receiving MV, they consume 20 to 40% of ICU bed-days and other critical care resources [16,27]. In our study, PMV patients represent 10% of all ICU admissions and 71% of total cost of all ICU admissions during the study period. This means that, according to our study, the PMV patients had a cost of more than three times that of non-PMV patients. The overall cost to the health care system for the management of CCI already exceeds an estimated $20 billion per year and is expected to climb with increases in the incidence of this syndrome and in overall expenditures for critical care, which nearly doubled between 1985 and 2000 and represent 13% of all hospital costs in the United States [2].
This study has a few limitations. It's a retrospective observational study, without long-term outcomes, such as evaluation of quality of life and cognitive impair. All PMV is a group of more than 21 days on MV, whereas non-PMV is a heterogeneous group of variation in total number until 20 MV days. However, the study brings an important contribution because it a large patient sample obtained from various centers and the utilization of a uniform definition. Moreover, it is the first study that evaluates the incidence and outcome of these patients in South America.
In our study, patients with CCI constituted a distinct group of patients with higher mortality, longer hospital stay and higher costs. Patients in respiratory failure, who, at admission, present a period of pre-ICU hospitalization longer than 12 days, are non-surgical and have sepsis, have a higher risk to become dependent on prolonged mechanical ventilation support.
References
- Girard K, Raffin TA (1985) The chronically critically ill: to save or let die? Respir Care 30: 339-347.
- Halpern NA, Pastores SM, Greenstein RJ (2004) Critical care medicine in the United States 1985-2000: an analysis of bed numbers, use, and costs. Crit Care Med 32: 1254-1259.
- Nelson JE, Cox CE, Hope AA, Carson SS (2010) Chronic critical illness. Am J RespirCrit Care Med 182: 446-454.
- MacIntyre NR, Epstein SK, Carson S, Scheinhorn D, Christopher K, et al. (2005) Management of patients requiring prolonged mechanical ventilation: report of a NAMDRC consensus conference. Chest 128: 3937-3954.
- Zilberberg MD, de Wit M, Pirone JR, Shorr AF (2008) Growth in adult prolonged acute mechanical ventilation: implications for healthcare delivery. Crit Care Med 36: 1451-1455.
- Estenssoro E, Reina R, Canales HS, Saenz MG, Gonzalez FE, et al. (2006) The distinct clinical profile of chronically critically ill patients: a cohort study. Crit Care 10: R89.
- Martin CM, Hill AD, Burns K, Chen LM (2005) Characteristics and outcomes for critically ill patients with prolonged intensive care unit stays. Crit Care Med 33: 1922-1927.
- Daly BJ, Douglas SL, Kelley CG, O'toole E, Montenegro H (2005) Trial of a disease management program to reduce hospital readmissions of the chronically critically ill. Chest 128: 507-517.
- Robson V, Poynter J, Lawler PG, Baudouin SV (2003) The need for a regional weaning centre, a one-year survey of intensive care weaning delay in the Northern Region of England. Anaesthesia 58: 161-165.
- Zilberberg MD, Luippold RS, Sulsky S, Shorr AF (2008) Prolonged acute mechanical ventilation, hospital resource utilization, and mortality in the United States. Crit Care Med 36: 724-730.
- Kahn JM, Benson NM, Appleby D, Carson SS, Iwashyna TJ (2010) Long-term acute care hospital utilization after critical illness. JAMA 303: 2253-2259.
- Mauri T, Pivi S, Bigatello LM (2008) Prolonged mechanical ventilation after critical illness. Minerva Anestesiol 74: 297-301.
- Gracey DR, Viggiano RW, Naessens JM, Hubmayr RD, Silverstein MD, et al. (1992) Outcomes of patients admitted to a chronic ventilator-dependent unit in an acute-care hospital. Mayo ClinProc 67: 131-136.
- Engoren M, Arslanian-Engoren C, Fenn-Buderer N (2004) Hospital and long-term outcome after tracheostomy for respiratory failure. Chest 125: 220-227.
- Seneff MG, Zimmerman JE, Knaus WA, Wagner DP, Draper EA (1996) Predicting the duration of mechanical ventilation. The importance of disease and patient characteristics. Chest 110: 469-479.
- Wagner DP (1989) Economics of prolonged mechanical ventilation. Am Rev Respir Dis 140: S14-18.
- Loss SH, Marchese CB, Boniatti MM, Wawrzeniak IC, Oliveira RP, et al. (2013) Prediction of chronic critical illness in a general intensive care unit. Rev Assoc Med Bras 59: 241-247.
- Chelluri L, Im KA, Belle SH, Schulz R, Rotondi AJ, et al. (2004) Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med 32: 61-69.
- Gracey DR, Naessens JM, Krishan I, Marsh HM (1992) Hospital and posthospital survival in patients mechanically ventilated for more than 29 days. Chest 101: 211-214.
- Combes A, Costa MA, Trouillet JL, Baudot J, Mokhtari M, et al. (2003) Morbidity, mortality, and quality-of-life outcomes of patients requiring >or=14 days of mechanical ventilation. Crit Care Med 31: 1373-1381.
- Carson SS, Garrett J, Hanson LC, Lanier J, Govert J, et al. (2008) A prognostic model for one-year mortality in patients requiring prolonged mechanical ventilation. Crit Care Med 36: 2061-2069.
- Cox CE, Carson SS, Lindquist JH, Olsen MK, Govert JA, et al. (2007) Differences in one-year health outcomes and resource utilization by definition of prolonged mechanical ventilation: a prospective cohort study. Crit Care 11: R9.
- Boniatti MM, Friedman G, Castilho RK, Vieira SR, Fialkow L (2011) Characteristics of chronically critically ill patients: comparing two definitions. Clinics (Sao Paulo) 66: 701-704.
- Carson SS, Bach PB, Brzozowski L, Leff A (1999) Outcomes after long-term acute care. An analysis of 133 mechanically ventilated patients. Am J RespirCrit Care Med 159: 1568-1573.
- Engoren M, Arslanian-Engoren C (2005) Hospital and long-term outcome of trauma patients with tracheostomy for respiratory failure. Am Surg 71: 123-127.
- Kahn JM, Carson SS, Angus DC, Linde-Zwirble WT, Iwashyna TJ (2009) Development and validation of an algorithm for identifying prolonged mechanical ventilation in administrative data. Health Serv Outcomes Res Method;9:117-132.
- Cox CE, Carson SS, Holmes GM, Howard A, Carey TS (2004) Increase in tracheostomy for prolonged mechanical ventilation in North Carolina, 1993-2002. Crit Care Med 32: 2219-2226.
- Sinuff T, Adhikari NK, Cook DJ, Schünemann HJ, Griffith LE, et al. (2006) Mortality predictions in the intensive care unit: comparing physicians with scoring systems. Crit Care Med 34: 878-885.
- Honarmand A, Safavi M, Moradi D (2009) The use of infection probability score and sequential organ failure assessment scoring systems in predicting mechanical ventilation requirement and duration. UlusTravmaAcilCerrahiDerg;15:440-447.
- Gentile LF, Cuenca AG, Efron PA, Ang D, Bihorac A, et al. (2012) Persistent inflammation and immunosuppression: a common syndrome and new horizon for surgical intensive care. J Trauma Acute Care Surg 72: 1491-1501.
- Nierman DM (2002) A structure of care for the chronically critically ill. Crit Care Clin 18: 477-491.
- Hollander JM, Mechanick JI (2006) Nutrition support and the chronic critical illness syndrome. NutrClinPract 21: 587-604.
- Kalb TH, Lorin S (2002) Infection in the chronically critically ill: unique risk profile in a newly defined population. Crit Care Clin 18: 529-552.
- Nelson JE, Tandon N, Mercado AF, Camhi SL, Ely EW, et al. (2006) Brain dysfunction: another burden for the chronically critically ill. Arch Intern Med 166: 1993-1999.
- Van den Berghe G, de Zegher F, Veldhuis JD, Wouters P, Awouters M, et al. (1997) The somatotropic axis in critical illness: effect of continuous growth hormone (GH)-releasing hormone and GH-releasing peptide-2 infusion. J ClinEndocrinolMetab 82: 590-599.
- Carasa M, Polycarpe M (2004) Caring for the chronically critically ill patient: establishing a wound- healing program in a respiratory care unit. Am J Surg 188: 18-21.
- Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, et al. (2005) Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J RespirCrit Care Med 171: 987-994.
- Hopkins RO, Jackson JC (2006) Long-term neurocognitive function after critical illness. Chest 130: 869-878.
- Quinnell TG, Pilsworth S, Shneerson JM, Smith IE (2006) Prolonged invasive ventilation following acute ventilatory failure in COPD: weaning results, survival, and the role of noninvasive ventilation. Chest;129:133-9.
- Hough CL (2006) Neuromuscular sequelae in survivors of acute lung injury. Clin Chest Med 27: 691-703.
- Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, et al. (2002) Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 287: 345-355.
- Rimachi R, Vincent JL, Brimioulle S (2007) Survival and quality of life after prolonged intensive care unit stay. Anaesth Intensive Care 35: 62-67.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 14217
- [From(publication date):
November-2014 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 9619
- PDF downloads : 4598