Research Letter Open Access
The Ramifications of At-Own-Risk Discharges in the Palliative Care Setting
Alvona Zi Hui Loh1, Julia Shi Yu Tan1, Rukshini Puvanendran2, Sumytra Menon1, Ravindran Kanesvaran3 and Lalit Kumar Radha Krishna4*1Yong Loo Lin School of Medicine, National University of Singapore, Singapore
2KK Women’s and Children’s Hospital, Singapore
3Division of Medical Oncology, National Cancer Centre Singapore, Singapore
4Division of Palliative Medicine, National Cancer Centre Singapore, Singapore
- Corresponding Author:
- Krishna LKR
Senior consultant in Division of Palliative Medicine
National Cancer Centre Singapore, Singapore
Tel: +65 6436 8000
Fax: +65 6225 6283
E-mail: lalit.krishna@nccs.com.sg
Received Date: June 17, 2015 Accepted Date: June 30, 2015 Published Date: July 03, 2015
Citation: Loh AZH, Tan JS, Puvanendran R, Menon S, Kanesvaran R, et al. (2015) The Ramifications of At-Own-Risk Discharges in the Palliative Care Setting. J Palliat Care Med 5:224. doi:10.4172/2165-7386.1000224
Copyright: © 2015 Loh AZH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: The Principle of Respect for Autonomy is integral to the patient-physician relationship, yet within a society that prizes the value of life and remains defined by Confucian-inspired concepts of Beneficence, limits to respect for patient choice are increasingly apparent. This is particularly evident in the end-of-life setting and specifically in situations where terminally ill palliative care patients choose to leave health care institutions against medical advice potentially to the detriment of their health. Focusing on "discharges against medical advice" (DAMA), also known as "at own risk" (AOR) discharges within the palliative care inpatients setting, we highlight growing concerns on the AOR discharge process as it is practiced presently.
Methods: We used 3 patient case studies to highlight the various aspects of concern surrounding AOR discharges and its compromise of patient welfare, ostensibly as a result of compliance with the central tenets of the Principle of Autonomy and patient choice. To preserve the interests of the patient we propose the employment of Krishna, Lee and Watkinson’s Welfare Model (WM) which offers a more clinically relevant and ethically sensitive means to decision-making at the end of life within societies still inspired by Confucian beliefs and the Principle of Beneficence.
Results: Based on the WM, AOR discharges in palliative care may be viable if decisions to respect them adopt: (1) a humanistic and holistic approach, (2) patient specific decision-making method, (3) a multidisciplinary medical team approach, (4) clear documentation of the deliberation process, and (5) an evidence-based decision making process that is consistent with regnant professional, social, institutional, and legal standards.
Conclusion: Greater efforts need to be taken to pre-empt AOR discharges where possible among inpatients of palliative care or other medical disciplines. If an AOR discharge is unavoidable, a decision-making process defined by the WM provides the best means of protecting patient welfare and being consistent with prevailing socio-cultural beliefs and values.
Keywords
At-own-risk discharges; Discharge against medical advice; Palliative care; Palliative medicine; Cancer; Welfare; End-oflife
Introduction
Respect for patient choice is central to the patient-physician relationship and is exemplified by respecting the competent patient’s choice to end their therapeutic relationship with their physician and to act against medical advice even if it is potentially detrimental to their health [1]. This act of leaving a medical unit against the expressed advice of the medical team, i.e. without notification by escaping from an involuntary or voluntary unit, or after consultation with a medical team before assessment and/or treatment is completed has been variously referred to as “discharges against medical advice” (DAMA), also known as “at own risk” (AOR) discharge [1]. For palliative care inpatients who chose to leave a care facility after seeing a medical team, but before assessment and/or treatment is completed, we question the extent to which an AOR discharge should be respected under the aegis of a palliative care approach.
Within the Singapore setting where Confucius-inspired Beneficence dominates, the autonomous choices of patients are not placed above all other considerations, because contextual considerations should be accounted for [2]. Within the end-of-life setting, Tsai [2] suggests that Confucius' principles tend to grant "beneficence" a favourable position, therefore diminishing the significance of respect for individual rights and autonomy, which is diametrically opposite to the centrality of respect for autonomy and its stance of "first among equals" so pivotal to Western ethics. Yielding to the maintenance of patient welfare and potentially the preservation of life, in the event of a request for AOR discharge which could endanger the life of a frail and vulnerable terminally ill patient, is consistent with local social, cultural and legal practices.
The primacy of beneficence in the Singapore context
Singapore places a great emphasis on the value of life, as evidenced by e.g. (1) the outlawing of suicide [3], where the Penal Code Chapter 224, Chapter XVI Offences Affecting The Human Body states that whoever attempts to commit suicide, and does any act towards the commission of such offence, shall be punished with imprisonment for a term which may extend to one year, or with fine, or with both, and (2) the implementation of the policy of Advance Medical Directive (AMD) [4] which sets out to ensure that basic medical care is not routinely foregone ostensibly to hasten death. A welfare model backed by local socio-cultural beliefs and values thus validates the trumping of the Principle of Respect for Autonomy in favour of the Principle of Beneficence.
The practical assumptions underpinning utilisation of an AOR discharge
In the event of AOR discharge, a physician avoids the threat of professional negligence by meeting a number of basic obligations which include: (1) providing the patient appropriate information about his/her condition, (2) explaining current treatment options and (3) potential risks of treatment, (4) risks of non-compliance with medical advice, and (5) offering alternative treatment options.
Furthermore, the physician must try to ascertain that the patient has understood and cogitated upon this information, as well as clarified any areas of ambiguity in the information provided that may lead to gaps in comprehension. To facilitate this process, other medical staff may help to assess the patient’s competence.
These discussions should be appropriately documented, and the patient should acknowledge these facts by signing the AOR discharge form. Levy et al. [5] suggest that in addition to the steps detailed above, “a properly executed" AOR discharge form is required to provide limited protection from future liability. The AOR discharge form proposed consists of information on: (1) the termination of the legal duty to treat a patient, (2) the creation of the affirmative defense of "assumption of risk", and (3) the creation of record evidence of the patient’s refusal of care. To date, there are no relevant negligence cases on AOR discharges in Singapore or England.
However, the face of healthcare is evolving and rapidly embracing an integrated approach that sees all elements of medical care merging, to ensure safe and effective care transition between care settings. We believe that the emergence of multi-faceted and multi-disciplinary therapeutic relationships renders the solitary patient-physician relationship defunct. This implies that it is implausible to sever the therapeutic relationship between a patient and a physician through an AOR discharge in the palliative inpatient setting where different care and specialist multidisciplinary teams are often involved in the care of the patient, whether in the hospital or at the patient's home.
Therefore, severing a patient-physician relationship in one setting does not necessarily sever the relationships with other teams involved in the patient’s care. Furthermore, medicine has become increasingly team-based and professional relationships are created with doctors from a number of specialties.
Palliative care patients often have complex and multi-faceted medical needs managed by multi-professional, multi-disciplinary teams within a care unit. As a result, terminating a particular relationship with a specific physician does not protect the care unit from liability when other relationships are maintained through association with other professional teams, such as the oncologic, nursing, social work, rehabilitative care and home care teams.
Physicians may also practice in more than one organization, and responsibilities that have ceased in one setting does not terminate the therapeutic relationship in their other roles and associations with other elements of the care team. For example, a patient may be known to both the hospital inpatient unit and local home care team. An AOR discharge terminating a patient-physician relationship in the hospital does not suggest a severance of the therapeutic relationship in the palliative home care setting.
Here, we proffer a means of maximizing efforts to preserve the therapeutic relationship and ensure that appropriate measures are taken to protect the patient.
The impact of an AOR discharge
Despite the best efforts of a healthcare team, the use of AOR discharges from time to time is inevitable. Querques et al. [6] see the responsible utility of AOR discharge as a sign of professional outlook to patient care. Yet, within our local palliative care setting, the repercussions of an AOR discharge for the patient, their family and the palliative care team may be perceived very differently. Due to a scarcity of studies on AOR discharges in palliative care, much of our comments are based on our own experiences. While there are a few studies of patients leaving a medical care facility against the expressed advice of the medical team within the Accident and Emergency (A&E), paediatrics and psychiatric care settings, little is known about AOR discharge in palliative care patients [1,7,8].
The rationale for AOR discharges in the A&E and psychiatric settings is very different from that of palliative care. In the former, patients most at risk of requesting an AOR discharge are admitted (1) in a medical or psychosocial crisis, (2) involuntarily or due to pressure from family and caregivers, (3) in a state of dissatisfaction with treatment, or (4) due to desire for prohibited substances. However, applying data accrued from the A&E and psychiatric settings to an inpatient setting such as a palliative care unit is difficult due to inherent differences in the medical disciplines [8-15].
Table 1 highlights some key differences in the A&E and palliative care settings which create significant hindrances to re-applying the principles that enable a valid AOR discharge in an A&E setting to an inpatient palliative care setting.
Comparison of the two settings reveals differences in the: (1) relationship of patient to healthcare providers, (2) medical team's responsibility to patient's family, (3) levels of integration of the healthcare provision, (4) methods used for appraisal of patient's competence, (5) importance of cultural, religious, personal and social factors in the medical disciplines, (6) time and resources available to discuss the patient's options, (7) necessity of follow-up by medical teams, (8) availability of the option of home leave or terminal discharges. Therefore, relying on an AOR discharge to indemnify the physician in an inpatient palliative care setting on the assumption that the therapeutic relationship has been severed, may prove to be more complicated.
However, what is universal is that patients discharged AOR often deteriorate without appropriate help. Social, financial and health implications cannot be underestimated, particularly when old data reveals that such patients demonstrate higher readmission rates and increased morbidity and mortality [5,16-20].
With this in mind and the validity of an AOR discharge increasingly under scrutiny, we offer health care professionals with a means of addressing the issues before deciding on an AOR discharge.
Subjects and Methods
Problems applying pre-existing models to the palliative care setting
In the premises of the complex end-of-life care setting, a vast array of psychosocial, cultural, clinical, practical and financial concerns exist behind the right to treatment refusal that may impinge on the validity of patient's decisional capacity. This is important, particularly because these patients are susceptible to repeat admissions, exacerbations of their conditions and potentially death [7,8].
To contextualize this discussion and our concerns about AOR discharge in the palliative care setting, we present three patients which our authors from National Cancer Centre Singapore have seen in our experience in palliative care from years 2013 to 2014.
Case 1
Mark is a 42-year-old man diagnosed with metastatic lung cancer with lymph node, contralateral lung, bone and liver involvement. Due to mounting lethargy, weakness and increasing dyspnoea, Mark was admitted to the local palliative care unit, as he had difficulty caring for himself, and his brothers who lived with him had long working hours. Therefore, Mark was left alone at home for prolonged periods of time. Mark had no other care providers and was at risk of falls particularly when using the toilet. Despite this Mark refused the use of commode or adult diapers. He also refused the use of an oxygen concentrator, as he was keen to continue smoking.
Not long after hospice admission, Mark began to agitate for a discharge home and signed an AOR discharge form. Mark had a history of AOR discharges whilst at other medical facilities, though no reason was ever identified. On most occasions, Mark would seek an AOR discharge within 3 days of admission, only to re-present at hospital within a week with worsening symptoms.
Case 2
Nia is a 98-year-old Malaysian living with her grandniece and nephews in Singapore when she was diagnosed with rectal cancer. Nia and her family decided on comfort measures after clinical examination revealed potential lymph node and liver metastasis. Given her frail state and lack of physical support at home, the family opted for a hospice placement. However, within 24 hours of being transferred, Nia insisted on being discharged. It was believed that the rationale for this AOR discharge was because Nia’s family had to pay for her unsubsidized care at the hospice as she was not a Singaporean. Despite efforts by the palliative care team to get some of the costs waived and reduce the financial burden of the family to the level which they had stated would be manageable to them, the family insisted on discharge.
Case 3
Teng Chee was admitted to a palliative care hospice due to refractory acute myeloid leukaemia and bone marrow failure. Despite his bleeding diathesis, Teng Chee was adamant on pursuing Traditional Chinese Medical treatment (TCM), which included the use of cupping and acupuncture. When the medical team would not condone such treatment, Teng Chee opted for an AOR discharge. Teng Chee was motivated by his family not to ‘give up’ and continue to ‘fight’ through the use of TCM. For the family and Teng Chee who were told of the risks of cupping and acupuncture, TCM represented ‘hope’ when conventional Western options had failed. In addition, Teng Chee saw entering the hospice as ‘giving up’ and accepting his death, even though he was aware that he was bleeding spontaneously from his mouth, nose and rectum, and that the cupping which was applied to his back could result in severe pain, hematomas and potentially death.
Results
Analyses of the cases
In all 3 cases, an AOR discharge was granted. However, it is important to understand the (1) various psychosocial, cultural, social, familial and existential issues of the patients, and (2) whether an AOR discharge offers the legal protection that pivot on the termination of a physician’s legal duty to treat, through the establishment of a risk assumption defense and evidencing the patient’s refusal of care [5].
Here, we scrutinize each of these posits, remembering that most of Levy et al. [5] position is based on the A&E setting, rather than the palliative care setting.
Termination of a physician’s duty to treat
According to Levy et al. [5], an AOR discharge allows physicians to raise a unique defence to a medical malpractice claim. It states that the duty to treat is one of the four elements of negligence that a plaintiff must prove to prevail in a malpractice action. In addition to a duty to treat, a plaintiff must show that a physician breached this duty by failing to adhere to a standard of medical care when treating the patient. The breach must be shown to have caused the patient to suffer injury or damages.
The termination of the physician-patient relationship states that no duty to treat exists, i.e. "absent that relationship, the physician has no duty toward the patient and, therefore, cannot be liable under a negligence theory". Yet, can this position be sustained within a palliative care setting? The idea that the termination of the physicianpatient relationship dissolves any duty to treat is based on the judgments in Lyons v Walker Regional Medical Centre Inc, and Griffith v University Hospitals [21,22].
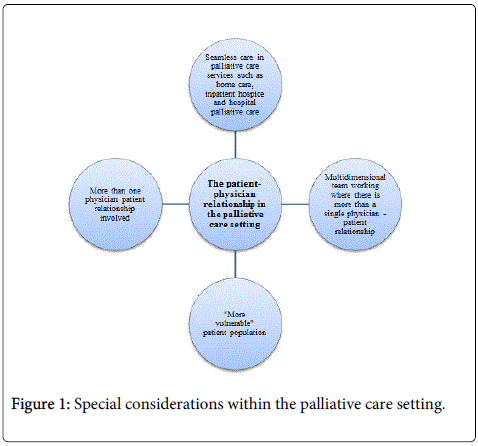
In an A&E setting, the physician-patient relationship is often clearly delineated and limited to a relationship between the patient and the treating physician. Therefore it is relatively straightforward to sever a therapeutic relationship through an AOR discharge. However, in palliative care practices, intricate links between the palliative care services in the hospital, hospice setting and home care services obscure the clear boundaries between the services. This type of care approach does not prioritize one therapeutic relationship over another. Therefore, simply terminating relationships through an AOR discharge may not circumnavigate liability due to special considerations within the palliative care setting (Figure 1).
The viability of Levy et al. [5] proposition of a severance of the therapeutic relationship which leads to the dissolution of a duty to treat and liability under the tort of professional negligence within the palliative care setting is also called into question when we consider issues rose in Table 1. Many pivots on the assumption of risk defence as a result of patient’s refusal of medical advice, the patient assumes the risks as consequential to refusing medical advice. Underpinning this assumption is the further assumption that the patient has capacity to refuse such advice and the physician has disclosed the appropriate risks to the patient. In the case of Mark (Case 1), his decision for an AOR discharge was in part fuelled by his wish to continue to smoke, a practice prohibited in the hospice. Indeed, his nicotine addiction may be seen as a coercive factor which impaired his capacity to appropriately weigh his options. It may be argued that in such circumstances and in the face of emotional issues, he was unlikely to have truly understood the consequences of severing his therapeutic relationship with the hospice team. Therefore, even if he could understand the facts and then make a choice, we question the validity of the choice due to the presence of coercive factors. In fact, Alfandre [23] remarked that proactively addressing substance abuse issues early during hospital admission can help prevent discharge dilemmas, and failure to consider these critical elements can lead to deficiencies in care and prevent the timely evaluation and intervention needed. Even though decisions to be discharged AOR can be related to a patient’s individual values [24], Alfandre [23] suggests that in such circumstances, appraisal and care provision is sub-optimal, which results in jeopardized treatment and lowered clinical standards which compromises the AOR process and voids any potential defence against negligence.
| A&E | Inpatient Palliative Care Unit | |
|---|---|---|
| Relationship of patient to healthcare providers | Usually involves a new relationship between the physician and the patient. The relationship is often limited to one main member of the medical team and the patient. |
Usually involves established relationships with various members of the home care and inpatient teams. |
| Medical team's responsibility to patient's family | No formal responsibility to the patient's family beyond the duty to maintaining the safety of the general public. | Part of the palliative care ethos is to provide care and support for the family, as well as bereavement support. |
| Levels of integration of the healthcare provision | In most cases, termination of the therapeutic relationship severs the responsibility of the unit towards the patient, since it is assumed that the patient would have refused transfer to the care of another physician or team. | An AOR in the palliative care setting may be difficult due to the integrated nature of services. |
| Methods used for appraisal of patient's competence | Appraisal of the patient’s competence is carried out by 1 member of staff. | Appraisals are often carried out by more than one member of the multidisciplinary medical team. |
| The importance of cultural, religious, personal and social factors in the medical disciplines | Less emphasis is required on the patient’s cultural, religious, personal and social factors, in the determination of capacity and the employ of an AOR discharge. | A holistic appraisal should be undertaken. |
| Time and resources available to discuss the patient's options | Limited opportunity to appraise the patient given time and resource constraints in emergency setting. | More time and resource in a palliative care setting to discuss patient's options. |
| Necessity of follow-up by medical teams | The patient may not be followed-up by the team after transfer to another discipline. | A follow-up by the home care team is usually done. |
| Availability of the option of home leave or terminal discharges | The option of home leave or terminal discharges is not available in an acute emergency setting. | The option of home leave or terminal discharges rather than an AOR is available, in order to preserve the therapeutic relationships in palliative care. |
Table 1: Key differences between AOR discharges in the A&E and inpatient palliative care setting.
The validity of an AOR discharge pivots on the patient’s capacity to make an informed decision based on the information provided. Section 4 of Singapore’s Mental Capacity Act (MCA) [25] articulates a two-stage test for capacity: (1) First, the health professional must determine whether the person is suffering from an impairment or disturbance that affects the functioning of the mind or brain. (2) Second, it must be determined whether that impairment or disturbance affects the person’s ability to make a decision at the particular time. We posit that in Mark’s case, the presence of coercive factors in conjunction with the probability of delirium among terminally ill patients would have irrevocably compromised his decision-making capacity and thus the validity of his assumption of risks.
The MCA further states that a person cannot make a decision for themselves if they are unable to understand the information relevant to the decision, retain that information, use or weigh that information as part of the decision-making process or communicate their decision (whether by talking, using sign language or any other means) [25,26]. It is noteworthy that in the palliative care setting, all these elements may be compromised. Here, the coercive influences of Mark’s (Case 1) nicotine addiction, the social and financial pressures faced by Nia (Case 2) over her medical care costs, and the familial and cultural influences on Teng Chee (Case 3) to maintain his ‘fight’ through the use of TCM, may each have compromised the patient’s deliberative capacity.
On understanding this, a number of issues are particularly salient in the palliative care context. It is well-documented that many patients are predisposed to alterations in their cognitive function due to psychiatric disorders, treatment, co-morbidities, and/or disorders of consciousness [27]. Nonetheless, the MCA prohibits one person from assuming that another lacks capacity simply because the latter has a specific condition. At this juncture, a multidimensional assessment must be sought to provide a balanced and informed decision of a patient’s specific context and a perception of the sometimes overt pressures confronting a patient.
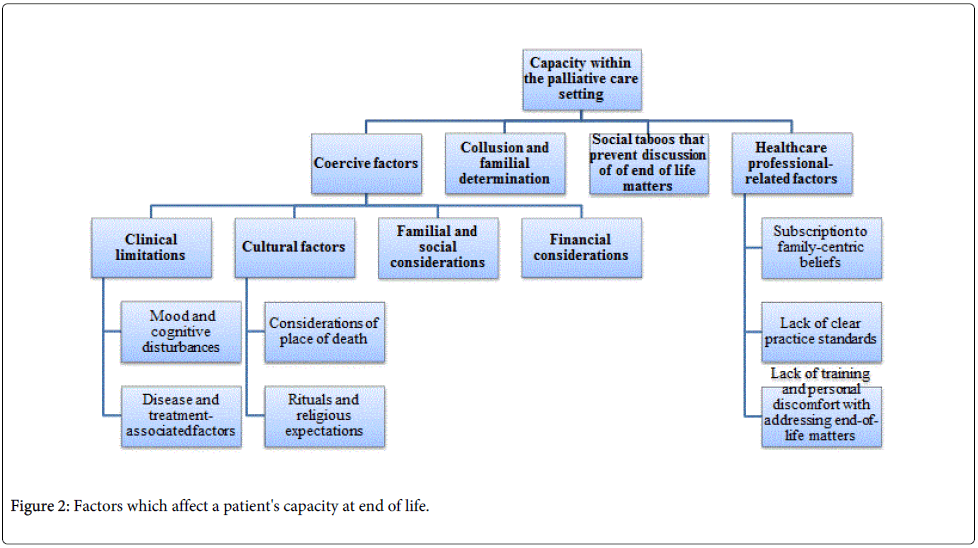
Mental capacity is only one aspect which may hinder the patient's ability to make an informed choice. Indeed, Nia’s case highlights yet another hindrance to the patient's ability to make an informed choice. Nia was not fully aware of her terminal state, which is consistent with local practices of collusion and familial determination, fed in part by the belief that maintaining hope will prolong life and spare loved ones from distress [27-33]. The impact of such practices is not limited to its effects on diagnosis disclosure, but also on the articulation of wishes and goals. Goh [34,35] reports that in the local setting, discussions of end-of-life care are frequently deemed taboo, inhibiting the writing of wills and the articulation of care plans by patients. The factors which affect a patient’s capacity at end of life are illustrated in Figure 2.
Due to this wide array of concerns, society recognizes that in moments of duress, stress and fear, expressions of preferences may be compromised and gives physicians the power to assess the decisional capacity of a patient, which was apparent in Nia’s case (Case 2). In certain circumstances, physicians may take measures to override patient refusal, to ensure the welfare of the individual [36].
It is also critical to appreciate that disruptions to an individual’s determinative ability or elements of the decision-making process could result from any contextualized, patient-specific factors affecting psychological and physical health, such as that of addiction, financial constraints and pressures from family, instead of simplistic medicallyrelated causes which affect cognition or global incapacity [25,26,36]. In such cases, there should be attempts to ensure respect for patient’s autonomy but without compromise on the maintenance of patient welfare, ostensibly through efforts to maintain the patient-physician relationship.
Results
The humanistic and holistic palliative care approach
In the palliative care setting, attempts are frequently made to preserve other therapeutic relationships between the patient, their loved ones, family and health care professionals, particularly when there is acceptance of the role of the palliative care team in caring of the patient’s loved ones during the patient’s illness as well as in providing bereavement care later.
When the patient realizes these long-term goals, a break in the therapeutic physician-patient relationship may be prevented. Furthermore, palliative care as a whole attempts to convey a more holistic and humanistic approach to care provision. In light of this view, an AOR discharge is much less desirable in comparison to a consensus about treatment from the physician, patient and other stakeholders after careful and in-depth discussion.
Efforts must be made to prevent deterioration in the relationship to the point when an AOR becomes necessary. To make compromises that are acceptable for the patient, the patient's family and the medical team should have regular meetings and understand one another's point of view, which would culminate in a much more desirable outcome than an AOR discharge. Here, flexibility is important as one may then arrange for medically-sanctioned discharges home, where the patient care is facilitated. Notably, shared decision making has a role in achieving more patient-centred care in decisions related to discharge against medical advice [37]. Hastily arranged medicallysanctioned discharges home that accept the realities of inevitable compromises in patient care are facilitated, often with home hospice care input, in order to preserve the therapeutic relationship.
Careful consideration of Mark’s (Case 1) situation on his wish to continue to smoke and his concepts of preserving his sense of dignity at the end of life, would have culminated in a better resolution instead of his subsequent experience, which was a re-admission to hospital some days later following a fall. On the other hand, closer inspection of Nia’s (Case 2) predicaments would have revealed that beyond the concerns about costs, was the pressure on the family to not ‘abandon’ the patient to a hospice, but to care for her at home. Facilitating the practical and personal needs of the family members, as they prepared to take ‘no pay leave’ to care for her, would have led to a more palatable solution. Tee Cheng’s (Case 3) family members were under significant pressure to fulfil their filial obligations to continue to care for him and Tee Cheng himself felt obliged to let them try, simply to prevent his children from being seen as abandoning him to his fate and subsequently enduring a ‘loss of face’, i.e. suffering humiliation from others.
Decisions made based on patient's context
Balance between a paternalistic approach and absolute patient autonomy is sought through careful and active listening to the patients concerns, wishes and views, while also assessing the viable options that least compromises their care [38]. This process of assessment also serves to correct misunderstandings and address shortfalls in patient care, thus providing a better understanding of the psychodynamics of the patient’s and their carer’s social, emotional, physical, financial, spiritual and cultural considerations. Such a process will improve the understanding of the positions of various parties' involvement in the deliberative process, build trust between patients, their caregivers and health care professionals, allow appraisal of the way in which decisions are made, and lower the prevailing tensions during the deliberative process. It will also provide insights into the reasons for acting against medical advice and potentially identify more acceptable alternatives for effective and practical delivery of patient-centred care [30-32,38]. This is evident from the later evaluations of the three cases presented.
Having a multidisciplinary medical team to obtain a 'balanced' viewpoint
In Singapore, a multidisciplinary medical team approach employs a group of people of different healthcare disciplines, which meets together at a given time (whether physically in one place, or by video or teleconferencing) to discuss a given patient [39]. The multidisciplinary team is seen as a source of ‘balance’ to various ideas, opinions and perspectives of all involved in a patient’s care, in order to provide a holistic viewpoint of the situation. This ensures that all decisions made are well-considered, equitable, effective, and accountable and focused on providing the patient and their families with the best and most appropriate care as determined by the specifics of their individual circumstances. Through careful consideration of both clinical and psychosocial issues, in addition to the values, cultural and spiritual matters relevant to the patient, decisions made on care provision will be beyond a purely clinically-orientated approach. Therefore, there are times when the input of the physician is not the most important. Instead, the medical social worker’s perspectives become the pivotal factor when significant psychosocial considerations are involved, as was the case with Nia (Case 2) or the physiotherapist and the occupational therapists in Mark’s (Case 1) circumstances and the nurse’s understanding of Teng Chee’s (Case 3) sociocultural pressures.
Given the breadth and variability of individual factors to each specific aspect, it is logical that a multidisciplinary team, rather than a single individual member of the health profession, elucidates the priorities in each case [40]. The multidisciplinary team is perceived to tamper ill-judged, ill-informed, unilateral decision-making invoked by a need to carry out the assigned duty. In particular, the multidisciplinary team has been found to assuage inclinations to overtreat or not accept patient's refusal of treatment options even when the patient is no longer benefitting, or in fact suffering, due to the implemented treatments. In addition, this model limits and negates proclivities held by any member of the multidisciplinary team.
Giving a 'weight' to each aspect of a patient's needs and desires
Through open discussions underlined by professional respect and courtesy, a platform for considering the myriad of relevant matters pertaining to a case is allowed. Each aspect of the patient's needs and desires is balanced and given a 'weight' before decisions are made. In such a model, ‘weight’ refers to: the importance and pertinence which a specific matter holds in a deliberation. Wherever possible, it is the patient and the families who determine the importance of each element within the discussion, and not the senior or ‘vocal tenacity’ of a member of the multidisciplinary team. Conversely, in some cases such as that of Mark (Case 1), Nia (Case 2) and Tee Cheng (Case 3), such 'weights' needs to be balanced with the realities of the situation and the potential harms to the patient, should certain decisions be made.
Documenting clearly the negotiation and deliberation process
The whole deliberation process should be documented clearly, like the discussions held with the patient, their caregivers and their palliative home care teams. The multidisciplinary team often gives specific ‘caregiver training’ to the individuals taking care of the patient at home, and provides equipments which the patient require to minimize disruption to patient care [30,31]. Such actions ensure accountability, transparency and true understanding of the patient's progress, in the process of discussing the patient's options.
Conclusion
It is clear that using an AOR discharge within the local health care setting is fraught with problems, as a result of the wider considerations of palliative care patients and the overarching goals of a palliative care approach. Indeed, we hope that discussions thus far emphasize the importance of maintaining the therapeutic relationships in patient care, and provide greater impetus to curtailing the need for AOR discharges wherever possible, among inpatients of palliative care or other medical disciplines. We hope that using the multidimensional approach adopted within Krishna, Lee and Watkinson’s Welfare Model [41] to assess the situation will help in these efforts.
However, we also hope that should these efforts fail and an AOR discharge does arise, Krishna, Lee and Watkinson’s Welfare Model [41] will pave the way to decisions which extend beyond simple respect for patient autonomy, and aspire towards broader considerations of the patient’s welfare based on the far-reaching goals of a holistic palliative care approach.
References
- Al Ayed I (2009): What makes patients leave against medical advice? Journal of Taibah University Medical Sciences 4:16-22.
- Tsai DF (2005) The Bioethical Principles and Confucius' Moral Philosophy. J Med Ethics 31:159-163.
- Penal Code Chapter 224, Chapter XVI Offences Affecting The Human Body.
- https://www.moh.gov.sg/content/moh_web/home/policies-and-issues/advance_medical_directiveamd.html.
- Levy F, Mareiniss DP, Iacovelli C (2012) The importance of proper against-medical-advice (AMA) Discharge. J Emergency Medicine 43:516-520.
- Querques J, Kontos N, Freudenreich O (2014) Discharges Against Medical Advice. JAMA 311: 17.
- Baptist AP, Warrier I, AroraR, Ager J, Massanari RM (2007) Hospitalized patients with asthma who leave against medical advice: Characteristics, reasons, and outcomes. J Allergy ClinImmunol119:924-929.
- Brooks M, HiltyDM, Liu W, Hu R, Frye MA (2006) Discharge Against Medical Advice From Inpatient Psychiatric Treatment: A Literature Review. Psych Serv 57: 1192-1198.
- Akhtar S, Helfrich J, Mestayer RF (1981) AMA discharge from a psychiatric inpatient unit. Int J Soc Psychiatry 27:143-150.
- Harper DW, Elliott-Harper C, Weinerman R, Anderson NJ, Nelson TA (1982) A comparison of AMA and non- AMA patients on a short-term crisis unit. Hosp Community Psychiatry 33:46-48.
- Jeffer EK (1993) Against medical advice: part II, the Army experience 1971-1988. Mil. Med 158:73-76.
- Kecmanovic D (1975) Patients discharged against medical advice from a lock-and-key psychiatric institution. Int J SocPsychiatr21:274-281.
- Long JP, Marin A (1982) Profile of patients signing against medical advice. Journal of Family Practice 15:551-552.
- Louks J, Mason J, Backus F (1989) AMA discharges: prediction and treatment outcome. Hosp Community Psych 40: 299-301.
- Phillips MS, Ali H (1983) Psychiatric patients who discharge themselves against medical advice. Can J Psychiatry 28:202-205.
- Tehrani E, Krussel J, Borg L, Munk-Jørgensen P (1996) Dropping out of psychiatric treatment: a prospective study of a first-admission cohort. ActaPsychiatricaScandinavica 94:266-271.
- Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, et al. (2002) Leaving hospital against medical advice among HIV-positive patients. CMAJ 167:633-637.
- Fiscella K, Meldrum S, Barnett S (2007) Hospital discharge against advice after myocardial infarction: deaths and readmissions. Am J Med 120:1047-1053.
- Hwang SW, Li J, Gupta R, Chien V, Martin RE (2003) What happens to patients who leave hospital against medical advice? CMAJ 168: 417-420.
- Windish DM, Ratanawongsa N (2008) Providers’ Perceptions of Relationships and Professional Roles when Caring for Patients who Leave the Hospital Against Medical Advice. J Gen Intern Med 23:1698-1707.
- http://www.medscape.com/viewarticle/770719_1
- https://www.courtlistener.com/opinion/1094071/lyons-v-walker-regional-medical-center/authorities/
- Alfandre D (2009) I'm Going Home: Discharges Against Medical Advice. Mayo ClinProc 84: 255-260.
- Alfandre D (2013) Reconsidering against medical advice discharges: embracing patient-centeredness to promote high quality care and a renewed research agenda. J Gen Intern Med 28:1657-1662.
- Cap 177A (2010) Rev Ed Sing.
- Menon S (2013) The Mental Capacity Act: Implications for Patients and Doctors Faced with Difficult Choices. Ann Acad Med Singapore 42:200-202.
- http://www.researchgate.net/publication/234095592_Psychiatric_symptoms_in_palliative_medicine
- http://app1.mcys.gov.sg/portals/0/summary/research/publications-survey-sas2001.pdf.
- Ho ZJM, Krishna LKR, Yee CPA (2010) Chinese Familial Tradition and Western Influence: A case Study in Singapore on Decision Making at the end of life. JPSM 40(6):932-937.
- Krishna L (2011) Decision making at the end of life: A Singaporean Perspective. Asian Bioethics Review 3:118-126.
- Krishna L (2011) The Position of the Family of Palliative Care patients within the Decision Making Process at the end of life in Singapore. Ethics and Medicine 27:183-190.
- Krishna L (2011) Nasogastric feeding at the end of life: A virtue ethics approach. Nurs Ethics 18: 485-494.
- Tan C (2012) Our Shared Values in Singapore; A Confucian Perspective. Educational Theory 62:449-463.
- Goh CR (2008) Challenges of cultural diversity. In J Beattie & S Goodlin (eds.), Supportive Care in Heart Failure. 451-461.
- Goh CR (2008) Culture, ethnicity and illness. In: Walsh TD, Caraceni AT, Fainsinger R, Foley KM, Glare P, et al. (eds) Palliative Medicine Philadelphia, PA:Saunders/Elsevier, pp. 51-54.
- Capozzi JD, Rhodes R (2002) Assessing a Patient’s Capacity to Refuse Treatment. J. Bone Joint Surg. Am 84:691-693.
- Alfandre D, Schumann JH (2013) What is wrong with discharges against medical advice. JAMA 310:2393-2394.
- Tong SF, Chen R (2007) A patient who refused medical advice: the doctor and the patient should look for common ground. Malaysian Fam Physician 2:110-113.
- London: Department of Health (2004). Manual for Cancer Services 2004.
- Fegg MJ, Brandstatter M, Kramer M, Kogler M, Haarmann- Doetkotte S, et al. (2010) Meaning of life in palliative care patients. J Pain Symptom Manage 40:502-509.
- Krishna LK, Watkinson DS, Beng NL (2014) Limits to relational autonomy-The Singaporean experience. NursEthics 22:331-340.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 22548
- [From(publication date):
July-2015 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 18077
- PDF downloads : 4471