The Purpose of Palliative Care Towards the End of Life is to Improve Quality of Life and have a Positive Impact on how the Illness Develops
Received: 30-Sep-2022 / Manuscript No. jpcm-22-77151 / Editor assigned: 03-Oct-2022 / PreQC No. jpcm-22-77151 (PQ) / Reviewed: 17-Oct-2022 / QC No. jpcm-22-77151 / Revised: 21-Oct-2022 / Manuscript No. jpcm-22-77151 (R) / Accepted Date: 27-Oct-2022 / Published Date: 28-Oct-2022 DOI: 10.4172/2165-7386.1000482
Abstract
The aim of palliative care is to alleviate suffering in patients and their families by evaluating all of the symptoms that patients experience on a physical, psychological, and spiritual level and treating them. It assists patients and their loved ones in reaching an appropriate medical treatment agreement and supporting the patient care objective with medical providers. The establishment of advance directives, the need for a proxy, and the status of resuscitation are all crucial components of palliative care towards the end of life. Recognizing the function of palliative care at the end of life is the goal of this review. A patient's symptom load may grow as death draws near, necessitating more extensive palliation. The care given to the relatives of a dying patient improves as ease measures do. After a patient has passed away, palliative care's job is mostly focused on providing the patient's family with assistance during this difficult time.
Keywords
Palliative care; End of life; Quality of life; Positive influence; Illness
Introduction
By establishing a network and cooperative group for the study application and research techniques in India, it would be possible to identify the problems that may improve the provision of palliative care and the areas where practical evidence is still lacking. With an emphasis on reporting the medical practices quality and quality of dying in patients when a cure may or may not be achievable and who have advanced stage illnesses, palliative care gains are produced [1]. In line with WHO Through the early detection, accurate evaluation, and treatment of pain and other difficulties, physical, emotional, and spiritual, palliative care is a method that enhances the quality of life for patients and their families facing the challenge associated with lifethreatening disease [2].
Despite the fact that death is a natural part of life, it is sometimes handled as an illness. A lot of lonely, suffering people pass away in hospitals, which is significant. The basic goals of palliative care are to anticipate, identify, prevent, ad treat symptoms that patients with serious or life-threatening illnesses experience, as well as to support patients and their families while they make critical medical decisions. Improving both the patient's and their family's quality of life is the clear objective of palliative care. It has a favourable impact on how a disease develops [3]
According to a systematic review from 2016, nurses were the greatest shared interventionists, working as a role practitioner in 70% of studies or in teams, and health services of palliative care found more support for their role than any other discipline of the 98/124 studies that were labelled provider disciplines. Palliative care refers to the use of specific precautions to anticipate, prevent from suffering and treat serious disease in order to maximise the quality of life for both patients and their families. It takes into account the many illnesses, as well as the patients' psychological, physical, emotional, and spiritual needs [4]. Palliative care is anticipated to be helpful in 38%-74% of all fatalities worldwide. According to a study, using palliative care in Belgium has a beneficial effect on treatment quality and lowers overall expenditures of care [5].
Methods
Using Google search engines, Medline, and Web of Science, literature searches have been conducted on a variety of palliative care topics, including palliative care, its role in end-of-life care, quality of life, and its favourable impact on the course of disease. Every piece of information about palliative care has been gathered, examined, and then summarised.
Results
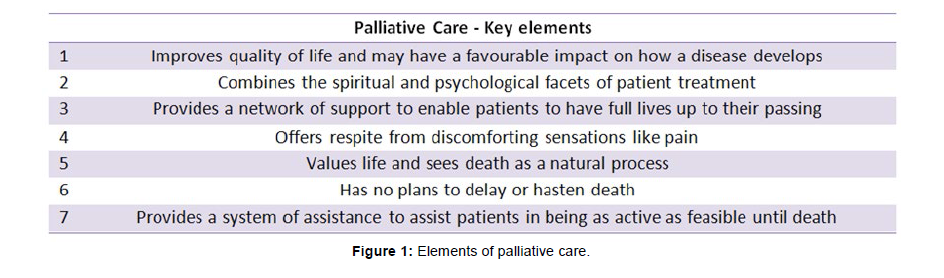
These categories are used to organize compiled data and information about palliative care (Figure 1).
Palliative care- key elements
Compared to standard treatment, palliative care offers improved symptom control and quality of life. Palliative care is underused in the advanced management of terminal disease, despite its documented advantages. It is expected that more than 1 million people would pass away in 2011 (45 percent of all fatalities occur in the United States). Despite the fact that data shows a consistent upward trend, over two thirds (63.1%) of those patients got care for less than a month, and 36.1% were either released or passed away within 7 days of admission. Family, carers, and friends can also benefit, which demonstrates increased approval for the quality care and attention to caregiver need. WHO's list of palliative care's advantages [6].
Common core:
People who are reaching the end of their lives frequently need specialised assistance and care. Several significant principles are included in palliative and end-of-life care: These guidelines give professionals who provide end-of-life care an overview [7].
• The person's priorities, including their spiritual, emotional, and cultural requirements, guide all choices and activities in the planning and delivery of care and support.
• Clear, timely, and appropriate communication is presented with tact, taking into account the conditions, requirements, and capabilities of the recipient and their caregivers.
• Integral working is used to offer end-of-life care, with practitioners working together to guarantee seamless care and support at the moment of delivery.
• Information that is good, clear, and direct is given to patients and their caregivers.
• Effective communication and regular evaluations guarantee that care and assistance are responsive to the needs and evolving circumstances of individuals and their caregivers.
• Caregivers' needs and rights are acknowledged and taken into consideration.
Palliative care extends its responsibility to assist with grief, if necessary, with the primary objective of achieving the highest possible quality of life for the patient and their loved ones. The idea of "term care" is "complete suffering," which is seen to include not just bodily symptoms but also social, psychological, and spiritual issues. The identification of the patient's overall state as well as the evaluation of the quality of the services offered depends critically on the patient's quality of life. It is clear that early multidisciplinary palliative care and caregiver support aid the patient in achieving effective symptom management and a higher quality of life.
Two common dangers were identified by a study as belonging to the structure and content measurement that carries the quality life designation. Such measures have a tendency to mimic a multidimensional conceptual strategy. In determining a person's quality of life, the following aspects of health are frequently considered, either more or less.
1. Physical well-being, which includes factors like sickness symptoms, bodily sensations, and repercussions from medical treatments.
2. Mental health ranges from a feeling of general wellbeing through non-pathological types of psychological suffering to diagnosable mental disorders.
3. Social health, which includes a quantitative and qualitative analysis of contacts and interactions within the community.
4. Functional health, which entails physical activity in connection to job and family obligations as well as physical functioning in terms of self-care and social role functioning [8].
A major objective of medical care towards the end of life is the idea of pain alleviation. The first step in treating it is to acknowledge the pain and suffering. The assessment and diagnosis of pain and suffering both depend on this idea. Pain has four different components.
Components of pain: Physical problems, Anxiety, depression, anger, Interpersonal problems, not accepting death approach.
At the end of life, in particular, it is important to treat all of the patient's suffering. Until all aspects of overall pain are treated, optimal pain alleviation will not be feasible. Understanding the notion of pain may assist improve quality of life and have a beneficial impact on how a disease develops.
Managing typical bodily symptoms
In the many contexts Patients may get palliative care in settings such as nursing homes, private residences, hospitals, day hospitals, and hospices. The interdisciplinary participation in controlling symptoms of various life-limiting or terminal illnesses is an important part of palliative care. Patients have a variety of physical symptoms such as poor nutrition can lead to concerns with tissue viability, weight loss, dehydration, infections, incontinence, shortness of breath, nausea, and vomiting, etc.
It's crucial to treat these symptoms in a multidisciplinary setting while maintaining open lines of communication with the patients and those who are caring for them. A helpful guide on end-of-life care was produced by the General Medical Council in 2010. Distressing physical and psychological symptoms should be treated, but there are times when medication, artificial feeding, and hydration should be discontinued. Teams providing palliative care are crucial in providing end-of-life care. Their early engagement is essential for the comprehensive care of individuals who are terminally ill [9].
Health care personnel are increasingly required to learn a patient's preference for where to die, to record it, and to try to fulfil it. It provides high-quality palliative care to all patients who are reaching the end of their lives, regardless of their diagnosis, allowing them to decide if they want to pass away at home. Death palace should debatably be considered alongside homes, hospitals, hospices, and nursing homes [10]. According to a research evaluation by Beccaro, 93.5% of cancer patients in Italy chose to die at home, according to their poll on actual and desired places of death. Arnold came to the conclusion that patients' professed preferences for last resting sites varied. The majority of patients (80%) who had never been hospitalised to a hospice preferred to pass away at home, they highlighted. As a result, a whopping 79% of those who had at least one admission at a hospice desired to pass away there.The goal of palliative care specialists is to keep patients at home as long as possible allowing for a more natural death at home. Home deaths might be seen as a result of excellent palliative care. People's actual site of death and whether they want to pass away there are frequently brought up in efforts to improve care for the dying, raising the possibility that they might serve as markers of the effectiveness of palliative care [11].
Conclusion
The goal of palliative care is to enhance quality of life. Additionally, it totally alters the course of a sickness and, when used early on in the illness, may lengthen life. There is an added financial strain in India. People afflicted by them require assistance to deal with these problems since they result in a low quality of life. Palliative care offers assistance in resolving these issues. Since palliative care is "whole care," a multidisciplinary team is needed to provide it. Doctors, nurses, counsellors, dieticians, and social workers make up the majority of this team, which collaborates to ensure that patients nearing the end of their lives have the highest quality of life possible.
Acknowledgement
Not applicable.
Conflict of Interest
Authors declare no conflict of interest.
References
- Mohanti BK (2011) Research focus in palliative care. Indian J Palliat Care 17: S8.
- Choudhary S, Mahala P (2021) Role of Palliative Care at the End of Life: To Enhance the Quality of Life and Positively Influence the Course of Illness. P J Nurs14: 42-45.
- Rome RB, Luminais HH, Bourgeois DA, Blais CM (2011) The role of palliative care at the end of life. Ochsner J 11: 348-352.
- Singer AE, Goebel JR, Kim YS, Dy SM, Ahluwalia SC, et al. (2016) Populations and interventions for palliative and end-of-life care: a systematic review. J Palliat Med 19: 995-1008.
- Maetens A, Beernaert K, De Schreye R, Faes K, Annemans L, et al. (2019) Impact of palliative home care support on the quality and costs of care at the end of life: a population-level matched cohort study. BMJ open 9: 25180.
- McAteer RA, Wellbery CE (2013) Palliative care: benefits, barriers, and best practices. Am Fam Physician 88: 807-813.
- Richards CT, Gisondi MA, Chang CH, Courtney DM, Engel KG, et al. (2011) Palliative care symptom assessment for patients with cancer in the emergency department: validation of the Screen for Palliative and End-of-life care needs in the Emergency Department instrument. J Palliat Med 14: 757-764.
- Thaniyath TA (2019) The quality of life of the patients under palliative care: The features of appropriate assessment tools and the impact of early integration of palliative care. Palliat Care.
- Singh K (2013) Fundamental and holistic aspects of palliative care.
- Munday D, Dale J, Murray S (2007) Choice and place of death: individual preferences, uncertainty, and the availability of care. J R Soc Med 100: 211-215.
- De Roo ML, Miccinesi G, Onwuteaka-Philipsen BD, Van Den Noortgate N, Van den Block L, et al. (2014) Actual and preferred place of death of home-dwelling patients in four European countries: making sense of quality indicators. PloS one 9: 93762.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Prakash M, Salins N (2022) The Purpose of Palliative Care Towards the End of Life is to Improve Quality of Life and have a Positive Impact on how the Illness Develops. J Palliat Care Med 12: 482. DOI: 10.4172/2165-7386.1000482
Copyright: © 2022 Prakash M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1419
- [From(publication date): 0-2022 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 1112
- PDF downloads: 307