The Prevalence of Work-Related Stress Complaints among Healthcare Workers for the Disabled Participating in a Workers’ Health Surveillance Program
Received: 05-Dec-2016 / Accepted Date: 27-Dec-2016 / Published Date: 31-Dec-2016 DOI: 10.4172/2329-6879.1000256
Abstract
Background: Healthcare workers are at high risk for developing mental health complaints due to frequent exposure to risk factors such as high work demands, low work control and high emotional demands. Aim: To be able to plan a job-specific workers’ health surveillance (WHS) program properly, knowledge about the number of workers that could be expected to be the target for interventions should be known. Therefore we studied the prevalence of stress and common mental health complaints among Dutch healthcare workers for the disabled who voluntarily participated in WHS in a large healthcare organization.
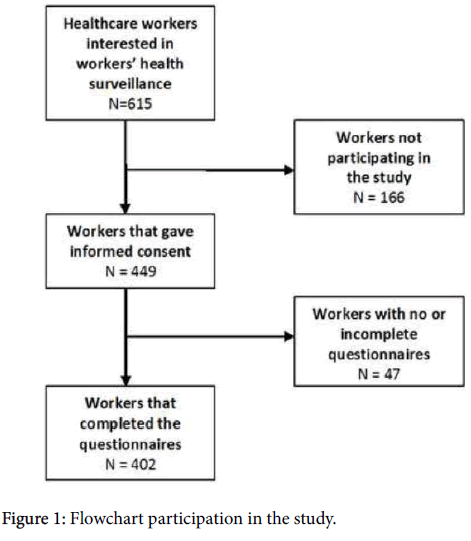
Methods: In total, 615 workers positively responded to the invitation for the surveillance program; 449 workers were willing to participate in the research study by giving informed consent. We used validated scales to assess general stress, work-related fatigue, distress, burnout, and posttraumatic stress. The prevalence rate of each mental health complaint was calculated.
Results: Information from 402 workers was eligible for analysis (response rate 65%). The mental health prevalence rates were: general stress 22%, work-related fatigue 17%, distress 12%, burnout 6%, post-traumatic stress complaints 8%.
Conclusions: Common mental health complaints among healthcare workers of the disabled is common (one in every five workers) for general stress and work-related fatigue. Distress was found in about 10% of the workers. Burnout and post-traumatic stress was less common (1 in 19-20 workers). This study suggests that to ensure future workers’ health and quality of care, employers of healthcare workers of the disabled should be offered WHS with adequate intervention strategies periodically.
Keywords: Occupational health; Workers health surveillance; Health personnel; Care givers; Psychological stress; Mental fatigue; Burnout; PTSD; Prevalence
55709Introduction
Healthcare workers are at high risk for developing occupational mental health complaints due to frequent exposure to risk factors such as high work demands, low work control and high emotional demands [1]. Exposure to these risk factors may increase the chance of experiencing stress complaints and other mental health complaints. Mental health complaints can affect work performance. This was shown in a study on hospital physicians [2]. These complaints also influence other aspects such as the quality of interaction with patients and colleagues [3]. To keep healthcare availability at the desired level, it is important to keep workers healthy in their job and to prevent ill health or absenteeism. It is known that moderate and high psychological distress increases the odds for workplace failure and decreases the odds for workplace success [4]. Efforts to prevent workrelated health problems usually target employees who already show a certain degree of impairment of health or work functioning. With a Workers’ Health Surveillance (WHS) program we can focus more on early detection of impaired health to prevent a loss in work functioning. To be able to plan a job-specific WHS properly, knowledge about the number of workers that could be expected to be target for interventions should be known. We therefore studied the prevalence of stress and common mental health complaints among Dutch healthcare workers for the disabled from a large healthcare organization during a pilot WHS.
Method
A cross-sectional study was performed in 2015 in a Dutch healthcare organization for the disabled of 7,600 employees. Study subjects were recruited by opportunity (voluntary response) sampling. About one third of the total population was invited to participate in a voluntary WHS. Workers who were interested in WHS (N=615) were contacted. This is the source population for the study. The employees worked either as an attendant, assistant-attendant or domestic worker. Official approval by the Medical Ethics Review Committee of the AMC was not required. General stress complaints and work-related fatigue were assessed by the Need for Recovery after Work scale and the Depression Anxiety Stress Scale (DASS). The Need for Recovery after work scale is the work-related fatigue scale and part of the Dutch Experience and Evaluation of Work Questionnaire (Dutch: VBBA) [5,6]. The scale measures the extent to which employees experience problems in recovery efforts from work. The scale score is calculated by adding the individual's scores on the eleven (recoded) yes/no items. This scale score is transformed into a scale ranging from 0 to 100. Higher scores (>54.4) indicate a high degree of need for recovery after work. Stress was assessed by the Depression Anxiety Stress Scale (DASS-21) [7]. This scale contains 13 theses about stress with the response categories “never (0),” “sometimes (1),” “often (2),” “mostly (3),” and “always (4)”. A scale score of 10 points or higher can be regarded as a high level of general stress. The first of the specific mental health screeners was the distress-screener [8]. This scale has three items about the worker’s feeling in previous week with a four point Likert scale of “no (0),” “sometimes (1),” “regular (2)” and “often (2)” A summed score of 4 points or more means an indication for adjustment disorder. Burnout was assessed through its two key dimensions: emotional exhaustion and cynicism [9,10]. Emotional exhaustion (5 items) is marked by a general feeling of extreme chronic fatigue caused by continuous or prolonged exposure to harsh working conditions. Cynicism (4 items) is defined as a hardened and cynical attitude to the work and/or persons with whom one works. Both scales consist of items with the response categories “never”(0), “almost never” (1), “sometimes” (2), “regular” (3), “often” (4), “very often” (5) and “always” (6). A summed mean score of 2,2 on emotional exhaustion and 2,0 on cynicism was used as indication for burnout. The last screener is the Dutch version of the “Impact of Event” scale, a screener of Post-Traumatic Stress. It consists of 15 theses with the response categories “not at all (0),” “rarely (1),” “sometimes (3),” and “often (5).” A scale score over 26 points means an indication of PTSD [11].
Results
In total, 615 workers positively responded to the invitation for the WHS program; A total of 449 workers were willing to participate in the research study by giving informed consent. Of these, 402 participants (65% of all positive responders) completed the questionnaires completely. A flowchart is presented in Figure 1.
In Table 1 we present the demographic data of the study population. Most participants are women with a mean age of 51 years and a parttime contract of 24 hours a week.
| Sex | Number | (%) |
|---|---|---|
| Male | 47 | 12 |
| Female | 355 | 88 |
| Age | (Range) | |
| Mean age (years) | 51.3 | 27-80 |
| Employment | Hours/years | (Range) |
| Mean hours employment contract (hours) | 23.5 | Jul-40 |
| Duration employment contract (years) | 13.6 | 0-40 |
Table 1: Demographic data study sample (number, mean and %).
The prevalence of general stress among healthcare workers for the disabled in this study is 22% (Table 2). Work-related fatigue is a problem for 17% of the respondents. Distress was high in 12%; 6% of the respondents scored indicative for burn out and 8% scored indicative for PTSD.
| Mental health problem | Prevalence rate (%) |
|---|---|
| Work-related fatigue | 17 |
| General stress | 22 |
| Distress | 12 |
| Burnout | 6 |
| Posttraumatic stress | 8 |
Table 2: Prevalence rates of mental health problems in the study sample (N=402).
Discussion
Mental health complaints among healthcare workers of the disabled that participated in a WHS program are common (about one in every five workers) for general stress and work-related fatigue. Distress was found in 12% and burnout and post-traumatic stress was less common (1 in 19-20 workers). In the Mental Vitality @ Work study, Ketelaar et al. [12] studied in a randomized controlled trial the effects of an Emental health intervention in a WHS program on mental health of hospital nurses and allied health professionals of a large hospital. By using the same questionnaires and cut-off points, they found slightly higher prevalence of mental health complaints among WHS participants in their baseline population: distress 24%, work-related fatigue 34% and PTSS 12%. The authors in that study aimed for high sensitivity, since they did not want to miss participants who might need help. In a cross-sectional study among professionals (most nurses) linked to the primary healthcare network in the city of Aracaju, Brasil, the prevalence of high risk of burnout (7%) showed findings comparable with our results [13]. However, study participants in that study were merely restricted to higher education professionals and the sampling was not related to WHS.
Mental health complaints seem to be a prevalent problem in healthcare workers of the disabled which can be seen as an opportunity to start a preventive program. The more so because screening on health issues with a higher prevalence theoretically increases the positive predictive value of the outcome. This enables an effective referral to adequate interventions in this population. Moreover, knowing the prevalence estimates gives an indication how many mental health interventions should be planned for. We did not perform a nonresponse study among the 35% of the workers that did not respond (completely) after they had indicated their interest in the WHS program. Analysis showed no differences in sexes and age between responders and non-responders. However, taking into account the low response rate to the initial invitation for WHS, future strategies to increase the attendance rate are needed. When we compare the response to the invitation for a voluntary WHS with other WHS programs in healthcare employees, our response is substantially lower [14-16]. A reason for this might be the reorganization that took place in the healthcare organization with a job loss of 10 percent of all employees.
References
- Bültmann U, Kant IJ, Van den Brandt PA, Kasl SV (2002) Psychosocial work characteristics as risk factors for the onset of fatigue and psychological distress: prospective results from the Maastricht Cohort Study. Psychol Med 32: 333â€345.
- Ruitenburg MM, Frings-Dresen MH, Sluiter JK (2012) The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability: a cross-sectional study. BMC Health Serv Res 12:292-298.
- Gärtner FR, Nieuwenhuijsen K, van Dijk FJ, Sluiter JK (2010) The impact of common mental disorders on the work functioning of nurses and allied health professionals: a systematic review. Int J Nurs Stud 47:1047-1061.
- Hilton MF, Whiteford HA (2010) Associations between psychological distress, workplace accidents, workplace failures and workplace successes. Int Arch Occup Environ Health 83:923-933.
- van Veldhoven M, Broersen S (2003) Measurement quality and validity of the ‘need for recovery scale’. Occup Environ Med 60:i3-i9.
- de Croon EM, Sluiter JK, Frings-Dresen MH (2006) Psychometric properties of the Need for Recovery after work scale test/retest and sensitivity to detect change. Occup Environ Med63:202-206.
- Henry JD, Crawford JR (2005) The short term version of the Depression Anxiety Stress Scale (DASS-21) Construct validity and normative data in a large non clinical sample. Br J ClinPsychol 44:227-239.
- Braam C, van Oostrom SH, Terluin B, Vasse R, de Vet HC, et al. (2009) Validation study of a distress screener. J OccupRehabil 19:231-237.
- Bakker AB, Demerouti E, Schaufeli WB (2002) Validation of the Maslach Burn-out Inventory-Gerenal Survey: An internet study. Anxiety, Stress and Coping 15:245-260.
- Maslach C, Schaufeli WB, Leiter MP (2001) Job burnout. Annu Rev Psychol52:397-422.
- van der Ploeg E, Mooren TT, Kleber RJ, van der Velden PG, Brom D (2004) Construct validation of the Dutch version of the impact of event scale. Psychol Assess 16:16-26.
- Ketelaar SM, Nieuwenhuijsen K, Gärtner FR, Bolier L, Smeets O, et al. (2013) Effect of an E-mental health approach to workers' health surveillance versus control group on work functioning of hospital employees: a cluster-RCT. PLoS One 8:e72546.
- Silva SC, Nunes MA, Santana VR, Reis FP, Machado Neto J, et al.(2015) Burnout syndrome in professionals of the primary healthcare network in Aracaju, Brazil. CienSaude Colet 20:3011-3020.
- Ketelaar SM, Nieuwenhuijsen K, Bolier L, Smeets O, Sluiter JK (2014) Improving work functioning and mental health of healthcare employees using an e-mental health approach to workers’ health surveillance: pretest-posttest study. Saf Health Work5:216-221.
- Opie T, Dollard M, Lenthall S, Wakerman J, Dunn S, et al. (2010) Levels of occupational stress in the remote area nursing workforce. Aust J Rural Health 18:235-241.
- Ruitenburg MM, Plat MC, Frings-Dresen MH, Sluiter JK (2015) Feasibility and acceptability of a workers' health surveillance program for hospital physicians. Int J Occup Med Environ Health 28:731-739.
Citation: Blekemolen JRM, Hulshof CTJ, Sluiter JK (2016) The Prevalence of Work-Related Stress Complaints among Healthcare Workers for the Disabled Participating in a Workers’ Health Surveillance Program. Occup Med Health Aff 4:256. DOI: 10.4172/2329-6879.1000256
Copyright: © 2016 Blekemolen JRM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7648
- [From(publication date): 0-2016 - Nov 23, 2024]
- Breakdown by view type
- HTML page views: 6768
- PDF downloads: 880