Research Article Open Access
The Prevalence of Gluten-Free Diet at the University of Otago: A Cross- Sectional Survey
Douglas Hancock*, Sultan Al-Shaqsi, Mastura Badron, Nadiah Mohd Rafain, Kurinji Nalankilli, Shivam Deo, Jayani Kannangara, Ray Li, John Dockerty, Josie Athens and Kirstin Kenrick
Dunedin School of Medicine, University of Otago, New Zealand
- Corresponding Author:
- Douglas Hancock
House Officer, Capital and Coast District Health Board
Wellington, PO Box 7902, New Zealand
Tel: +64-4-3855999
Fax: +64-4-3855856
E-mail: Douglas.Hancock@ccdhb.org
Received Date: July 15, 2014; Accepted Date: August 26, 2014; Published Date: September 03, 2014
Citation: Hancock D, Al-Shaqsi S, Badron M, Rafain NM, Nalankilli K, et al. (2014) The Prevalence of Gluten-Free Diet at the University of Otago: A Cross-Sectional Survey . J Gastroint Dig Syst 4:209. doi:10.4172/2161-069X.1000209
Copyright: © 2014 Hancock D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Aim: The objectives of this study were to: (1) determine the prevalence of the GFD in a New Zealand adult population, (2) investigate the reasons why people are on the GFD and (3) explore what factors limit adherence to the diet.
Methods: This was a cross-sectional online survey of 3,000 students and 3,000 staff at the University of Otago, New Zealand, undertaken in July-August 2013. Participants were randomly selected from databases of students and staff at the University of Otago in July 2013. Survey questions included four main sections: demographics, dietary habits, motivating factors and barriers to following a GFD. The analysis compared the variables between students and staff as well as between people on the GFD and those not on the GFD, using a linear regression analysis model.
Results: The overall response rate was 35.5% (2123 respondents). The prevalence of people currently on the GFD was 6.1% in this university population, while another 6.2% reported having previously tried the GFD. The prevalence of CD was 1.2%. Feeling unwell when eating food that contains gluten was the main reason for following the GFD in our study population. Poor availability along with cost of gluten-free (GF) foods was the main factors limiting adherence to the GFD.
Conclusion: A significant proportion of a New Zealand university population is currently following or has followed a GFD. People follow a GFD for multiple reasons other than medical indications. People with special diets in a university setting appear to have difficulty accessing dietary options.
Keywords
Gluten intolerance; Non celiac-gluten sensitivity; Celiac disease; Gluten-free diet
Introduction
Gluten is a protein complex made up of gliadin and glutenin [1]. It is found in wheat, rye, barley and hybrids of these grains. A Gluten-free diet (GFD) involves completely avoiding ingredients derived from these grains and gluten-containing food additives, as well as food contaminated with gluten [2]. This diet was originally indicated for people with Celiac Disease (CD), a condition first described by Areteus, an ancient Cappadocian physician from Anatolia [1]. In such patients, ingestion of gluten-containing food causes an autoimmune reaction which leads to chronic inflammation of the small intestinal mucosa and atrophy of its villous structures [3,4]. Clinical symptoms of CD include gastrointestinal symptoms such as chronic diarrhoea, abdominal pain and bloating as well as extra-gastrointestinal symptoms (including weight loss, fatigue, myalgia, skin rashes and neurological symptoms) [5]. Removal of gluten from the diet leads to improvement in these symptoms and resolution of the intestinal damage [6]. This intervention was first observed by the Dutch paediatrician, Willem Dicke following the 2nd World War.1 He noted a remarkable improvement in the symptoms reported by his CD patients at the time when wheat was in short supply.
Another group of people following the GFD are those with non-celiac gluten sensitivity (NCGS) [7]. This evolving clinical diagnosis is described as “a condition in which gluten ingestion leads to morphological or symptomatic manifestations despite the absence of CD [8].” Other indications that have been proposed for a GFD include: wheat allergy; lactose-intolerance; systemic lupus erythematosis; irritable bowel syndrome; rheumatoid arthritis; and psoriasis [9-12]. The evidence is equivocal as to whether the GFD improves the symptoms of such diseases.
The prevalence of CD in New Zealand has been reported to be around 1.2% [13]. A similar figure has been observed in studies of adults in other industrialised countries such as Australia, the United States, Europe and the United Kingdom [14-16]. While the increase in prevalence of diagnosed CD has remained relatively consistent there has been a substantial increase in the popularity of the GFD around the world [7,17]. For example, in the United States of America sales of gluten-free products have increased dramatically with a compound annual growth rate of 28% observed between 2004 and 2011 [11,18]. It is possible that the increase in popularity of the GFD is in part due to non-medical factors such as a growth in marketing, celebrity endorsements and people becoming more health conscious.
There is little evidence to suggest any significant health benefits from being on the GFD among individuals without CD. In fact concerns have been raised that the diet may lead to deficiencies in certain nutrients such as thiamin, riboflavin, niacin, folate, and iron [19,20].
Despite this, anecdotal evidence suggests that up to 5% of Australians without CD follow a GFD [21]. Furthermore a cross-sectional survey among a cohort of 916 New Zealand children found that 4.3% avoided gluten without a diagnosis of CD [22]. This could indicate that some people restrict their diet and nutritional supplements without valid medical reason.
There is a lack of data regarding the prevalence of adults following the GFD and the motivating factors behind this. Our study was therefore designed primarily to investigate the prevalence of the GFD among university staff and students. Our secondary aims were to estimate the prevalence of doctor-diagnosed CD (as reported by participants), to establish the reasons why people are on the GFD, and to explore difficulties experienced by those following a GFD in a university setting.
Materials and Methods
Study design
We conducted a cross-sectional online survey of 3,000 staff and 3,000 students at the University of Otago to estimate the prevalence of the GFD in a university setting. In 2013 it had over 25,000 enrolled students and 10,000 staff. The University of Otago is based in the city of Dunedin, but has smaller campuses in Christchurch, Wellington and Auckland. The study received category ethical approval as non-interventional research, from the University of Otago ethics committee. This research was conducted in July and August 2013.
Eligibility
Participants were randomly selected from databases of students and staff at the University of Otago in July 2013. There were 3,000 students across all university campuses and levels of study that were randomly selected from the Student Services database.
At the time of conducting the study, approximately 10,000 staff was affiliated to the University of Otago, although only 4,800 had valid university email addresses, which was a requirement for selection. The rest were casual contractors, student tutors and associate teachers from all over New Zealand affiliated to the college of education. The remainder was full-time and part-time academic and general staff and 3,000 of these staff were randomly selected from the Human Resources database.
Sample size
The sample size of this study was based on the assumption that the prevalence of the GFD is around 5% [22]. We estimated the response rate to the online survey to be 30%. Therefore, our final target sample size was 6,000 to provide sufficient study power to detect a prevalence of 5% GFD and 1% CD.
Survey tool
Survey questions included four main sections: demographics, dietary habits, motivating factors and barriers to following a GFD. There were 19 questions in the format of tick box answers, some of which allowed multiple selections. There was one open-ended qualitative question. The number of questions participants were asked varied depending on whether they were on the GFD, or had previously tried the GFD. The survey questions were uploaded onto a commercially available survey website (www.surveymonkey.com).
To further validate the questionnaire, it was piloted with a sample of 20 potential respondents, and their responses were evaluated to screen for potential problems, such as containing excessive medical jargon, misinterpretation of questions and problems with question prompting/relaying.
Data analysis
Basic characteristics were analysed using descriptive frequencies for categorical variables and means for continuous variables. The statistical significance of differences between the variables was assessed using the Student t-test. Statistical significance was considered to be achieved if the P value was <0.05. The analysis compared the variables between students and staff as well as between people on the GFD and those not on the GFD, using a linear regression analysis model.
Results
Participants
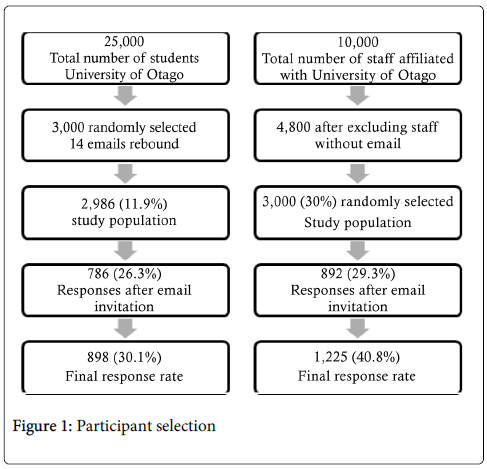
The participants’ selection process is demonstrated in Figure 1.
Baseline demographics
The overall response rate for our study was 35.5% (30.1% among students, 40.8% among staff). The mean age of student participants was 23.9 (SD ± 7.6) years compared to 48.6 (SD ± 10.9) years for staff. New Zealand Europeans constituted 68.8% of students and 82.5% of staff. Table 1 displays the demographic characteristics of participants. The characteristics of gluten-free vs. non-gluten-diet populations are demonstrated in Table 2.
| Student (n=898) | Staff (n=1225) | Overall n=2123 | |
|---|---|---|---|
| Age | 23.9 (SD ±7.6) | 48.6 (SD ±10.9) | 38.2 (SD ±15.6) |
| Gender | |||
| Male | 260 (29.0%) | 427 (34.9%) | 687 (32.4%) |
| Female | 627 (69.8%) | 782 (63.8%) | 1409 (66.4%) |
| Missing | 11 (1.2%) | 16 (1.2%) | 127 (1.2%) |
| Ethnicity | |||
| NZ European/Pakeha | 617 (68.7%) | 1011 (82.5%) | 1628 (76.9%) |
| Maori | 30 (3.3%) | 28 (2.3%) | 58 (2.7%) |
| Pacific people | 15 (1.7%) | 7 (0.6%) | 22 (1%) |
| Asian1 | 139 (15.5%) | 29 (2.4%) | 168 (7.9%) |
| MELAA2 | 15 (1.7%) | 5 (0.4%) | 20 (0.9%) |
| Other | 70 (7.8%) | 127 (10.4%) | 197 (9.3%) |
| Missing | 12 (1.3%) | 18 (1.5%) | 30 (1.4%) |
| Income | |||
| Zero income | 120 (13.4%) | 3 (0.2%) | 123 (5.7%) |
| $1-$10000 | 437 (48.7%) | 2 (0.2%) | 439 (20.7%) |
| $10001-$50000 | 266 (29.6%) | 223(18.2%) | 489 (23.0%) |
| $50001-$100000 | 45 (5.0%) | 630 (51.4%) | 675 (31.8%) |
| $100001 or more | 14 (1.6%) | 338 (27.6%) | 352 (16.6%) |
| Missing | 16 (1.8%) | 29 (2.4%) | 45 (2.1%) |
| Maximum education level | |||
| No secondary or tertiary qualifications | 9 (1.0%) | 15 (1.2%) | 24 (1.1%) |
| Secondary school qualification3 | 506 (56.3%) | 108 (8.8%) | 614 (29.0%) |
| Diploma | 36 (4.0%) | 97 (7.9%) | 133 (6.3%) |
| Bachelor's degree | 219 (24.4%) | 247 (20.2%) | 466 (22.0%) |
| Master's degree | 62 (6.9%) | 187 (15.3%) | 249 (11.7%) |
| PhD | 12 (1.3%) | 412 (33.6%) | 424 (20.0%) |
| Other | 36 (4.0%) | 126 (10.3%) | 162 (7.6%) |
| Missing | 18 (2.0%) | 33 (2.7%) | 51 (2.3%) |
| Response Rate | 898 (30.1%) | 1225 (40.8%) | 2123 (35.5%) |
| Total emails | 2986 | 3000 | 5986 |
Table 1: Baseline characteristics; 1 Including south-east Asian, Indian; 2Middle eastern, Latin American, African; 3Including NZ school certificate, NCEA Level 2/3.
| Gluten Free Diet (n=130) | Non-Gluten Free diet (n=1976) | P value | |
|---|---|---|---|
| Age | 38.1 (SD ±14.5) | 38.2 (SD ±15.6) | 0.9 |
| Gender | <0.005 | ||
| Male | 16 (12.3%) | 671 (34.1%) | |
| Female | 114 (87.7%) | 1296 (65.9%) | |
| Ethnicity | 0.01 | ||
| NZ European/Pakeha | 117 (90.0%) | 1512 (77.0%) | <0.05 |
| Maori | 2 (1.5%) | 56 (2.9%) | 0.06 |
| Pacific people | 0 (0.0%) | 22 (1.1%) | - |
| Asian1 | 0 (0.0%) | 168 (8.6%) | - |
| MELAA2 | 1 (0.8%) | 19 (1%) | 0.02 |
| Other | 10 (7.7%) | 187 (9.5%) | 0.04 |
| Income | 0.08 | ||
| Zero income | 4 (3.0%) | 120 (6.2%) | |
| $1-$10000 | 28 (21.5%) | 411 (21.1%) | |
| $10001-$50000 | 38 (28.9%) | 451 (23.1%) | |
| $50001-$100000 | 47 (36.2%) | 628 (32.2%) | |
| $100001 or more | 13 (10.0%) | 339 (17.4%) | |
| Maximum education level | 0.2 | ||
| No secondary or tertiary qualifications | 1 (0.8%) | 23 (1.2%) | |
| Secondary school qualification3 | 35 (26.9%) | 580 (29.9%) | |
| Diploma | 13 (10.0%) | 120 (6.2%) | |
| Bachelor's degree | 24 (18.5%) | 442 (22.7) | |
| Master's degree | 23 (17.7%) | 226 (11.6%) | |
| PhD | 24 (18.5%) | 400 (20.6%) | |
| Other | 10 (7.7%) | 152 (7.8%) |
Table 2: Gluten Free Diet vs Non-Gluten Free Diet followers baseline characteristics; 1Including south-east Asian, Indian; 2Middle eastern, Latin American, African; 3Including NZ school certificate, NCEA Level 2/3
Prevalence of GFD
Among the 2123 participants (898 students, 1225 staff), 56 students (6.2%) and 74 staff (6.0%) reported currently being on a GFD giving a study population total of 130 (6.1%). Of the remaining 1993 students and staff not on the GFD, 129 (6.5%) reported previously having tried the diet. There is a statistically significant difference in both gender and ethnicity of those on the GFD compared with those who are not, with NZ European/Pakeha women being the most likely group of participants to indicate that they follow a GFD.
Reasons for the GFD
The most common reason for being on a GFD was feeling unwell when eating food that contained gluten, with 89 people (68.5% of the 130 currently on the GFD) experiencing symptoms such as abdominal discomfort, bloating, loose stools and fatigue. Students more commonly reported trying the diet to improve energy levels (37.5%) compared to staff (17.6%). Other common reasons reported by students and staff for following a GFD were: to be healthier (25.3%), a belief that they had gluten intolerance/gluten sensitivity (22.3%), and to lose weight (12.3%). Eight students (0.9%) and 18 staff (1.5%) reported having a doctor confirmed diagnosis of CD, giving a total study population prevalence of 1.2% for CD. A common reason for being on the GFD listed among the 29 (22.3%) who selected “other” was Irritable Bowel Syndrome. These figures are presented in Table 3
| Students n=56 | Staff n=74 | Overall n=130 | |
|---|---|---|---|
| I get unwell when I eat food that contains gluten | 40 (71.4%) | 49 (66.2%) | 89 (68.5%) |
| I think I have CD but not tested for it | 4 (7.1%) | 2 (2.7%) | 6 (4.6%) |
| I think I have gluten intolerance/gluten sensitivity but not tested for it | 12 (21.4%) | 17 (23.0%) | 29 (22.3%) |
| I have a doctor confirmed diagnosis of CD | 8 (14.3%) | 18 (24.3%) | 26 (20%) |
| To improve energy levels | 21 (37.5%) | 13 (17.6%) | 34 (26.1%) |
| To lose weight | 10 (17.9%) | 6 (8.1%) | 16 (12.3%) |
| My friends/family are on it | 5 (8.9%) | 5 (6.8%) | 10 (7.7%) |
| It is cool to be on a diet | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| To be healthier | 17 (30.4%) | 16 (21.6%) | 33 (25.3%) |
| I have food/skin allergy | 11 (19.6%) | 4 (5.4%) | 15 (11.5%) |
| Personal beliefs | 4 (7.1%) | 2 (2.7%) | 6 (4.6%) |
| Other | 12 (21.4%) | 17 (23.0%) | 29 (22.3%) |
Table 3: Reasons for being on the GFD
Barriers to following a GFD
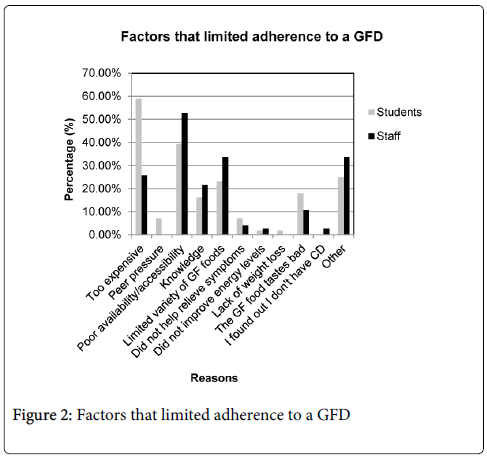
The most common barrier to following the GFD for students was expense, with 33 students (58.9%) stating this was a limiting factor compared to 19 staff (25.7%). Poor availability of gluten-free food was more commonly listed as a problem for staff (52.7%) than for students (39.3%). Limited variety of gluten-free food was a factor for 13 students (23.2%) and 25 staff (33.8%). Students and staff also put gluten-free food tastes bad as one of the limiting factors to following a GFD as shown in Figure 2.
Discussion
Prevalence of the GFD
In this study the estimated prevalence of the GFD among university students and staff was 6.1%. This estimate is marginally higher than the prevalence of 5.2% that was reported in a recent nested cohort study of New Zealand children [22]. While their study population was restricted to children, the present study looks at the New Zealand adult population. Therefore the difference in average age of study populations may account for the variation seen in GFD prevalence. The reported prevalence in this study may be an overestimate as higher levels of education are associated with more health conscious behavior [23]. The study sample (having been selected from a university population) has a significantly higher level of education than that the wider public and therefore, it is likely that the reported prevalence might be different from that of the general population. However among the study participants, maximum level of education and income did not appear to be associated with being on a GFD. We found that the GFD was prevalent among low and high income students and staff.
Reasons for the GFD
The main reason reported by study participants for being on a GFD was because gluten made them unwell. Two thirds of those on the diet reported that gluten gave them some of the following symptoms: abdominal discomfort, bloating, loose stools and fatigue. It is also interesting to note that of the 130 people in our study who reported being on a GFD only 26 (20%) reported having doctor confirmed CD. This raises concern that there are a significant number of people who may be going undiagnosed with gluten-sensitivity or CD. A study by Biesiekierski et al. indicated that a significant number of GF followers adhere to a GFD without scientific testing for CD and this restrictive diet could harm their health.12 The prevalence of CD in this study is 1.2%, which could be an over-representation given that previous studies have estimated that only 15%-20% of CD patients have a confirmed diagnosis [24,25]. This could again reflect the high educational level among university sample compared to the general population. University participants are likely to seek medical attention for their symptoms and therefore more likely to be tested and diagnosed with CD. In fact 29 people (22.3%) on the GFD suspected they had gluten intolerance/sensitivity but had no medical investigation for it. Other common reasons for the diet were to improve energy levels (26.1%), to be healthier (25.3%), and to lose weight (12.3%). Shepherd and others identified a multitude of reasons for why people might follow GFD other than CD. Their study also highlighted that there might be a spectrum of other sensitivities and gastrointestinal symptoms that improve by avoiding gluten-containing foods [26].
While the GFD has been endorsed in the popular media by celebrities for some of the reasons above there is little or no scientific evidence to support these claims. In fact restricting gluten from a diet in people without CD or gluten-sensitivity may be harmful. Gluten has been reported to improve blood lipid levels, lower blood pressure, improve immune system function and possibly reduce the risk of cancer [9]. Conversely there are recognised long term nutritional complications of being on a GFD with deficiency in thiamin, folate, vitamin A, magnesium, calcium, iron and fibre intake observed.27 A possible explanation for this is that commercially available GF foods are often high glycaemic index, not commonly fortified and contain less fibre than equivalent non GF foods [27]. For this reason it is important that doctors and individuals considering or currently on the GFD are well informed of the possible risks and benefits and appropriate investigations are done when required.
Factors that limit adherence to a GFD
This study highlights the barriers to compliance experienced by followers of a GFD. Participants reported that the greatest limitations to following a GFD included: poor availability to gluten-free food (46.9%). This replicates the findings of a study of college students in the United States of America where 9 of 21 students (43%) interviewed mentioned access to GF foods as one of the challenges to following the diet.28 The variety of gluten-free foods (29.2%), knowledge of which foods contain gluten (19.2%) and gluten-free food tasting bad (13.8%) were are also reported to be significant limiting factors for people following a GFD.
An interesting difference in reported barriers to following a GFD between students and staff was cost. 58.9% of students compared to 25.7% of staff rated expense as one of the factors that limited their ability to follow the diet. This is likely a reflection of the average annual income of staff being greater than that of students. The result for staff is consistent with a study done in Boston in 2007 which found that cost limited adherence in 24.7% of people with CD.
While this study examined a university population it is likely that similar factors limit adherence to the GFD in the rest of the New Zealand adult population. Research in Boston found that demographic factors such as age, gender, and level of education were not correlated with adherence [28,29].
Strengths and limitations
This original study identifies the prevalence of the GFD as well as factors that influence New Zealand adults to follow a GFD. To our knowledge this is also the first study to compare student and staff populations in the university setting. This study achieved an overall response rate of 35.5%. The literature suggests that while online surveys are quick, inexpensive, and allow for large sample sizes they are typically associated with lower response rates than more traditional survey methods. A possible explanation for this is the phenomenon called “research fatigue” [30]. The modest response rate could have resulted in an overestimate of the true prevalence of the GFD, however people were asked to complete the survey without specifically knowing it was about gluten in the hope of mitigating this. The results are consistent with previous studies conducted in New Zealand and internationally [11,22]. An inherent limitation of cross sectional studies is reliance on self-report therefore the quality and accuracy of the data presented is determined by respondents’ honesty.
This study found that 6.1% of university population was on the GFD while only 1.2% had self-reported doctor confirmed CD. It is of some concern therefore that two thirds of those following the GFD do so because of symptoms such as abdominal discomfort, bloating, loose stools, and fatigue but would seem not to have been medically investigated. Those following a GFD make up a significant dietary minority of a university population. It is imperative that further work is done to educate the general population on what CD is and the importance of seeking medical attention if experiencing symptoms that may be related to gluten ingestion before starting on a GFD. While the university population is not demographically representative of the New Zealand adult population the authors believe that the study’s findings are comparable to other studies conducted both in New Zealand and internationally. Further research is required in the field NCGS in the form of high quality, reproducible studies to firstly confirm the existence and accurately define this entity. Improved diagnostic criteria will allow more accurate quantification of the disease burden in New Zealand.
Acknowledgment
The authors wish to disclose no conflict of interest. This research was conducted without any external financial support. We would like to acknowledge the support and participation of the University of Otago students and staff.
References
- Sapone A, Lammers KM, Mazzarella G, Mikhailenko I, Cartenì M, et al. (2010) Differential mucosal IL-17 expression in two gliadin-induced disorders: gluten sensitivity and the autoimmune enteropathy celiac disease.Int Arch Allergy Immunol 152: 75-80.
- El-Chammas K, Danner E (2011) Gluten-free diet in nonceliac disease.NutrClinPract 26: 294-299.
- Green PH, Rostami K, Marsh MN (2005) Diagnosis of coeliac disease.Best Pract Res ClinGastroenterol 19: 389-400.
- Murray JA, Van Dyke C, Plevak MF, Dierkhising RA, Zinsmeister AR, et al. (2003) Trends in the identification and clinical features of celiac disease in a North American community, 1950-2001.ClinGastroenterolHepatol 1: 19-27.
- Hopper AD, Hadjivassiliou M, Butt S, Sanders DS (2007) Adult coeliac disease.BMJ 335: 558-562.
- Rashid M, Butzner JD, Warren R, Molloy M, Case S, et al. (2009) Home blood testing for celiac disease: recommendations for management.Can Fam Physician 55: 151-153.
- Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, et al. (2012) Spectrum of gluten-related disorders: consensus on new nomenclature and classification.BMC Med 10: 13.
- Ludvigsson JF, Leffler DA, Bai JC, Biagi F, Fasano A, et al. (2013) The Oslo definitions for coeliac disease and related terms.Gut 62: 43-52.
- Green PH (2009) Mortality in celiac disease, intestinal inflammation, and gluten sensitivity.JAMA 302: 1225-1226.
- Gaesser GA, Angadi SS (2012) Gluten-free diet: imprudent dietary advice for the general population?J AcadNutr Diet 112: 1330-1333.
- Wahnschaffe U, Schulzke JD, Zeitz M, Ullrich R (2007) Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome.ClinGastroenterolHepatol 5: 844-850.
- Biesiekierski JR, Muir JG, Gibson PR (2013) Is gluten a cause of gastrointestinal symptoms in people without celiac disease?Curr Allergy Asthma Rep 13: 631-638.
- Cook HB, Burt MJ, Collett JA, Whitehead MR, Frampton CM, et al. (2000) Adult coeliac disease: prevalence and clinical significance.J GastroenterolHepatol 15: 1032-1036.
- Cummins AG, Roberts-Thomson IC (2009) Prevalence of celiac disease in the Asia-Pacific region.J GastroenterolHepatol 24: 1347-1351.
- Dubé C, Rostom A, Sy R, Cranney A, Saloojee N, et al. (2005) The prevalence of celiac disease in average-risk and at-risk Western European populations: a systematic review.Gastroenterology 128: S57-67.
- Pietzak M (2012) Celiac disease, wheat allergy, and gluten sensitivity: when gluten free is not a fad.JPEN J Parenter Enteral Nutr 36: 68S-75S.
- Marcason W (2011) Is there evidence to support the claim that a gluten-free diet should be used for weight loss?J Am Diet Assoc 111: 1786.
- Niewinski MM (2008) Advances in celiac disease and gluten-free diet.J Am Diet Assoc 108: 661-672.
- Case S (2006) Gluten-Free Diet: A Comprehensive Resource Guide. Regina, Saskatchewan, Canada Case Nutrition Consulting.
- Long KH, Rubio-Tapia A, Wagie AE, Melton LJ 3rd, Lahr BD, et al. (2010) The economics of coeliac disease: a population-based study.Aliment PharmacolTher 32: 261-269.
- Financial Review Food fadism: exposing the gluten mytha
- Tanpowpong P, Ingham TR, Lampshire PK, Kirchberg FF, Epton MJ, et al. (2012) Coeliac disease and gluten avoidance in New Zealand children.Arch Dis Child 97: 12-16.
- Mechanic D, Cleary PD (1980) Factors associated with the maintenance of positive health behavior.Prev Med 9: 805-814.
- El-Hadi S, Tuthill D, Lewis E, Adisesh A, Moody M, et al. (2004) Unrecognised coeliac disease is common in healthcare students.Arch Dis Child 89: 842.
- Cooper GS, Bynum ML, Somers EC (2009) Recent insights in the epidemiology of autoimmune diseases: improved prevalence estimates and understanding of clustering of diseases.J Autoimmun 33: 197-207.
- Shepherd SJ, Lomer MC, Gibson PR (2013) Short-chain carbohydrates and functional gastrointestinal disorders.Am J Gastroenterol 108: 707-717.
- Shepherd SJ, Gibson PR (2013) Nutritional inadequacies of the gluten-free diet in both recently-diagnosed and long-term patients with coeliac disease.J Hum Nutr Diet 26: 349-358.
- Panzer RM, Dennis M, Kelly CP, Weir D, Leichtner A, et al. (2012) Navigating the gluten-free diet in college.J PediatrGastroenterolNutr 55: 740-744.
- Leffler DA, Edwards-George J, Dennis M, Schuppan D, Cook F, et al. (2008) Factors that influence adherence to a gluten-free diet in adults with celiac disease.Dig Dis Sci 53: 1573-1581.
- Porter SR, Whitcomb ME, Weitzer WH. Multiple surveys of students and survey fatigue. New Directions for Institutional Research 121: 63-73.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14627
- [From(publication date):
August-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10054
- PDF downloads : 4573