The Prevalence of Breast Cancer in Patients of a Mastology Clinic from an Amazonian Hospital
Received: 28-Aug-2019 / Accepted Date: 06-Sep-2019 / Published Date: 14-Sep-2019 DOI: 10.4172/2165-7386.1000362
Abstract
Introduction: Breast cancer is the second most prevalent malignancy occurring in women worldwide, and due to its prevalence, it is accountable for the majority of deaths among Brazilian women. Hence, this study aimed to assess the prevalence of breast cancer among patients from the Mastology clinic from a referral hospital in the state of Amapá in 2017.
Materials and methods: It was performed a retrospective, quantitative, and descriptive study from medical records of patients diagnosed with breast cancer in the Mastology clinic from the Alberto Lima Clinics Hospital (UNACON). The variables assessed included socio demographic data, personal information, and the diagnostic methods from the medical record of the patients, and the statistical analysis was performed using the software Bioestat version 5.3. The correlation between variables was assessed using the Chi-square test (C2=0.05), and the significance level was set at as p=0.05.
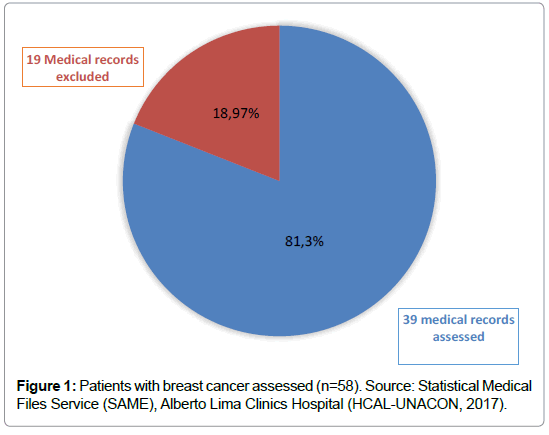
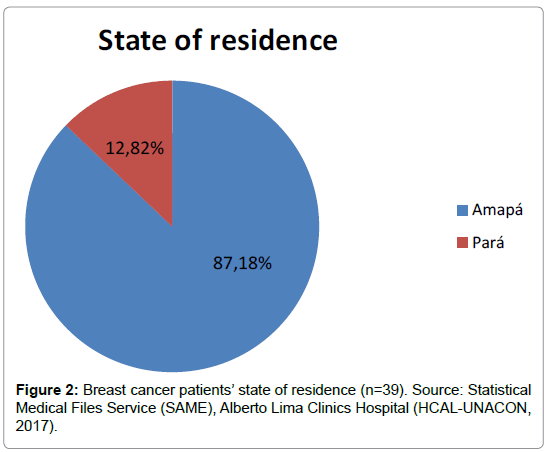
Results: A total of 58 patients were assessed, where 39 of them were included in the study and 19 were excluded due to the lack of information or death; the majority of patients were from the State of Amapá (81.3%), with age ranging from 30 to 89 years old, as for colour/race, 51.28% of the patients were white, 100% of them were not alcoholic, the most part had a low education level (58.98%), menarche after 12 years old (100%) and menopause (53.85%). All of the patients breastfed (100%), and only one (2.56%) had hormone replacement; and 100% of them had ultrasound and biopsy.
Conclusion: The results evidence the need of public politics in the prevention, more considerable attention, and improvement in women care in order to achieve earlier diagnoses.
Keywords: Breast cancer; Histo-pathological diagnosis; Mortality; Women
Introduction
Breast cancer represents the primary cause of death among Brazilian women, and the chances to have 57,000 new cases in 2018 are estimated around 29.5% [1]. Among the general population, the risk of acquiring breast cancer throughout life is about 8%, that is, one in twelve women are expected to develop this disease in its life. This probability is known as the basal risk among the female population, losing only to lung cancer, and hence, it represents a significant public health issue around the world.
Risk factors associated with breast cancer development include advanced age, reproductive characteristics, family and personal history, lifestyle and environmental influences. The reproductive risk characteristics are based on oestrogen-dependent disease [2] and include early menarche, late menopause, first pregnancy after 30 years and nuliparity [3]. Breastfeeding, contraceptive use and hormone replacement therapy (HRT) after menopause are still controversial [3].
The importance of family and personal screening includes: one or more first-degree relatives with breast cancer before age 50, one or more first-degree relatives with bilateral breast cancer or ovarian cancer at any age, relative to male breast cancer, previous breast cancer and/ or benign breast disease. Related lifestyle habits are obesity, regular alcohol use above 60 grams per day, and the influence of smoking [2].
The mammary neoplasia is possibly the most feared cancer among women since its occurrence brings psychological, functional, and social impact, having a detrimental effect regarding the patients’ self-image and sexuality [4]. The main features and symptoms of breast cancer are lumps found in the breasts or armpits, breast pain, and modifications in the breast skin, such as bulging and retractions, similar to an orange peel. The cancer is usually located in the upper-outer quadrant and the lesions are painless, fixed, with jagged edges and accompanied by skin changes in advanced stages [5].
To date, the most effective way for earlier detection of the disease is clinical breast examination and mammography. The breasts selfexamination detects the disease in advanced stages, and is accountable for 80% of breast cancer discovery [5]; the mammography, in turn, is a radiological exam of breasts soft tissues, performed in women with 35 years old or older, in order to visualize changes not detected by clinical breast examination.
Another method used is ultrasonography, which is the first-choice exam for young and pregnant women with breasts symptoms such as inflammation, dense breasts, and palpable nodules, with or without negative mammogram [6]. Considering the information given, this study aimed to assess the prevalence of breast cancer among patients from the Mastology clinic from a referral hospital in the state of Amapá, in the period of 2017.
Methodology
In this study was performed a retrospective, quantitative, and descriptive research from the Alberto Lima – Amapá Clinics Hospital. Data from patients treated in 2017 at the UNACON Mastology service of the referred hospital were analyzed.
This year 4084 patients were treated in the Mastology sector. Of this total, through research in the SAME (medical archive service) and in the medical records, 58 patients with breast cancer were diagnosed.
The inclusion criteria were of patients above 18-year-old diagnosed with breast cancer. From these were excluded patients with benign nodules, incomplete medical record, male patients, patients without histo-pathological diagnostic, and patients who had passed away. From the 58 medical records analyzed, only 39 met the study criteria. Through a spreadsheet, epidemiological and socio-demographic data were collected in order to build a profile of breast cancer patients.
The data acquired was assessed with the software Biostat version 5.3. The tables and graphs were built with the software Microsoft Excel and the following variables were analyzed: age of the patient, menarche, parity, type of childbirth, menopause, smoking, alcoholism, birthplace, breastfeeding, schooling, ultrasound and histopathology diagnostic. Correlations between variables were measured through the Chi-square test (C2=0.05), and the significance level was p=>0.05.
The present study was approved by the Research Ethics Committee of the Federal University of Amapá (UNIFAP) and by the Research Ethics Committee of the Dr. Alberto Lima Clinical Hospital, in the city of Macapá-AP.
Results and Discussion
In 2017 were performed 4,084 attendances in the mastology clinic from the referral hospital assessed in this study. Among the medical records evaluated, there were a total of 58 patients (57 female patients and 1 male patient) diagnosed with breast cancer, corresponding to 1.42% of the total attendances. About 11 medical records were excluded due to the lack of information, and eight patients (6.5%) had passed away.
Regarding the place of residence of breast cancer patients, it was found that the majority, 34 patients (87%) reside in the State of Amapá and 12.82% were from the State Pará (which borders Amapá) (Figures 1 and 2).
The patients with breast cancer ranged from 30 to 89 years, with the predominant and statistically significant age group (p=0.01), and the vast majority, 35 patients (90%), were 40 years old or older, corroborating the advanced age information as a risk factor for the disease (Table 1). In accordance with the results observed in this study, the National Institute of Cancer states that age is still one of the most critical risk factors for the development of breast cancer. The incidence rates rapidly increase until 50 years old. After this age, the incidences occur slower, evidencing the role of the female hormones in the etiology of this disease [4].
| Age range | Number(N) | Percentage (%) | p-value |
|---|---|---|---|
| 30-39 | 4 | 10% | 0.01 |
| 40-49 | 15 | 38% | |
| 50-59 | 8 | 21% | |
| 60-69 | 8 | 21% | |
| 70-79 | 3 | 8% | |
| 80-89 | 1 | 2% |
Table 1: Age range of patients diagnosed with breast cancer (n=39). Source: Statistical Medical Files Service (SAME), Alberto Lima Clinics Hospital (HCALUNACON, 2017).
In the study of Soares et al. [7], 54.5% of the patients were above 50 years old; in their study, there was no association shown between the cancer staging and the diagnostic, and this is in accordance with our study since most patients were above the 50 years.
Although breast cancer is uncommon in young women, 4 (10%) patients under 40 years of age were found in the present study. Other studies, however, suggest that breast cancer in young women has a more aggressive physiopathology, evidencing more advanced stages, and compared to the tumours of older women, the prognosis is worse (Table 1) [8].
The socioeconomic data of the research reveals that the majority of women were white (51.28%), followed by brown (43.59%), and black (5.13%). Hence, there was a statistically significant difference in the incidence of breast cancer according to the race (p=0.01). As for the schooling level, only 12.82% of the women had higher education, which is the same percentage of women who did not finish the high school; however, there was no statistical difference regarding the schooling level (p=0.161) (Table 2).
| Socio-demografic data | *N | Percentage (%) | P value | ||||
|---|---|---|---|---|---|---|---|
| Color/race | 0.001 | ||||||
| White | 20 | 51.28% | |||||
| Brown | 17 | 43.59% | |||||
| Black | 2 | 5.13% | |||||
| Schooling level | 0.161 | ||||||
| Incomplete fundamental education | 5 | 12.82% | |||||
| Complete fundamental education | 13 | 33.34% | |||||
| Incomplete high school | 5 | 12.82% | |||||
| Complete high school | 6 | 15.38% | |||||
| Complete superior education | 5 | 12.82% | |||||
| Illiterate | 5 | 12.82% | |||||
| Professor | 0.423 | ||||||
| Housewife | 22 | 56.41% | |||||
| Employed | 17 | 43.59% | |||||
Table 2: Characterization of patients according to socio demographic data (n=39). Source: Statistical Medical Files Service (SAME), Alberto Lima Clinics Hospital (HCAL-UNACON, 2017).
According to Dugno et al. [9], white women represented 92.7% of the patients in its study performed in Caxias do Sul, similar to the study of Campana et al. [10], where 80% of the women were white. The majority of women, 58.98%, were of low schooling (complete or incomplete fundamental education) or had no schooling at all. According to Mourão et al. [11], the low schooling can be accountable for the lack of information and knowledge about the prevention and earlier detection methods of breast cancer, also, the difficulty on access to basic health care (Table 2).
Among the factors predisposing for cancers in general (Table 3), tobacco is pointed out as a high-risk factor for the development of the disease [12]. About 42.03% of the patients in our study stated that they smoke. This is in accordance with the study of Rêgo et al. [13], where most of the patients were non-smokers. Hence, in this study, smoking was not a statistically significant factor for the occurrence of the disease (p=0.262).
| Factors | *N | Percentage (%) | p value | ||||
|---|---|---|---|---|---|---|---|
| Smoking | 0.262 | ||||||
| Yes | 16 | 42.03% | |||||
| No | 23 | 58.97% | |||||
| Alcoholism | <0.001 | ||||||
| Yes | 0 | 0% | |||||
| No | 39 | 100% | |||||
| Social drinking | 0.423 | ||||||
| Yes | 17 | 43.59% | |||||
| No | 22 | 56.41% | |||||
Table 3: Some of the risk factors for breast cancer (n=39). Source: Statistical Medical Files Service (SAME), Alberto Lima Clinics Hospital (HCAL-UNACON, 2017).
Alcoholism is also pointed as a high risk factor for the development of cancer, but it was not shown to be a predominant factor among women, but it is supposed to contribute as an additional factor for the development of breast cancer in women in question [9]. However, no patient reported having this addiction, 56.41% claim not to drink alcohol, being similar to the study conducted at the Hospital in the city of Macapá in which around 62.5% of patients said not to drink alcohol [13].
According to Dugno et al. [9], the ingestion of alcohol is proportionally associated with the development of breast cancer, that is, the more the patient consumes alcohol, the higher the chances of acquiring the disease. When ethanol is consumed, it can act as a mutagenic agent through its metabolite acetaldehyde, which in turn, can increase the serum levels of oestrogen and the transcription activity of the estrogen receptor, increasing the response of the cells to the action of this hormone (Table 3) [14].
In this study, the menarche of the patients occurred in the average of 12.8 years old (the ages ranged from 11 to 17 years old), and early menarche occurred only in 35.90% of the cases, 14 patients, as shown in Table 4.
| Factor | *N | Percentage (%) | p value |
|---|---|---|---|
| Menarche | 0.078 | ||
| <12 years old | 14 | 35.90% | |
| >12 years old | 25 | 64.10% | |
| Menopause | 0.631 | ||
| Yes | 21 | 53.85% | |
| No | 18 | 46.15% | |
| Menopause age range | 0.009 | ||
| 55-59 years old | 2 | 9.52% | |
| 50-54 years old | 7 | 33.33% | |
| 45-59 years old | 9 | 42.86% | |
| 40-45 years old | 3 | 14.29% | |
| Type of childbirth | <0.001 | ||
| Natural | 32 | 94.80% | |
| Cesarean | 2 | 5.20% | |
| Parity | <0.001 | ||
| Nulligesta | 5 | 12.82% | |
| Not multiparous | 5 | 12.82% | |
| Multiparous | 29 | 74.36% | |
| Breastfeeding | <0.001 | ||
| Yes | 34 | 100% | |
| No | 0 | 0% | |
| Breastfeeding time | <0.001 | ||
| <6 months | 5 | 12.82% | |
| 6 months – 1 year | 4 | 10.26% | |
| >1 year | 25 | 76.92% | |
| Hormone replacement therapy | <0.001 | ||
| Yes | 1 | 2.56% | |
| No | 38 | 97.44% | |
Table 4: Data regarding menarche, menopause, type of childbirth, parity, breastfeeding, and hormonal reposition therapy (n=39). Source: Statistical Medical Files Service (SAME), Alberto Lima Clinics Hospital (HCAL-UNACON, 2017).
It is noteworthy that early menarche (before 12 years) is considered a risk factor due to the higher exposure to oestrogen in this period. In fact, not only early menarche but long ovarian period and late menopause also are associated with a higher risk of developing breast cancer [4]. Decarli et al. estimated a 4.7% decrease in the chances of acquiring breast cancer for each year that the menarche is late [15]. A fertile period of 30 years or more is considered a risk factor that increases twice the chances of breast cancer.
From the total number of patients, 53.85% (21 women) had already reached the menopause, and 46.18% (women) did not, and there was no significant difference between these number (p=0.631). As for the age range of the menopause (Table 3), only two women (9.52%) had late menopause, which is not in agreement with the risk factors established in the literature and by INCA. The majority of patients had menopause between 45 and 59 years (42.8% and p=0.09), which is statistically significant for higher rates of breast cancer.
In this study, 94.8% of the patients had natural childbirths, while 5.2% had cesarean, and about 34 (86.82%) of the patients had at least one pregnancy and 5 patients (12.82%) never had children as shown in Table 4. According to Thuler [16], late first pregnancy is a not modifiable factor that increases the risk of developing breast cancer and null parity, or lack of pregnancy, also is considered as an important factor in the development of breast cancer. In our study, 74.3% of the women were multiparous (p=0.001), similar to the report of Oliveira et al. [17], where 81.9% of the patients had children and acquired breast cancer.
Considered a protection factor when performed for at least six months [14], all of the patients claimed to have breastfed their children. The period of breastfeeding was below six months for five women (12.8%), between six months and one year for four women, and 25 (76,9%) of them breastfed during a period of one to three years (Table 4).
Tessaro et al. [18] in a control case study performed in the south of Brazil also reported in their results that breastfeeding did not exert a protector effect against breast cancer, which is in accordance with our study; despite the literature relate that breastfeeding has a potential role in decreasing the incidence of this cancer. In our study 76.9% of breast cancer patients breastfed for more than 1 year (p=0.001), breastfeeding was not a protective factor. Only one patient of this study used hormone replacement therapy (HRT) with oestrogen, a hormone with an important role in the development of breast cancer since it induces the growth of cells from the breast tissues (Tables 4 and 5) [4].
| Factors | *N | Percentage (%) | P value |
|---|---|---|---|
| Nodule detection method | 0.631 | ||
| Self-exam | 21 | 53.85% | |
| Imaging exam | 18 | 46.15% | |
| Complementary exams | <0.001 | ||
| Mammography | 39 | 100% | |
| Biopsy | 39 | 100% | |
| BI-RADS classification | <0.001 | ||
| BI-RADS I | 1 | 2.56% | |
| BI-RADS II | 4 | 10.27% | |
| BI-RADS III | 0 | 0% | |
| BI-RADS IV | 18 | 46.15% | |
| BI-RADS V | 15 | 38.46% | |
| BI-RADS VI | 1 | 2.56% | |
| Histological classification | <0.001 | ||
| Grade 1 invasive ductal carcinoma | 7 | 17.95% | |
| Grade 2 invasive ductal carcinoma | 21 | 53.85% | |
| Grade 3 invasive ductal carcinoma | 6 | 15.38% | |
| Poorly differentiated carcinoma with solid morphological appearance: 1 | 1 | 2.56% | |
| Grade 1 residual invasive lobular carcinoma | 3 | 7.70% | |
| In situ papilliferous carcinoma | 1 | 2.56% | |
Table 5: Methods of nodule detection, complementary exams, ultrasound, and histological classification (n=39). Source: Statistical Medical Files Service (SAME), Alberto Lima Clinics Hospital (HCAL-UNACON, 2017).
Most of the women from this study (53.85%) reported that observed the breast lump through the breast self-examination – BSE. The other patients, around 46.15%, detected the nodule through imaging exam and all the 39 women performed mammography and biopsy (Table 5). Regarding the diagnosis, the self-exam is considered an essential tool for early detection of mammary changes. Hence, it is emphasized the need for information and education projects, always respecting the privacy of the patients [19]. According to Vicelli [20], the efficacy detecting nodules with a smaller diameter is superior when compared to the clinical exam of the breast since 87% of the patients in its study had suspicious nodules that only were observed through mammography.
As shown in Table 5, 18 patients had BI-RADS IV (46.1%), 15 patients had BI-RADS V (38.4%), and one patient had BI-RADS VI (2.5%). Despite the recommendation that biopsies should be performed only in samples classified as BI-RADS IV and V, in this study was observed that four patients had mammography labelled as BI-RADS II; hence, 87% of the patients had BI-RADS IV or higher (p=0.001). There are some exceptions for this rule, for instance, when the nodule shows features indicating malignancy (skin like, similar to an orange peel, secretions, and nodules suspicious of malignancy), it will be performed biopsy even if it is not labelled as BI-RADS V or higher [21].
Regarding the histology, the results of the study show seven patients (17.95%) were diagnosed with grade 1 invasive ductal carcinoma, which is the most common breast cancer. This type of cancer is characterized by starting at the milk ducts, followed by disrupting its wall and development in nearby tissue, then, it can spread through metastasis toward other organs. According to Galea [22], the histological grade has relevant prognosis either being independent or associated with the lymph node stage and tumour size, as established by the prognostic index of Nottingham 2.
About 53.85% of the patients from this study had grade 2 invasive ductal carcinoma, corresponding to 21 women (p=0.001), which is statistically significant compared to the total sample size. In grade 3, the cancerous cells are of fast progression and were identified in 15.38% (six) of the patients. One patient was diagnosed with poorly differentiated carcinoma with solid morphological appearance, corresponding to 2.56% of the total. Moreover, three women (7.70%) were diagnosed with grade 1 residual invasive lobular carcinoma, and one woman (2.56%) was diagnosed with in situ papilliferous carcinoma.
Henson et al. [23] observed that 99% of the patients had favourable prognosis when the tumours were of grade 1 and smaller than 2 cm of diameter; these patients had an average survival of 5 years, even if they had positive armpit lymph nodes.
Despite the relevance of this study, due to the analysis of epidemiological data of a serious and frequent disease in the northern region of Brazil, the main limitations were the difficulty of obtaining all data due to failures in filling out medical records. One suggestion is to standardize the first consultation form with a list of epidemiological information and socioeconomic data and follow-up appointments to have a table to insert histo-pathological diagnosis, treatments and results (cure or recurrence or death).
Conclusion
The socio-demographic profile shows that the majority of women had low schooling level (46.1%), aged between 40 and 49 years old (38%), were white (51%), reached the menopause (53.8%), were multiparous (74.3%), non-smoking (58.9%), and breastfed for more than a year (76.9%); these women were, on average, more affected by breast cancer. All the patients had performed mammography; in 87% of the cases it was reported BI-RADS IV or higher, and the diagnosis was confirmed by biopsy and histopathology (53.8% of grade 2 invasive ductal carcinoma). However, from the results of this study, it was observed that some risk factors of the literature were refuted, such as the parity, breastfeeding, ingestion of alcoholic drinking, and smoking.
References
- Ministry of Health, National Cancer Institute (INCA) (2018) Incidence of Cancer in Brazil.
- Cantinelli FS, Camacho RS, Smaletz O, Gonsales BK, Braguittoni E et al. (2006) Oncopsychiatry in breast cancer: considerations regarding women's issues Rev Psiquiatr ClÃn 33: 124-133.
- Ministry of Health, National Cancer Institute (INCA) (2002). Talking about breast cancer, Rio de Janeiro.
- Ministry of Health. National Cancer Institute (INCA) (2014) Breast cancer: it is needed to talk about it.
- Migowski A. et al.(2018) Guidelines for early detection of breast cancer in Brazil. III Challenges of implantation. Public Health Notebook. 34: e00074817.
- Siegel RL, Miller KD, Jemal A (2017) Cancer Statistics, 2017. CA Cancer J Clin 67:7-30.
- Soares BM, Filho SQ, Souza PW, Gonçalves RCR, Martelli DRB et al. (2012) Characteristics of women with breast cancer assisted in referral services from the North of Minas Gerais. Rev Bras Epidemiol 15: 595-604.
- Castiglione M, Aebi S (2006) The enigma of young age. Ann Oncol 17: 1475-1477.
- Dugno GLM (2014) Breast cancer profile and its relation to clinical staging in a hospital from the South of Brazil. Brazilian J Oncol 10: 60-66.
- Campana HCR (2007) Profile of women with breast cancer. Maringá: State University of Maringá..
- Mourão CML et al. (2008) The profile of breast cancer patients in a referral hospital from Ceará. Rev RENE 9: 47-53.
- Do Rêgo AD, Machado GLD, de Almeida SC, Ribeiro AC, Corrêa NCA, et al. (2017) Quality of Life Outcomes in Patients with Breast Cancer in an Amazon City: The Impact of Breast Reconstruction. J Palliat Care Med 7: 317.
- Inumaru LE, Silveira EA, Naves MMV (2011) Risk and protective factors for breast cancer: a systematic review. Cad Saude Publica 27: 1259-1270.
- Decarli A, La Vecchia C, Negri E, Franceschi S (1996) Age at any birth and breast cancer in Italy Int J Cancer 67: 187-189.
- Thuller LC (2003) Considerations about the prevention of women breast cancer. Brazilian Journal of Cancerology 49: 227–238.
- Oliveira MMC, Torrezan C, Oliveira SFV, Torrezan GT, Abuazar CS et al. (2009) The epidemiology of breast câncer in patients from the South of Brazil. Paulista Epidemiology Bulletin 18: 146-157.
- Tessaro S, Beria JU, Tomasi E, Victora CG (2003) Breastfeeding and breast cancer: a control case study in the south of Brazil. Cad Saude Publica 19:1593-1601.
- Silva PA, Riul SS (2010) Breast cancer: risk factors and early detection. Brazilian Journal of Nursery 64:1016-1021.
- Vicelli JT (1999) The performance of mammography in the diagnosis of cancer in women from 35 to 50 years old. State University Campinas. p. 112.
- Ministry of Health. National Cancer Institute (INCA) (2002) Coordination of Prevention and Vigilance – Conprev. Speaking About Breast Cancer.
- Galea MH, Blamey RW, Elston CE, Ellis IO (1992) The Nottingham Prognostic Index in primary breast cancer. Breast Câncer Res Treat 22: 207-219.
- Henson DE, Ries L, Freedman LS, Carriaga M (1991) Relationship among outcome, stage of the disease, and histologic grade for 22,616 cases of breast cancer. The basis for a prognostic index Cancer 68:2142-2149.
Citation: de Sousa Almeida A, do Rêgo AD, do Socorro Gonçalves Farias Rêgo L (2019) The Prevalence of Breast Cancer in Patients of a Mastology Clinic from an Amazonian Hospital. J Palliat Care Med 6:362. DOI: 10.4172/2165-7386.1000362
Copyright: © 2019 de Sousa Almeida A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2480
- [From(publication date): 0-2019 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 1732
- PDF downloads: 748