The Pattern of Neurological Emergencies: Frequency, Etiology and Outcome, for Patients Admitted to Intensive Care Unit at Khartoum State Hospitals
Received: 15-Dec-2023 / Manuscript No. JADP-23-122874 / Editor assigned: 18-Dec-2023 / PreQC No. JADP-23-122874 (PQ) / Reviewed: 01-Jan-2024 / QC No. JADP-23-122874 / Revised: 08-Jan-2024 / Manuscript No. JADP-23-122874 (R) / Published Date: 15-Jan-2024 DOI: 10.4172/2161-0460.1000590
Abstract
Background: Neurological emergencies are frequent presentations and often end with devastating short and long term consequences. Neurological disorders are increasingly prevalent in Sub-Saharan Africa with paucity of data on adult neurological emergencies in our context.
Methods: A prospective cross-sectional study enrolled 103 patients with neurologic emergencies admitted to Intensive Care Unit (ICU) Khartoum state intensive care departments during the period from October 2019 to April 2020. Data regarding demographics, presentations, clinical examinations, laboratory investigations, indications of ICU admission, diagnosis of neurological conditions, length of ICU stay, patterns of medications and outcomes were collected. Data was analyzed by using Statistical Package for the Social Sciences (SPSS) v. 21.0.
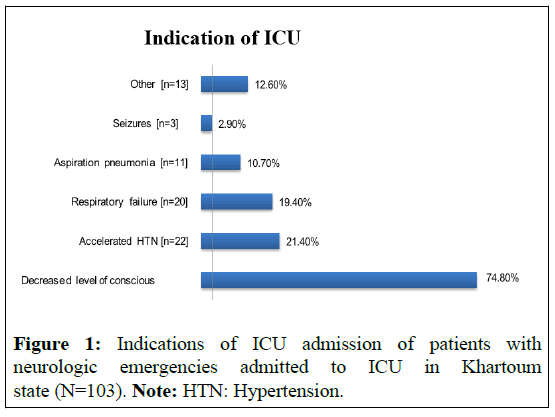
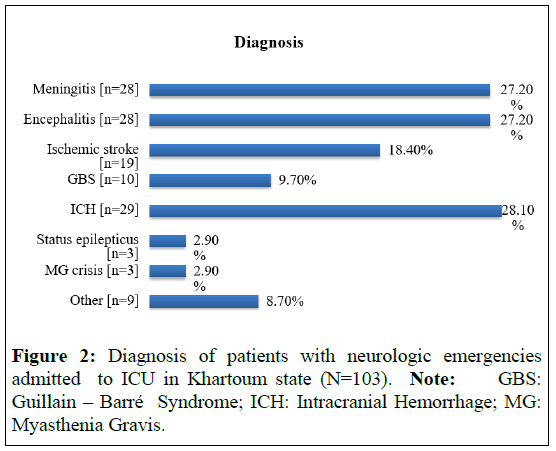
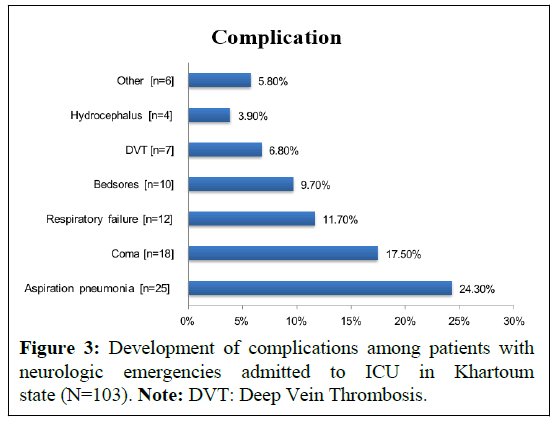
Results: Among 103 patients with neurologic emergencies admitted to ICU, 56% were Males (M) and 44% were Females (F). Patients are categorized into central nervous system diseases in which intracranial hemorrhage 28.1%, meningitis 27.2%, encephalitis 27.2%, ischemic stroke 18.4% were the common diagnoses. Whereas, in the peripheral nervous system Guillain-Barré Syndrome (GBS) 15.5%, Myasthenia Gravis (MG) crisis 3.88% were the common diseases. The common symptoms were altered mental status 64.1%, seizures 34%, motor weakness 27.2%, headache 18.4%, dysphagia 16.5%, fever 16.5%, shortness of breath 9.7% and mutism 7.8%. Hypertension 43.7% and diabetes mellitus 21.4% were the major co morbidities. Indications for ICU admission were mostly decreased level of consciousness 74.8%, accelerated hypertension 21.4%, respiratory failure 19.4%, aspiration pneumonia 10.7% and intractable seizures 2.9%. Majority of the patients 83.5% received antibiotics, 36% received Low Molecular Weight Heparin (LMWH), 32% received Proton Pump Inhibitors (PPI) and 10.6% received mechanical ventilation. 44% of patients improved and discharged, 41% developed complications mainly aspiration pneumonia 24.3% and 15% died.
Conclusion: Sudanese patients with neurologic emergencies admitted to ICU were older and mostly males. Intracranial hemorrhage and meningoencephalitis were the main diagnosis. Patients commonly presented with altered mental status. A decreased level of consciousness low Glasgow Coma Scale (GCS) was the foremost indication of ICU admission. Half of the patients were improved and aspiration pneumonia observed in a quarter of the patients.
Keywords: Proton pump inhibitors; Low molecular weight heparin; Intensive care unit; Neurological emergencies
Introduction
There are many neurological emergencies necessitate admission to the ICU, has different etiologies that can have a devastating results, with high rates of long-term disability and death. Early recognition of the disease, proper triage and management determine the prognosis [1]. Neurological emergencies account for between 2.6% and 14% of medical emergencies. Stroke represents a third of all neurological emergencies [2].
Furthermore, neurological emergencies are often severe conditions associated with high mortality and high costs, the latter not only generated by the emergency care provided in the acute phase, but also resulting from their frequent disabling outcomes. Thirty-day mortality is as high as 50% in cases of intraparenchymal hemorrhage, 50% in subarachnoid hemorrhage, 29% in cranial trauma and 20% in status epilepticus.
These conditions are frequent in the general population and the treatment provided within the first hours of the acute event may be crucial for patient survival and functional outcome. Other diseases (e.g. acute spinal cord injuries), though less frequent, are associated with similar high mortality, morbidity and costs [3].
There is a considerable rarity of data according to emergencies of neurology in intensive care among Sudanese patients. Therefore, we aimed in this study to evaluate etiologies, patterns of clinical presentation and outcomes of neurological emergencies patients admitted to ICU.
Materials and Methods
The prospective cross-sectional study conducted between October 2019 and April 2020 aimed to investigate neurologic emergencies among patients admitted to ICU departments in Khartoum state. A total of 103 patients were enrolled in the study and data collection utilized structured questionnaires covering various aspects such as demographics, clinical presentations, examinations, laboratory findings, reasons for ICU admission, specific neurological diagnoses, length of ICU stay, medication patterns and outcomes. Demographic information including age, gender and possibly other relevant factors were recorded to provide a comprehensive understanding of the patient population under study. Clinical presentations and examinations were documented to assess the severity and nature of neurological emergencies upon admission. Laboratory investigations, such as blood tests or imaging studies, were conducted to aid in diagnosis and treatment planning. The study also focused on indications for ICU admission, which could include factors like the need for close monitoring, respiratory support or interventions to manage neurological complications. Specific neurological conditions diagnosed during the ICU stay were identified and categorized.
Furthermore, the study explored the length of ICU stay for patients with neurological emergencies, providing insights into the duration of critical care required. Medication patterns were analyzed to understand the pharmacological interventions employed in managing neurologic emergencies in the ICU setting. Finally, outcomes such as mortality rates, neurological sequelae or improvements in clinical status were assessed to evaluate the effectiveness of ICU management strategies. Statistical analysis using SPSS v. 21.0 was conducted to derive meaningful insights from the collected data. Overall, this study contributes valuable information to the understanding and management of neurologic emergencies in ICU settings within the Khartoum state region.
Results
Among 103 patients with neurologic emergencies admitted to ICU, 56% were males, 44% were females and the mean age was 56.4 ± 16.8 years. Patients are categorized into central nervous system diseases in which intracranial hemorrhage 28.1%, Meningitis 27.2%, encephalitis 27.2%, ischemic stroke 18.4% were the common diagnoses. Whereas, in the peripheral nervous system GBS 15.5%, MG crisis 3.88% were the common diseases. The common symptoms were altered mental status 64.1%, seizures 34%, motor weakness 27.2%, headache 18.4%, dysphagia 16.5%, fever 16.5%, shortness of breath 9.7% and mutism 7.8%. Hypertension in 43.7% and diabetes mellitus 21.4% were the major co morbidities. Majority of the patients were hemodynamically stable. Indications for ICU admission were mostly decreased level of consciousness 74.8%, accelerated hypertension 21.4%, respiratory failure 19.4%, aspiration pneumonia 10.7% and seizures 2.9%.
Majority of the patients 83.5% received antibiotics, 36% received Low Molecular Weight Heparin (LMWH), 32% received Proton Pump Inhibitors (PPI) and 10.6% received mechanical ventilation. 44% of patients improved and discharged, 41% developed complications and 16 (15%) died, mainly due to aspiration pneumonia 24.3% (Figures 1-3).
Discussion
In the present study we aimed to describe etiologies, patterns of clinical presentation, risk and outcomes of neurological emergencies admitted to ICU among 103 patients in Khartoum state.
The patient demographic profile reflected that most of the ICU admitted were older (the mean age=56.4 ± 16.8 years) and male patients (M:F=1.3:1). These findings were similar to findings of Rajib, et al., [4] in Bangladesh who reported mean age of 45.11 ± 17.3 years and male patients (63.3%) predominated with a sex ratio was almost 2:1, Gajurel, et al., [5] in India who reported mean age of patients was 51.93 years and 55.4% were Males (M) (M:F=1.2:1) and Selemon, et al., [6] in Ethiopia who found mean age of the patients was 44.68 ± 1.1 years and males outnumbered females giving a sex ratio (M:F) of 1.22:1.
Intracranial hemorrhage 28.1%, meningitis 27.2%, encephalitis 27.2%, ischemic stroke (n=19; 18.4%) were the common diagnosis among our study patients. Our study was comparable to Ekanem, et al., [7] in Nigeria who found the most common diagnoses were stroke (52.5%) and meningoencephalitis (11.3%) and Rajib, et al., [4] in Bangladesh and Gajurel, et al., [5] in India reported stroke was the most common condition (47.5%) observed. In contrast, Selemon, et al., [6] in Ethiopia reported most common neurologic emergencies were cerebrovascular disorder (54%), neurologic complications of Human Immunodeficiency Virus infection/Acquired Immunodeficiency Syndrome (HIV/AIDS) (9%) and meningitis (8.7%).
Altered mental status was the predominant complain in 64.1% patients, in addition most of the patients 60.2% had moderate to severe reduced glasgow coma scaling. These observations were consistent with studies of Mapoure, et al., [8] and Sang-Beom, et al., [9] who reported altered mental status and decreased level of consciousness to be the major indication of ICU admission. However, Selemon, et al., [6] and Christopher, et al., [10] reported hemiparesis and focal weakness to be the main presenting complains, respectively.
Hypertension 43.7% and diabetes mellitus 21.4% were the major comorbidities among our study group. This because hypertension and diabetes are vascular risk factors for atherosclerosis and associated with cerebrovascular events. Similar findings were reported by Selemon, et al., [6] who reported hypertension (42.1%) was the frequent comorbidity among patients with neurologic emergencies.
A decreased level of consciousness low GCS was the major indication of ICU admission in 74.8% patients followed by high blood pressure in 21.4% and respiratory muscles weakness in 19.4% patients. This goes in same line with Roland, et al., [11] reported indications for transfer to ICU were mostly due to impaired consciousness and respiratory or cardiopulmonary complications.
The length of ICU stay ranged from 8-14 days in 38.8% of our study group. This range was similar to that reported by Selemon G, et al., [6] in Ethiopia (mean=18 ± 2 days). This is lower than the study conducted in northwest Nigeria where length of stay of neurologic disorders was 25 days [12].
The current study demonstrated antibiotics was the predominant medications received by 83.5% of the patients. This could be explained by high rate of neuro infections among our study patients. In addition, anticoagulants, antiplatelet and antihypertensive were taking by more than 20% of the patients. The study of Kuriakose, et al., [13] in India showed that antihypertensive drugs, antiplatelet, neuroprotective and nootropics were the main prescribed drug.
The morality rate was found in our patient to be 15%. Similar rates were reported Steffling, et al., [14] (15.4%) and lower than (28.5%) (56%), Selemon, et al., [6] (27.3%). In addition, 41% patients developed complications, mainly aspiration pneumonia (24.3%), prolonged coma state (17.7%) and respiratory failure (11.7%) of the patients.
Conclusion
Sudanese patients with neurologic emergencies admitted to ICU were older and mostly males. Intracranial hemorrhage, meningitis, encephalitis, stroke and neuromuscular failure were the main diagnosis. Patients commonly presented with altered mental status. Hypertension and diabetes mellitus were the major comorbidities. A decreased level of consciousness was the foremost indication of ICU admission. Half of the patients improved. Aspiration pneumonia occurred in the quarter of our patients. In the study, Sudanese patients admitted to the ICU for neurologic emergencies were predominantly older males. Primary diagnoses included intracranial hemorrhage, meningitis, encephalitis, stroke and neuromuscular failure. Altered mental status was a common presentation, with hypertension and diabetes mellitus as prevalent comorbidities. Decreased consciousness was the primary indication for ICU admission and half of the patients showed improvement. Aspiration pneumonia affected a quarter of the patients, highlighting a significant complication. This data underscores the critical nature of neurologic emergencies and the associated challenges in ICU management.
Ethical consideration
An ethical approval was obtained from Sudan Medical Specialization Board (SMSB). Approval acceptance to the hospital authority was being given. Written and verbal consents were obtained from patients or their families. Data used anonymously by using identity numbers instead of names is order to protect patient’s identity and kept securely and in separate file. No reference to any individual participant made in study reports. Subject identities were being known only by the study staff.
References
- Kottapally M, Josephson SA (2016) Common neurologic emergencies for nonneurologists: When minutes count. Cleve Clin J Med 83:116-126.
[Crossref] [Google Scholar] [PubMed]
- Ibáñez AG, Irimia P, Martínez-Vila E (2008) Urgencias neurológicas y guardias de Neurología The problem of neurological emergencies and the need for specific neurology shifts. An Sist Sanit Navar 31:7-13.
[Google Scholar] [PubMed]
- Stone K (2009) When seconds count: tackling neurological emergencies. Lancet Neurol 8:702-703.
- Chowdhury RN, Hasan AH, Rahman YU, Khan SI, Hussain AR, et al. (2014) Pattern of neurological disease seen among patients admitted in tertiary care hospital. BMC Res Notes 7:1-5.
[Crossref] [Google Scholar] [PubMed]
- Gajurel BP, Parajuli P, Nepali R, Oli KK (2012) Spectrum of neurological disorders admitted in Tribhuvan University Teaching Hospital Maharajgunj. JIOMN 34:50-53.
- Gebrezgabiher S, Azazh A, Kebede S (2019) Pattern of Neurologic Emergencies in Tikur Anbessa Specialized Hospital-Emergency Department in Addis Ababa, Ethiopia. J Neurol Disord 7:408.
- Philip-Ephraim EE, Eyong KI, Oparah SK, Williams UE, Udonwa N (2013) Profile of Neurologic Emergencies At The Accident & Emergency Department of A Tertiary Hospital in South Nigeria. J Neurol Sci 30:34.
- Mapoure YN, Ongono JS, Nkouonlack C, Beyiha G, Mouelle AS, et al. (2015) Neurological disorders in the emergency centre of the Douala General Hospital, Cameroon: A cross-sectional study. AfJEM 5:165-170.
- Jeon SB, Lee HB, Koo YS, Lee H, Lee JH, et al. (2021) Neurological emergencies in patients hospitalized with nonneurological illness. J Patient Saf 17:e1332–e1340.
[Crossref] [Google Scholar] [PubMed]
- Hansen CK, Fisher J, Joyce NR, Edlow JA (2015) A prospective evaluation of indications for neurological consultation in the emergency department. Int J Emerg Med 8:1-6.
[Crossref] [Google Scholar] [PubMed]
- Backhaus R, Aigner F, Schlachetzki F, Steffling D, Jakob W, et al. (2015) Inventory of a neurological intensive care unit: who is treated and how long? Neurol Res Int 2015:696038.
[Crossref] [Google Scholar] [PubMed]
- Owolabi LF, Shehu MY, Shehu MN, Fadare J (2010) Pattern of neurological admissions in the tropics: Experience at Kano, Northwestern Nigeria. Ann Indian Acad Neurol 13:167.
[Crossref] [Google Scholar] [PubMed]
- Wagle L, Thomas AA, Shrestha S (2017) Drug utilisation study of stroke and other patients admitted to general ward of neurology unit at quaternary care private hospital. Int J Curr Pharm Res 9:23-28.
- Steffling D, Ritzka M, Jakob W, Steinbrecher A, Schwab-Malek S, et al. (2023) Indications and outcome of ventilated patients treated in a neurological intensive care unit. Nervenarzt 83:741-750.
[Crossref] [Google Scholar] [PubMed]
Citation: Daoud MH, Abuobieda H, Abdelhalim SI, Mohmed MHA, Elamin AEA (2024) The Pattern of Neurological Emergencies: Frequency, Etiology and Outcome, for Patients Admitted to Intensive Care Unit at Khartoum State Hospitals. J Alzheimers Dis Parkinsonism 14:590. DOI: 10.4172/2161-0460.1000590
Copyright: © 2024 Daoud MH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 819
- [From(publication date): 0-2024 - Feb 08, 2025]
- Breakdown by view type
- HTML page views: 743
- PDF downloads: 76