Research Article Open Access
The Palliative Curative Treatment of Untreatable Metastatic Solid Tumor Patients by a Psycho-Neuroendocrino-Immunophytotherapic (PNEIF) Regimen with Natural Anticancer Agents
Paolo Lissoni1, Giusy Messina1*, Fernando Brivio1, Franco Rovelli1, Luca Fumagalli2 and Giuseppe Di Fede3
1International Institute of Psychoneuroendocrinoimmunology, Milan, Italy
2Manzoni Hospital, Surgery Department, Lecco, Italy
3Institute of Biological Medicine, Milan, Italy
- *Corresponding Author:
- Giusy Messina
International Institute of Psychoneuroendocrinoimmunology, Milan, Italy
Tel: +39026693950
Fax: +39026700708
E-mail: giusy.messina@libero.it
Received date: February 23, 2017; Accepted date: March 21, 2017; Published date: March 25, 2017
Citation: Lissoni P, Messina G, Brivio F, Rovelli F, Fumagalli L, et al. (2017) The Palliative Curative Treatment of Untreatable Metastatic Solid Tumor Patients by a Psycho-Neuroendocrino-Immunophytotherapic (PNEIF) Regimen with Natural Anticancer Agents. J Palliat Care Med 7:299. doi:10.4172/2165-7386.1000299
Copyright: © 2016 Paolo, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Several natural agents, including both human endogenous neuroendocrine substances, namely the pineal hormones, and plants, mainly Aloe, Myrrh and Magnolia, have been proven to exert anticancer activities, due to antiproliferative and immunomodulating properties. On this basis, a study was planned in an attempt to evaluate the therapeutic efficacy of a psychoneuroendocrinoimmun-phytotherapic (PNEIF) regimen with pineal hormones and antitumor plants in a group of untreatable metastatic solid tumor patients, for whom no treatment other than the palliative therapy was available, because of lack of response to previous chemotherapies, poor clinical status or personal refusal of chemotherapy, and with a life expectancy less than 1 year. The pineal hormone melatonin (MLT) and 5-methoxytryptamine (5-MTT) were given orally at 100 mg/day in the dark period and at 5 mg in the light period of the day, respectively, in association with Aloe and Myrrh mixture at 10 ml thrice/day, Magnolia cortex at 500 mg twice/day and Bowellia at 1000 mg/day in patients with brain metastases. A complete response (CR) and partial response (PR) were achieved in 2 and in 8 patients. Then, an objective tumor regression was obtained in 10/132 (8%) patients. A stable disease (SD) was found in 61 patients, then a disease control (DC), consisting of CR plus PR plus SD, was achieved in 71/132 (54%) patients, whereas the remaining patients had a progressive disease (PD). A survival longer than 1 year was seen in 63/132 (48%) patients, and the percent of 2 and 3-year survival obtained in patients with response or SD was significantly longer than that found in patients with PD. The treatment was well tolerated and no relevant biological toxicity occurred. This preliminary study would demonstrate that a PNEIF combination with natural anticancer agents may prolong the survival time in patients, for whom no standard therapy was available other than the only palliative therapy, and with an expected survival less than 1 year.
Keywords
Anticancer plants; Natural anticancer agents; Pineal hormones
Introduction
Today, there is no doubt about the fundamental importance of the immune system in the control of cancer growth and that the anticancer immunity is namely a lymphocyte-dependent phenomenon [1,2], as demonstrated by the fact that the evidence of lymphocytopenia is one of the most negative prognostic factor in cancer patients [1-3]. With respect to the physiology of the antitumor immune response, the anticancer potency of the immune system could be further enhanced and amplified at least from a theoretical point of view through two different strategies, consisting of an artificial manipulation of the immune system, or of a modulation of its function by acting at psychoneuroendocrine levels on the basis of the existence of a physiological psychoneuroendocrine regulation of the immune reactions [4-6]. The first strategy is founded on the possibility to artificially generate molecules, such as the monoclonal antibodies (MAB) [7,8], capable of acting on the key-points of the anticancer immunity, such as cell surface receptors involved in the inhibitory regulation of T lymphocyte-mediated anticancer immunity, including cytotoxic T lymphocyte antigen-4 (CTLA-4) or programmed death-1 (PD-1) [7,8] by blocking their activation. On the contrary, the other strategy has been elaborated an attempt to reproduce in cancer patients the immune functionless of the status of health, which is characterized by a natural immunobiological resistance against cancer onset and dissemination, by simply correcting the main endocrine and immune alterations occurring during cancer progression, the most evident of them is a progressive decline in the neuroendocrine function of the pineal gland [9,10], whose anticancer activity has been well documented in both experimental [11] and clinical [12] conditions. Moreover, in the recent years a great effort was spent also to identify possible natural non-toxic anticancer molecules, either in the nature of plants, or in the human body. As far as the human body is concerned, the pineal gland would represent the main anticancer organ [13], since it produces at least two anticancer neuroendocrine molecules, consisting of the indole hormones melatonin (MLT) [14] and 5-methoxytryptamine (5-MTT) [15], which are mainly released by the pineal gland during the dark and the light period of the day, respectively. Most studies carried out up to now have been limited to the investigation of the antitumor mechanisms of MLT [14], which is considered the main pineal hormone, but preliminary experimental studies would suggest that 5-MTT may exert an anticancer antiproliferative activity superior to that of MLT itself [15]. The anticancer activity of MLT is due to several mechanisms, and at present it represents the only molecule existing in the world capable of counteracting the overall main phases responsible for cancer progression, including the loss of the apoptotic process and the persistent activation of cell surface receptors for tumor growth factors, such as epidermal growth factor (EGF), the alteration of intercellular junctions and the consequent change in the intercellular matrix and the stimulation of the angiogenesis, and cancer-related mechanisms responsible for the immunosuppressive status, which characterizes the advanced neoplastic disease. At the other side, several plants may produce anticancer substances, the most investigated of them are Aloe [16], Myrrh [17], Cannabis Indica [18] and Magnolia [19]. According to the results available upto now, the main anticancer cytotoxic molecules would be represented by aloehemodine for both Aloe Vera and Arborescens [16], guggulsterone for Myrrh [17], tetrahydrocannabinol (THC) for Cannabis [18] and honokiol for Magnolia [19]. On these bases, a study was performed in an attempt to evaluate the therapeutic efficacy of a biological natural antitumor psychoneuro- endocrino-immuno-phytotherapic (PNEIF) regimen, with pineal indole hormones and some well investigated anticancer molecules drawn from plants, in metastatic cancer patients, for whom no other standard anticancer therapy was available or accepted by patients.
Materials and Methods
Patients
The study included 132 metastatic solid tumor patients, who were considered as untreatable cancer patients according to the conventional antitumor protocols.
Eligibility criteria were, as follows: histologically proven metastatic solid tumors other than breast cancer and prostate cancer, measurable lesions, no double tumor, and no availability of further conventional chemotherapeutic or target anticancer therapies because of lack of response to previous standard antitumor treatments, or poor clinical status with a consequent inability to tolerate the conventional treatments, and life expectancy lower than 1 year. Two female patients, affected by liver metastases due to colon cancer and by endometrial adenocarcinoma with lung metastases, respectively, were also included in the study because of their personal refusal of chemotherapy, with a consequent lack of other potentially effective therapies. Metastatic breast and prostate cancer patients were not included in the study because of the availability of several potential non-toxic treatments, including the endocrine therapies and the chemotherapeutic metronomic regimens. The experimental protocol was explained to each patient, and informed consent was obtained. The clinical characteristics of cancer patients are reported in Table 1.
| Eligibility Criteria | |
|---|---|
| Histologically proven solid tumor (other than breast and prostate carcinomas) | |
| Measurable lesions | |
| No availability of other oncological standard therapies because of lack of response to previous chemotherapies, poor clinical status or personal refusal of standard therapies | |
| Life expectancy less than 1 year | |
| Clinical Characteristics Of Patients | |
| N | 132 |
| M / F | 67/65 |
| Median age | 65 ( 39-62 ) |
| Tumor Hystotipes | |
| Lung cancer | 34 |
| -Non small cell | 28 |
| -Small cell | 6 |
| Colorectal cancer | 19 |
| Pancreati carcinoma | 20 |
| Gastric cancer | 9 |
| Biliary tract carcinoma | 11 |
| HCC | 6 |
| Bladder cancer | 3 |
| Ovarian carcinoma | 14 |
| Melanoma | 5 |
| Sarcoma | 11 |
| Dominant Metastasis Sites | |
| Soft tissues | 19 |
| Bone | 5 |
| Lung | 36 |
| Liver | 24 |
| Liver plus lung | 19 |
| Peritoneum | 16 |
| Brain | 13 |
| Previous chemotherapies | 104 |
| No previous chemotherapies | 28 |
| - poor clinical status or age | 25 |
| - personal refusal | 3 |
Table 1: Eligibility criteria and clinical characteristics of untreatable metastatic solid tumor patients treated by psychoneuroendocrinoimmunotherapy of cancer.
Methods
The PNEIF regimen consisted of an oral administration of MLT at a dose of 100 mg once day in the dark period of the photoperiod, 5- MTT at 5 mg/day in the period of maximum light, Aloe arborescens plus Myrrh mixture (60/40%) at 10 ml thrice/day and Magnolia cortex with honokiol content greater than 50% at 500 mg twice/day. In patients with brain metastases, Boswellia was also orally administered at 1000 mg/day because of its anti-oedema activity. The treatment was continued without interruption until disease progression.
The clinical response was evaluated according to WHO criteria, by repeating the radiological examinations, including CT scan and PET, every 3 months. Patients were also assisted by a spiritual psychotherapeutic approach, consisting of progressively rediscovering the pleasure as a spiritual experience. Data were statistically evaluated by the chi-square test and the Student’s t test.
Results
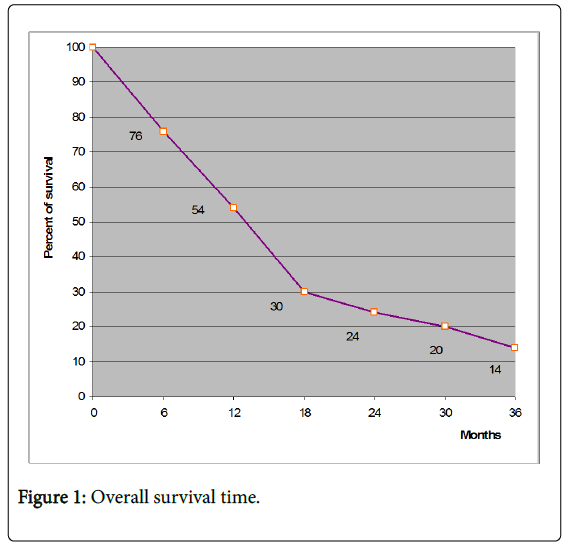
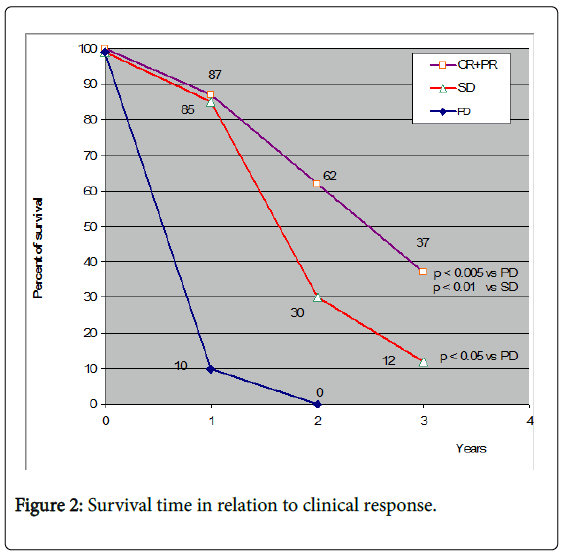
The clinical response achieved in cancer patients are reported in Table 2. A complete response (CR) was achieved in one patient with peritoneal metastases due to gastric cancer and in another patient with lung adenocarcinoma. Moreover, a partial response (PR) was obtained in 8 other patients (Colorectal cancer 2; Pancreatic cancer 1; Biliary tract carcinoma 1; Hepatocarcinoma 1; Malignant melanoma 2; Endometrial cancer 1). Therefore, an objective tumor regression (CR +PR) was found in 10/132 (8%) patients, with a median duration of 18 months (range 4-38). In particular, both patients who had refused chemotherapy for personal reasons, the former with lung metastases due to gynaecologic cancer and the latter with liver metastases due to colon cancer, obtained a PR. A stable disease (SD) was achieved in other 61/132 (46%) patients. Therefore, a disease control (DC), including CR, PR and SD, was achieved in 71/132 (54%) patients, whereas the remaining 61 patients had a progressive disease (PD). Moreover, with respect to a life expectancy less than 1 year, a survival time longer than 1 year was observed in 63/132 (48%) patients, as illustrated in Figure 1. Moreover, 28 (21%) patients were still alive at 2 years. Finally, a survival longer than 3 years was achieved in 16/132 (13%). Figure 2 illustrates the 3-year survival time observed in cancer patients in relation to their clinical response to treatment. The percentage of 3-year survival time observed in patients, who obtained an objective tumor regression (CR+PR) was statistically significant with respect to both patients with PD (P<0.005) or SD (P<0.05). Moreover, patients who had SD also obtained a significantly longer survival at 3 years than that found in patients with PD (P<0.05). In more detail, no patient with PD was alive at 2 years. On the contrary, 26/71 (36%) patients and 11/71 (15%) of patients with clinical response or SD were still alive at 2 and at 3 years, respectively.
| Clinical Response * | Survival ( Years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tumors | n | CR | PR | CR+PR | SD | DC | PD | 1 | 2 | 3 |
| ALL | 132 | 2 | 8 | 10 (8%) | 61 | 71 | 61 | 63 (48 %) | 28 (21%) | 16 (13%) |
| Lung | 34 | 1 | 0 | 1 | 17 | 18 | 16 | 16 (47%) | 7 (21%) | 6 (18%) |
| Colon | 19 | 0 | 2 | 2 | 10 | 12 | 7 | 10 (53%) | 7 (37%) | 4 (21%) |
| Pancreas | 20 | 0 | 1 | 1 | 8 | 9 | 11 | 9 (45%) | 1 (11%) | 0 |
| Biliary | 11 | 0 | 1 | 1 | 4 | 5 | 6 | 5 (45%) | 3 (27%) | 2 (18%) |
| Stomach | 9 | 1 | 0 | 1 | 3 | 4 | 5 | 2 (22%) | 1 (11%) | 1 (11%) |
| HCC | 6 | 0 | 1 | 1 | 3 | 4 | 2 | 3 (50%) | 2 (33%) | 1 (17%) |
| Bladder | 3 | 0 | 0 | 2 | 2 | 2 | 1 | 2 (67%) | 0 | 0 |
| Ovarian | 14 | 0 | 1 | 1 | 8 | 9 | 5 | 9 (64%) | 3 (21%) | 1 (7%) |
| Melanoma | 5 | 0 | 2 | 2 | 1 | 3 | 2 | 2 (40%) | 1 (20%) | 1 (20%) |
| Sarcoma | 11 | 0 | 0 | 0 | 5 | 5 | 6 | 5 (45%) | 3 (27%) | 1 (9%) |
*CR: Complete Response; PR: Partial Response; SD: Stable Disease; DC: Disease Control; PD: Progressive Disease
Table 2: Clinical response (WHO) and survival in untreatable metastatic cancer patients under psychoneuroendocrinoimmunotherapy (PNEIF) of cancer.
No treatment-related toxicity occurred. A mild excitation state was observed in 12/132 (9%) patients during the first days of high-dose MLT administration, which was corrected through the simple reduction of its dose for few days, followed by a progressive increase until the planned dosage of 100 mg/day. No cachexia occurred under the PNEIF therapy, neither in those patients who had a disease progression. On the contrary, most patients experienced an improvement in their mood, in the quality of sleep with lore episodes of dreaming, and a mild relief of asthenia.
Discussion
The results of this preliminary study, which was carried out in a group of metastatic solid tumors patients for whom no other standard anticancer therapies, including chemotherapy and target therapies, was not available because of progression on previous treatments, or who were unable to tolerate the conventional therapies because of poor clinical status or personal refusal, and then with life expectancy less than 1 year, would demonstrated that a PNEIF regimen consisting of the association between a neuroendocrine therapy with the antitumor pineal hormones and the products of the most experimentally an clinically investigated natural antitumor plants, including Aloe , Myrrh and Magnolia , may induce an objective control of disease, with possible tumor regressions and disease stabilization and a prolongation of the survival time with respect to the expected one. MLT alone is generally unable to induce objective tumor regressions in a considerable number of cases [10,12,20], and the percentage of 1-year survival in the same types of cancer patients treated by MLT alone has appeared to be generally less than 30%. Therefore, this study would suggest that the antitumor effect of MLT may be amplified by the association with the most potentially effective antitumor plants. Moreover, PNEIF-induced objective tumour regressions or disease stabilizations would not represent a simple epiphenomenon, because of their association with a longer survival time with respect to that observed in patients who progressed under PNEIF therapy. If further studies will confirm these results, PNEIF regimen could be interpreted as a link between palliative and curative therapies of human neoplasms, and propose as a potential effective antitumor treatment for cancer patients, for whom no other possibility of cure may be available.
However, more recent studies have shown that the pineal gland may release not only anticancer indole hormones, but another group of molecules also provided by anticancer activity in association with some effects of consciousness expansion [21], the so-called betacarbolines, which could further enhance the efficacy of a PNEIF regimen for the untreatable cancer patients.
References
- Riesko A (1970) Five-year cancer cure: relation to total amount of peripheral lymphocytes and neutrophils. Cancer 25: 135-140.
- Grimm EA, Mazumder A, Zhang HZ, Rosenberg SA (1982) Lymphokine-activated killer cell phenomenon. J Exp Med 155: 1823-1841.
- Fumagalli L, Lissoni P, Di Felice G, Meregalli S, Valsuani G, et al. (1999) Pretreatment serum markers and lymphocyte response to interleukin-2 therapy. Br J Cancer 80: 407-411.
- Maestroni JGM (1993) The immunoneuroendocrine role of melatonin. J Pineal Res 14: 1-10.
- Jankovic B (1994) Neuroimmunomodulation from phenomenology to molecular evidence. Ann NY Acad Sci 741: 3-38.
- Riley V (1981) Psychoneuroendocrine influences on immunocompetence and neoplasia. Science 212: 1100-1109.
- Okazaki T, Honjo T (2007) PD-1 and PD-1 ligands: from discovery to clinical application. Int Immunol 19: 813-824.
- Deeks ED (2014) Nivolumab: a review of its use in patients with malignant melanoma. Drugs 74: 1233-1239.
- Conti A, Maestroni GJM (1995) The clinical neuroimmunotherapeutic role of melatonin in Oncology. J Pineal Res 19: 103-110.
- Brzezinski A (1997) Melatonin in humans. N Engl J Med 336: 186-195.
- Bartsch H, Bartsch C (1981) Effect of melatonin on experimental tumors under different photoperiods and times of administration. J Neural Transm 52: 269-279.
- Mills E, Wu P, Seely D, Guyatt G (2005) Melatonin in the treatment of cancer: a systematic review of randomized controlled trials and meta-analysis. J Pineal Res 39: 360-366.
- Lissoni P (1999) The pineal gland as a central modulator of cytokine network. Neuroendocrinol Lett 20: 343-349.
- Vijayalaxmi B, Thomas CR, Russel RJ, Herman TS (2002) Melatonin: from basic research to cancer treatment clinics. J Clin Oncol 20: 2575-2601.
- Sze SF, Ng TB, Liu WK (1993) Antiproliferative effect of pineal indoles on cultured tumor cell lines. J Pineal Res 14: 27-33.
- Guo JM, Xiao BX, Liu Q, Zhang S, Liu DH, et al. (2007) Anticancer effect of aloe-emodin on cervical cancer cells involves G2/M arrest and induction of differentiation. Acta Pharmacol Sin 28: 1991-1995.
- Hanus LO, Rezanka T, Dembitsky VM, Moussaieff A (2005) Myrrh-Commiphora chemistry. Biomed Papers 149: 3-28.
- Grotenhermen F (2004) Pharmacology of cannabinoids. Neuroendocrinol Lett 25: 14-23.
- Levi EF, Arbiser JL (2009) Honokiol, a multifunctional antiangiogenic and antitumor agent. Antioxid Redox Signal 11: 1139-1148.
- Lissoni P (2002) Is there a role for melatonin in supportive care? Supp Care Cancer 10: 110-116.
- Di Fede G, Messina G, Monzon A, Meli O, Gavazzeni C, et al. (2017) Clinical Effects of the Pineal Antitumor and Psychedelic Beta-Carboline Pinealine in the Palliative Therapy of Untreatable Metastatic Cancer Patients. Integrative Cancer Biology & Research 1: 002.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 2644
- [From(publication date):
March-2017 - Nov 24, 2024] - Breakdown by view type
- HTML page views : 1998
- PDF downloads : 646