Research Article Open Access
The Occurrence of Positive Psychotic Experiences in an Outpatient Clinic in Flanders
Krystle Gaul1*, E De Loore1 and D van West1,2,31University Centre of Child and Adolescent Psychiatry Antwerp (UKJA), Hospital Network Antwerp (ZNA), Lindendreef 1, 2020 Antwerp, Belgium
2Faculty of Medicine and Health Sciences, Collaborative Antwerp Psychiatric Research Institute (CAPRI), University of Antwerp, Universiteitsplein 1, 2610 Antwerp, Belgium
3Faculty of Psychology and Educational Sciences, Lifespan and Clinical Psychology (KLEP), Free University of Brussels, Pleinlaan 1, 1050 Brussels, Belgium
- *Corresponding Author:
- Krystle Gaul
University Centre of Child and Adolescent Psychiatry Antwerp (UKJA)
Hospital Network Antwerp (ZNA)
Lindendreef 1, 2020 Antwerp, Belgium
Tel: +32 479/454510
E-mail: Gaul.Krystle@gmail.com
Received Date: Mar 02, 2017; Accepted Date: Mar 27, 2017; Published Date: Apr 03, 2017
Citation: Gaul K, De Loore E, van West D (2017) The Occurrence of Positive Psychotic Experiences in an Outpatient Clinic in Flanders. J Child Adolesc Behav 5: 338. doi:10.4172/2375-4494.1000338
Copyright: © 2017 Gaul K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Objective: Psychotic like experiences (PLEs) resemble psychotic symptoms but are more benign and transient. They occur numerously in clinical and non-clinical samples and have a peak incidence in adolescence. PLEs can be linked to psychopathology and, in the presence of risk factors, PLEs can make a transition to psychotic symptoms and psychosis. The aim of this study was to measure the occurrence of PLEs in a Flemish clinical sample of adolescents using the CAPE (Community Assessment of Psychic Experiences). Gender, age, IQ differences and possible links with psychopathology, distress and impairment have been investigated. Method: 1176 adolescents between 12 and 17 years old were referred to a child and adolescent psychiatric outpatient clinic for psychiatric assessment. PLEs were measured using the CAPE, more precisely the CAPE positive experiences scale (CAPE-P, 20 questions). PLEs were divided into 5 subdimensions: Hallucination, Paranoia, Delusion, Grandiosity and Paranormal Belief. Results: 734 CAPEs were valid for research. 94.2% of adolescents in the clinical sample reported at least one PLE at least ‘sometimes’. 62.3% of our population reported at least one PLE at least ‘often’, which was a higher rate than found in the general population. 83.2% of the population reported at least ‘a bit distress’ for at least one PLE, whereas 51% reported to be ‘quite or very distressed’ about at least one PLE. Girls reported more PLEs than boys and reported higher levels of distress. There was no significant general trend in PLEs found when looked at age or IQ distribution. PLEs with distress could be linked to psychopathology in general, but not to specific diagnoses. Conclusion: In comparison to the general population, adolescents in a clinical population experience PLEs more often and with a higher degree of distress. The CAPE can be used in a clinical population for follow up and identification in the risk of transition. Higher risk can be defined by a higher score of frequency and distress on the CAPE and the persistence of this score over time. Risk of transition increases with a certain degree of impairment (that might be caused by comorbid psychopathology) and the combination with specific risk factors for psychosis.
Keywords
Positive psychotic experiences; Occurrence; CAPE; Clinical population; Gender difference; Psychopathology; Age difference
Introduction
Psychotic like experiences (PLEs), such as hallucinatory experiences or delusional thoughts, are often reported by children and adolescents both in clinical [1,2] and non-clinical [1,3] populations. PLEs have a peak incidence in adolescence due to hormonal changes, ongoing maturation and myelination processes and higher dopaminergic transmission at the onset of puberty [4]. On the level of social cognitive processes, the increased self-focus and feeling of invincibility leads to a process referred to as ‘adolescent egocentrism’, which can be responsible for misinterpretations of the social world and the beliefs of others [4,5].
PLEs are more commonly reported by girls than boys and decline with increasing age [6,7]. Individuals can express more or less PLEs depending on their genetic liability for psychosis [8]. Although PLEs are mostly benign and transient [7,9], they may lead to distress and need for care, thus increasing the risk of psychopathology.
Although most individuals with PLEs will never develop e psychotic disorder, PLEs, in combination with risk factors for psychosis (IQ, use of cannabis, urbanicity, and so on), may persist over time increasing the risk of a later psychotic disorder [7,10,11].
This gives rise to the hypothesis that not the occurrence of, but rather the distress associated with PLEs, the degree of impairment and need for care may be an important focus for early intervention and treatment. It is also hypothesized that PLEs are not linked to specific psychiatric disorders, but that a higher amount of PLEs may increase the risk of psychopathology in general [12]. The current paper aims to investigate the occurrence of PLEs in a Flemish clinical sample of adolescents by using the CAPE (Community Assessment of Psychic Experiences) [13]. It aims to investigate the association between PLEs on the one hand and distress, impairment, psychopathology and need for care on the other hand. The distribution of PLEs according to age, gender and IQ are also examined, based on the relation described in literature for these three risk factors.
Method
Participants
Data were retrospectively derived from 1176 adolescents (12-17 years) in the outpatient clinic of the University Centre of Child and Adolescent Psychiatry in Antwerp (UKJA) from 2009 through 2015. Some patients were seen twice for psychiatric assessment during this period. If so, CAPEs were only included twice if the period between assessments was more than one year.
PLEs were assessed by using the CAPE. The CAPE is a self-report questionnaire that focuses on the frequency and distress of PLEs. The extended version consists of 42 self-report items [13], whereas the CAPE positive experiences scale (CAPE-P) exists of 20 self-report items, used previously in both clinical and non-clinical adolescent populations [1,3]. The CAPE-P showed good internal consistency (Cronbach alpha=0.94) [1]. Both frequency and distress associated with the experience were assessed on a 4-point scale (0=never/not distressed; 1=sometimes/a bit distressed; 2=often/quiet distressed to 3=nearly always/very distressed). Scores were calculated for 5 subdimensions (Hallucination, Paranoia, Grandiosity, Delusion and Paranormal Belief) within the positive psychotic dimension [1]. The presence of psychopathology was examined by clinical psychiatric observation, assessment and use of the Development and Well-Being Assessment (DAWBA), a semi-structured screening instrument [14]. IQ was mainly measured by means of Wechsler scale WISC-III [15]. Severity of impairment was measured by using the Children’s Global Assessment Scale (CGAS) [16]. Intensity of care was examined by employing the Dutch translation of the Child and Adolescent Service Intensity Instrument (CASII) [17].
Statistical analyses
For the statistical analyses, SPPS 22.0 was used [18].
Raw “CAPE frequency/distress” scores were calculated in total and for each subdimension.
“CAPE frequency/distress” scores were also dichotomized (value 1 indicating at least “sometimes” or “a bit distress”) and calculated in total and for each subdimension.
Mean frequency and distress scores were calculated in total and for each subdimension. Because of the known high prevalence of PLEs, the 90th percentile was calculated to define a clinically important group with a higher risk.
A linear regression analysis was conducted to examine the association between the frequency of PLEs and the degree of distress caused by these PLEs, with raw “CAPE distress score” as dependent variable and raw “CAPE frequency score” as independent variable.
In order to assess the association between PLEs on the one hand and age and IQ on the other hand, a linear regression analysis was carried out, with dichotomized “CAPE frequency/distress score” (total and for each subdimension) as dependent variable and “age” and “IQ” respectively as independent variables.
In order to investigate the association between PLEs on the one hand and gender, psychopathology, impairment, and need for care on the other hand, AN(C)OVA was used to measure the significance with dichotomized “CAPE frequency/distress score” (total and for each subdimension) as dependent variable and “gender”, “psychopathology”, “CGAS” and “CASII” respectively as independent variables.
Age, gender and IQ were controlled for in all analyses. Comorbidity was accounted for by controlling for other diagnoses when the association with psychopathology was investigated.
Results
Descriptive statistics
The Response rate at valid CAPE registration was 62%. 443 CAPEs did not return (mean age 14.5 years old; SD 1.6; 27.1% girls). The study population (N=734, one person filled in two CAPEs with an interval of 2 years and 3 months) showed a mean age of 14.0 years old (SD 1.5), consisted of 30.1% girls and had a mean intelligence score of 93.0 (SD 19.0). In total 9.8% of the clinical sample had no psychiatric diagnosis, 10.9% had a deferred diagnosis and 2% of the diagnoses were missing. 77.3% of the clinical sample had a DSM (Diagnostic and Statistical Manual of Mental Disorders) IV-TR or 5 diagnosis: 40.7% ADHD, 14.0% Autism Spectrum Disorder (ASS), 13.9% Mood Disorder, 9.4% Anxiety Disorder, 1.5% Tic Disorder, 13.8% Behavioural Disorder, 13.5% Learning Disorder/Motor Disorder/Language Disorder, 0.4% Eating Disorder, 0.7% Attachment Disorder, 1.0% Substance Abuse, 1.0% Psychotic Disorder and 1.2% Other diagnoses.
The population was divided into categories for the CGAS depending on definition of impairment, with as first category scores from 0 to 40 “major impairment of functioning (2.2% of population)”; second category scores from 41 to 60 “moderate impairment of functioning (42.9% of population)” and third category scores from 61 to 100 “slight or no impairment of functioning (41.6% of population)”. Data were missing for 13.3% of the total population.
The population was divided into categories for the CASII depending on the need for care. A first category included CASII levels 0 and 1, “no further need for care” (8.0% of population), a second category included levels 2 to 6, “further need for care” (46.5% of population). Data was missing for 45.5% of the total population.
Prevalence of positive psychotic experiences and associated distress
A mean CAPE frequency score of 6.93 was found (interquartile range (IQR)=3-10). 90th percentile was 14 experiences. 94.2% of the adolescents reported at least one PLE at least ‘sometimes’. 62.3% reported at least one PLE ‘often or nearly always’. A mean CAPE distress score of 4.56 out of 20 experiences was found. 83.2% of the population reported at least ‘a bit distress’ for at least one PLE, 51% reported to be ‘quite or very distressed’ about at least one PLE. 90th percentile for distress was 10 out of 20 experiences.
Distress
Linear regression showed that there is a significant linear relation between CAPE frequency score and CAPE distress score. It showed a stronger linear relation with hallucinations, paranoia and delusions than with grandiosity and paranormal belief (Table 1).
| CAPE score | Regression coefficient β |
|---|---|
| Total | 0.876** |
| Hallucination | 0.858** |
| Paranoia | 0.863** |
| Delusion | 0.844** |
| Grandiosity | 0.530** |
| Paranormal Belief | 0.495** |
Table 1: Linear regression analysis for CAPE frequency and CAPE distress score (**p<0.001).
Gender, age and IQ differences
The mean CAPE frequency score was significantly higher for girls regarding the total score and all the subdimensions, with the exception of Grandiosity. The results remained significant after controlling for Mood Disorders (Table 2). Girls reported significantly more distress than boys (p<0.001). Girls reported for a mean of 6.17 PLEs to experience at least ‘a bit distress’. Boys reported to experience at least ‘a bit distress’ for a mean of 3.95 PLEs.
| Gender | Mean CAPE frequency | Hallucinations | Paranoia | Grandiosity | Delusions | Paranormal Belief |
|---|---|---|---|---|---|---|
| Boys | 6,39** (SD4,48) |
0,57* (SD 0,92) |
2,72** (SD 1,56) |
0,81 (SD 0,80) |
1,85** (SD 1,93) |
0,48** (SD 0,70) |
| Girls | 8,38** (SD 4,58) |
0,80* (SD 1,00) |
3,59** (SD 1,46) |
0,78 (SD 0,75) |
2,53** (SD 2,20) |
0,80** (SD 0,82) |
Table 2: Mean CAPE frequency score for gender. (**p<0.001, SD: Standard Deviation).
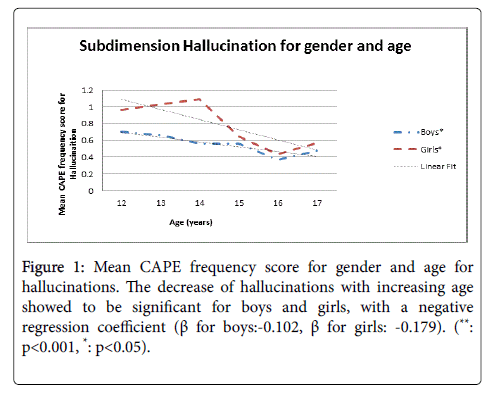
Concerning the age distribution, no linear relation was found for the general mean CAPE frequency score or for most of the subdimensions. Only regarding hallucinations, a significant and inverse linear relation was found (Figure 1). No significant difference was found for mean CAPE distress scores according to age.
When looking at IQ distribution there were no significant differences or linear trends found in the mean CAPE frequency score. For hallucinations, a borderline significant result was found with an inverse linear relation (p=0.052, β=-0.103). Based on distress, there was a borderline significant linear trend found between the mean CAPE distress score (p=0.057, β=-0.108) and IQ. A significant and inverse linear relation was found for Delusions (p=0.040, β=-0.112) and Paranormal Belief (p=0.006, β=-0.143).
Psychopathology
In the presence of psychopathology a higher mean CAPE frequency score was found for Paranoia (3.00 vs. 2.66, p=0.038) and the mean CAPE distress score was significantly higher (3.47 vs. 4.68, p=0.010).
Although higher mean CAPE frequency scores were found in the presence of a specific diagnosis, differences in mean CAPE frequency scores for specific diagnoses were not found to be significant.
In the presence of a Mood Disorder a significant higher mean CAPE frequency score was found for Paranoia (3.52 vs. 2.88, p=0.018). A borderline significant higher mean CAPE distress score was found for Paranoia in the presence of a Mood Disorder (2.91 vs. 2.18, p=0.055). A significant higher mean CAPE distress score was found for Paranoia in the presence of an Anxiety Disorder (3.31 vs. 2.18, p=0.003).
The mean CAPE distress score was significantly higher in the presence of ASS (5.17 vs. 4.45, p=0.012). For the other diagnoses no significant results were found, not even for psychotic disorder.
Impairment and need for care
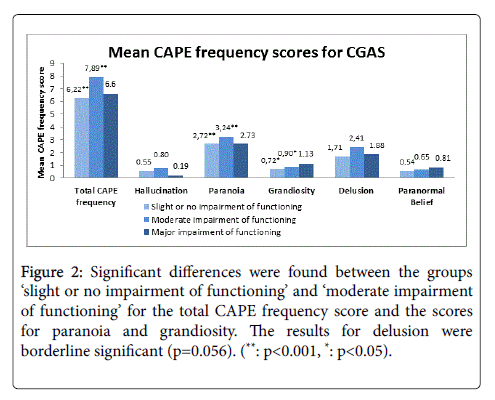
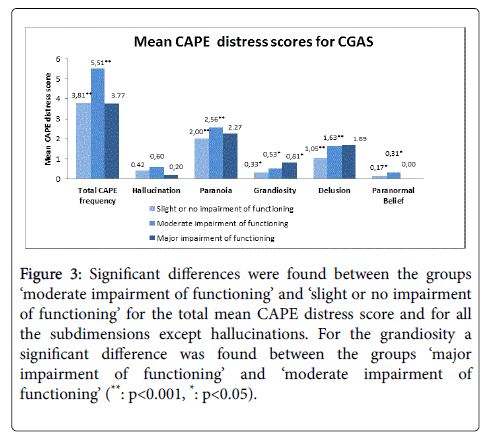
A significant higher mean CAPE frequency score was found for the CGAS group ‘moderate impairment of functioning’ compared to the group with ‘slight or no impairment of functioning’(Figure 2). A significant higher mean CAPE distress score was found for the CGAS group ‘moderate impairment of functioning’ compared to the group ‘slight or no impairment of functioning’ (Figure 3).
Figure 2: Significant differences were found between the groups ‘slight or no impairment of functioning’ and ‘moderate impairment of functioning’ for the total CAPE frequency score and the scores for paranoia and grandiosity. The results for delusion were borderline significant (p=0.056). (**: p<0.001, *: p<0.05).
Figure 3: Significant differences were found between the groups ‘moderate impairment of functioning’ and ‘slight or no impairment of functioning’ for the total mean CAPE distress score and for all the subdimensions except hallucinations. For the grandiosity a significant difference was found between the groups ‘major impairment of functioning’ and ‘moderate impairment of functioning’ (**: p<0.001, *: p<0.05).
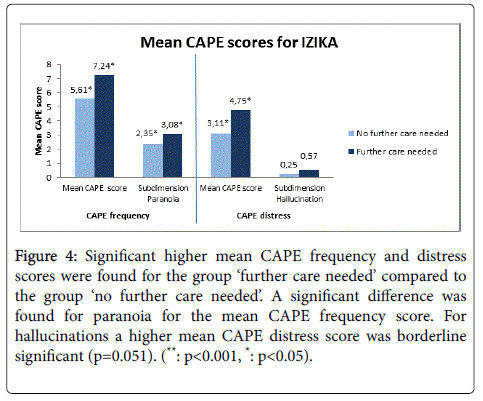
For the CASII a significant higher mean CAPE frequency score was found for the group ‘further care needed’ compared to the group ‘no further care needed’. A significant higher mean CAPE distress score was found for the group ‘further care needed’ compared to the group ‘no further care needed’ (Figure 4).
Figure 4: Significant higher mean CAPE frequency and distress scores were found for the group ‘further care needed’ compared to the group ‘no further care needed’. A significant difference was found for paranoia for the mean CAPE frequency score. For hallucinations a higher mean CAPE distress score was borderline significant (p=0.051). (**: p<0.001, *: p<0.05).
Discussion
Prevalence of positive psychotic experience and associated distress
The majority (94.2%) of adolescents in this clinical sample reported at least one PLE at least ‘sometimes’. This result is comparable to what has been found in former general and clinical population studies [1,3]. Still 62.3% of the population reported at least one PLE at least ‘often’, which was a higher rate than found in the general population (39-43%) [1]. The 90th percentile was found to be higher than in general population (14 vs. 9 PLEs) [1]. These results suggest that the occurrence of minimum 1 PLE is comparable in a clinical and general population, however, in the clinical group the overall amount and frequency of PLE's are higher compared to the general population.
Although comparable data on distress were not available from the general population, the rate of distress is expected to be higher in clinical populations in comparison to non-clinical populations, based on higher CGAS scores in a clinical population and the relation of CGAS with distress. The majority of adolescents in this clinical sample reported at least ‘a bit distress’ for at least one PLE. Half (51%) of our population reported to be at least ‘quite distressed’ for at least one PLE. The 90th percentile of experiences associated with a certain degree of distress was 10 out of 20 experiences.
Distress
The frequency of PLEs in total and in all subdimensions shows a significant linear relation with degree of distress, suggesting that distress is being mediated by the frequency of experiences as has been described in literature [19]. The strength of the relation between frequency and distress is higher for hallucinations, delusions and Paranoia. It is lower for grandiosity and paranormal belief. Similar results were found in literature [1,3] and were found to be significant concluding that subdimensions as grandiosity and paranormal belief are less clinically relevant. Recent studies have proposed new structures eliminating those clinically less significant subdimensions [11,20].
Gender, age and IQ differences
The gender difference reported in literature [1,21-23] was also found in our study. Girls reported significantly more PLEs than boys (resp. 8.38 vs. 6.39) and reported significantly higher distress rates (6.17 PLEs vs. 3.95 PLEs). The previous is in line with former literature suggesting that adolescence shows to be a more stressful period for girls and that the higher rates of Mood Disorders in girls might give rise to affect driven changes in salience [1]. Affective dysregulation is described in literature to coexist with reality distortion due to the effect of emotional state and combined associated beliefs on logical reasoning. These effects may give rise to an attributional bias of emotional salience to neutral or ambiguous stimuli. In individuals with genetic vulnerability for psychotic experiences, misassignment for internal stimuli may lead to the appearance of hallucinations, for external stimuli it may lead to the appearance of delusions [24].
No linear relation of PLEs with age was found in this study. In other studies a significant decrease of PLEs was found with increasing age, mainly between the age of 12 and 16 [1,6,7,25]. A hypothesis for our findings is that in a clinical population there is a higher amount of PLEs, associated with a higher degree of distress, overruling a normal age gradient. The only exception was for the hallucinations, where a significant decrease in psychotic experiences with increasing age was found. This trend has also been described in literature [23,25,26]. Multiple hypotheses can be found for this benign resolution of hallucinations. One hypothesis includes the great level of plasticity of the child or adolescent brain, which provides an innate capacity to recover from exposure to adversity or trauma through brain differentiation. A second hypothesis is the emotional significance of auditive hallucinations as a functional role of companionship, especially in a context of social isolation. This disappears when more mature cognitive strategies are developed. A third hypothesis is found in cognitive and language development. The inner speech that is present in the performance of problem solving tasks is more seen as self-produced with increasing age [27].
Although lower intellectual functioning is a known risk factor for risk of transition to psychosis [28], in accordance to PLES we found no significant relation between the total occurrence of PLEs and IQ. Hallucinations, however, occur more with lower intellectual functioning. Lower intellectual functioning has a relation with the experienced distress caused by the PLEs, borderline significant for the total amount of stress and that in relation to delusions and paranormal beliefs.
Individuals with lower intellectual functioning have less coping mechanisms to comprehend visual or auditive abnormalities, which make them more prone to assigning different significances to external stimuli.
Psychopathology, impairment and need for care
In the presence of psychopathology a significantly higher number of PLEs was found for paranoia and a significantly higher number of PLEs causing distress (resp. 4.68 vs. 3.47 PLEs) was found in total. Specific diagnoses were not significantly linked to a higher number of PLEs .This supports earlier findings in literature [3,26] i.e., that the presence of PLEs is prevalent in a higher rate in a population that is confronted with more difficulties and stress, without being predictive for a diagnosis for any specific diagnosisd especially not being predictive for the presence of a psychotic disorder.
Mood Disorders were significantly associated to a higher amount of paranoid experiences and were borderline significantly associated with the distress caused by these experiences. In the presence of an Anxiety Disorder significantly more distress by paranoid experiences was reported. Former research has shown a higher rate of PLEs in individuals with non-psychotic illnesses, in particular concerning depression or anxiety disorders [29,30]. A first hypothesis is that there is a shared vulnerability to develop symptoms on the continuum between affective dysregulation and reality distortion which leads to a co-occurrence of these symptoms. A second hypothesis is that the depressive or anxiety symptoms are prodromal symptoms of a psychotic disorder. The latter hypothesis cannot account for all cases, since the majority of people presenting affective symptoms do not make the transition to a psychotic disorder. It is however important to identify patients with affective disorders and co-occurrent psychotic symptoms as a higher risk group when it comes to prognosis and severity, whether the evolution goes in the direction of an affective disorder or a psychotic disorder [1,32]. One study showed that the rate of hospitalization for non-affective psychotic disorders occurred faster after baseline than for affective psychotic disorders, showing some degree of specificity of PLEs towards non-affective psychotic disorders [12]. The link between a higher rate of experiences of paranoia with Mood Disorders has already been described in literature [3,33]. Several studies have shown the deficits in Theory of Mind and cognitive empathy in individuals with Mood Disorders [34]. A deficit in perspective taking may make these individuals prone to developing paranoid thoughts. In the presence of an Anxiety Disorder, more distress is reported for paranoia. This is in line with former research showing that anxiety plays a central role in the onset of psychotic symptoms such as paranoia [12].
The presence of more PLEs with distress in ASS is possibly due to the mechanism of misunderstanding and the wrong attributions to external events and stimuli often seen in adolescents with ASS. The unpredictability of these events causes a higher degree of anxiety and distress, which makes them more vulnerable.
A higher degree of distress is inherent to a clinical population and groups with higher rates of distress seem to be more vulnerable. This is reflected in the higher number of positive psychotic experiences in groups with higher impact on functioning in daily life (CGAS) and in groups that are referred to further support or help (CASII). This confirms the hypothesis of distress and occurrence of PLEs and asks for a policy of early detection in clinical populations.
Conclusion
The results of this study demonstrate that PLEs are very frequent in a clinical adolescent population, moreover they are more frequent and more numerous than in non-clinical populations. The lifetime prevalence of one PLE is comparable between clinical and non-clinical populations. PLEs are not predictive for specific psychopathology, but the presence of psychopathology in general leads to a higher amount of distress related to the PLEs reported. The number of PLEs increases when the impact on functioning in daily life is higher and when there is a need for further therapy or support. It is known that not the presence of PLEs determines the evolution to a psychotic disorder, but the distress experienced by them and the persistency [1,9]. Based on the stress-vulnerability model the combination of the persistence of PLEs with distress, the impact on daily life and the need for care increases the risk of psychotic disorder. The impact on daily life and the need for care are influenced by psychopathology in general.
In using the CAPE as an instrument for the evaluation of PLEs in the risk of developing a psychotic disorder, it will be advisable to subject the adolescents with rather high scores (over 90th percentile for frequency (14 PLEs) or distress (10 PLEs)) to subsequent follow-up.
This stands in contrast with the study of 2012 suggesting to choose a low cut-off for the CAPE to provide high sensitivity, even if the number of false positives is high [35]. This study is however conducted in a sample of patients specifically referred for early detection and intervention in psychosis, which is already more specific than a sample in a general outpatient clinic. Using the CAPE in a more general clinical population requires more specificity in order to reduce false positives.
Patients with higher impairment on their daily functioning and a higher need of further support or help may experience higher rates of stress due to their psychopathology which makes them more prone to develop a higher persistence rate of the PLEs over time. Previous literature showed that it might be better to focus only on positive psychotic experiences that are associated with a range of distress, to avoid the stigmatization or pathologizing of normative experiences [33,36]. Introducing a high cut off for follow up could already avoid stigmatization. In general, a high risk group based on the number and distress of experiences can be identified using the CAPE. In addition to following this group over time for persistence rate, it can be advised to make a general risk profile including specific risk factors for psychosis. The CAPE-P 20 can thus function as a tool in early detection of high risk groups for psychosis.
This study shows several limitations. It is a retrograde, crosssectional study that did not include a follow-up over time, thus limiting us to test our proposal about the use of the CAPE in an outpatient clinic. We used a self-report questionnaire which may lead to overestimation. There are, however, studies that point out that the use of a self-report method is equally reliable in comparison to interview based methods [37]. In using the CAPE there is no emphasis on negative symptoms. Another study advised including questionnaires as the Aschenbach (CBCL parent version) to provide that information. Two rating subscales of the CBCL proved to be useful in differentiating youth at risk for psychosis in the general population. The rating scale “thought problems” refers more to the positive symptoms while the rating scale “withdrawn/depressed” is useful in evaluating negative symptoms [38].
Results regarding the relation between psychosis specific risk factors and PLEs in this population will be published in a second article.
Further research will include prevalence of PLEs in a general population in Flanders and prevalence of PLEs in an adolescent psychiatric inpatient clinic to be able to define risk groups in different populations and define specific follow up advices.
References
- Wigman JTW, Vollebergh WAM, Raaijmakers QAW, Iedema J, Van Dorsselaer S, et al. (2011) The structure of the extended psychosis phenotype in early adolescence – A cross sample replication. Schizophrenia Bull 37: 850-860.
- Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, et al. (2012) Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychol Med 42: 1857-1863.
- Yung AR, Buckby JA, Cotton SM, Cosgrave EM, Killackey EJ, et al. (2006) Psychotic-like experiences in nonpsychotic help-seekers: associations with distress, depression and disability. Schizophrenia Bull 32: 352-359.
- Verdoux H, Van Os J, Maurice-Tison S, Gay B, Salamon R, et al. (1998) Is early adulthood a critical developmental stage for psychosis proneness? A survey of delusional ideation in normal subjects. Schizophrenia Res 29: 247-254.
- Harvey MA (2012) Adolescent egocentrism and psychosis, thesis for the doctoral degree of philosophy, University of Birmingham.
- Gale CK, Wells JE, McGee MA, OakleyBrowne MA (2011) A latent class analysis of psychosis-like experiences in the New Zealand Mental Health Survey. Acta Psychiatr Scand 124: 205-213.
- Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L (2009) A systematic review and meta-analysis of the psychosis continuüm: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med 39: 179-195.
- Phillips LJ, Francey SM, Edwards J, McMurray N (2007) Stress and psychosis: towards the development of new models of investigation. Clin Psychol Rev27:307-317.
- Hanssen M, Bank M, Bijl R, Vollebergh W, Van Os J (2005) The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol 44: 181-191.
- Kounali D, Zammit S, Wiles N, Sullivan S, Cannon M, et al. (2014) Common versus psychopathology-specific risk factors for psychotic experiences and depression during adolescence. Psychol Med 44: 2557-2566.
- Nuñez D, Arias V, Vogel E, Gomez L (2015) Internal structure of the Community Assessment of Psychic Experiences- Positive (CAPE-P15) scale: evidence for a general factor. Schizophrenia Res 165: 236-242.
- Werbeloff N, Drukker M, Dohrenwend BP, Levav I, Yoffe R, et al. (2012) Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Arch Gen Psychiatry 69:467-475.
- CAPE, Community assessment of psychotic experiences.
- Goodman R, Ford T, Richards H, Gatward R, Meltzer H (2000) The Development and Well-Being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry 41: 645-655.
- Wechsler D (1992) Wechsler Intelligence Scale for Children - Third Edition UK. London: The Psychological Corporation
- Shaffer D, Gould MS, Bird H, Fisher P (1983) Children’s Global Assessment Scale. Adaptation of the Adult Global Assessment Scale.
- Uvin K, Naessens B, Deboutte D (2011) Instrument om de intensiteit van hulpverlening voor kinderen en adolescenten na te gaan (IZIKA(CASII)). Dutch Translation.
- SPSS Inc., Chicago, IL, USA.
- Hanssen M, Peeters F, Krabbendam L, Radstake S, Verdoux H, et al.(2003) How psychotic are individuals with non-psychotic disorders? Soc Psychiatry Psychiatr Epidemiol 38: 149-154.
- Capra C, Kavanagh D, Hides L, Scott J (2013) Brief screening for psychosis-like experiences. Schizophrenia Res 149: 104-107.
- Yung A, Nelson B, Baker K, Buckby JA, Baksheev G, et al. (2009) Psychotic-like experiences in a community sample of adolescents: implications for the continuum model of psychosis and prediction of schizophrenia. Aust Nz J Psychiatry 43:118-28.
- Armando M, Nelson B, Yung A, Ross M, Birchwood M, et al. (2010) Psychotic-like experiences and correlation with distress and depressive symptoms in a community sample of adolescents and young adults. Schizophrenia Res 119: 258-265.
- David CN, Greenstein D, Clasen L, Gochman P, Miller R, et al. (2011) Childhood onset schizophrenia: High rate of visual hallucinations. J Am Child Adolesc Psychiatry 50: 681-686.
- Van Rossum I, Dominguez M, Lieb R, Wittchen H, Van Os J (2011) Affective dysregulation and reality distortion: a 10-year prospective study of their association and clinical relevance. Schizophrenia Bull 37: 561-571.
- Kelleher I, Devlin N, Wigman HTW, Kehoe A, Murtagh A, et al. (2014) Psychotic experiences in a mental health clinic sample: implications for suicidality, multimorbidity and functioning. Psychol Med 44: 1615-1624.
- Brandizzi M, Schultze-Lutter F, Masillo A, Lanna A, Curto M et al. (2014) Self-reported attenuated psychotic-like experiences in help-seeking adolescents and their association with age, functioning and psychopathology. Schizophrenia Res 160: 110-7.
- Rubio JM, Sanjuan JS, Florez-Salamanca L, Cuesta MJ (2012) Examining the course of hallucinatory experiences in children and adolescents: a systematic review. Schizophrenia Res 138: 248-254.
- Gur RE (2014) Early detection of psychosis: challenges and opportunities. Curr Behav Neurosc Rep1: 117-124.
- Varghese D, Scott J, Welham J, Bor W, Najman J, et al. (2011) Psychotic-Like Experiences in Major Depression and Anxiety Disorders: A Population-Based Survey in Young Adults. Schizophrenia Bull 37: 389-393.
- Hanssen M, Peeters F, Krabbendam L, Radstake S, Verdoux H, et al. (2003) How psychotic are individuals with non-psychotic disorders? Soc Psychiatry Psychiatr Epidemiol 38:149-154.
- Wigman JTW, Van Nierop M, Vollebergh WAM, Lieb R, Beesdo-Baum Ket al. (2012) Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk and severity- implications for diagnosis and ultra-high risk research. Schizophrenia Bull 38: 247-257.
- Verdoux H, Van Os J,Maurice-Tison S, Gay B, Salamon R, et al. (1999). Increased occurrence of depression in psychosis-prone subjects: A follow-up study in primary care settings. Compr Psychiatry 40: 462-468.
- Barragan JM (2013) Psychotic –like experiences and psychometric schizotypy: their relationships with depressive symptoms and theory of mind in adolescents from the general population. Doctorado en psychologia clinica y de la salud. Universidad Autonoma de Barcelona.
- Epa R, Dudek D (2015) Theory of mind, empathy and moral emotions in patients with affective disorders. Arch Psychiat Psychother 2: 49-56.
- Mossaheb N, Becker J, Schaefer M, Klier CM, Schloegelhofer M et al. (2012) The Community Assessment of Psychic Experience (CAPE) questionnaire as a screening-instrument in the detection of individuals at ultra-high risk for psychosis. Schizophrenia Res 141: 210-214.
- Kline E, Thompson E, Bussell K, Pitts SC, Reeves G, et al. (2014) Psychosis-like experiences and distress among adolescents using mental health services. Schizophrenia Res 152: 498-502.
- Linscott RJ, Van Os J (2013) An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med 43: 1133-1149.
- Simeonova DI, Nguyen T, Walker EF (2014) Psychosis risk screening in clinical high-risk adolescents: a longitudinal investigation using the Child Behavior Checklist. Schizophr Res 159: 7-13.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 3152
- [From(publication date):
April-2017 - Apr 21, 2025] - Breakdown by view type
- HTML page views : 2338
- PDF downloads : 814