Research Article Open Access
The National Quality Plan and More Caesarean Sections, Less Wound Infections,more Gestational Diabetes (GDM) and Fewer Smokers in Northern Norway: A Registry-based Retrospective Study
Jan Norum*, Tove Elisabeth Svee, Ingrid Petrikke Olsen, Margit Steinholt, Merethe Kumle and Randi Spørck
Institute of Clinical Medicine, Faculty of Health Sciences, UiT - The Arctic University of Norway, Tromsø, Norway
- *Corresponding Author:
- Jan Norum
Institute of Clinical Medicine
Faculty of Health Sciences
UiT - The Arctic University of Norway
Tromsø, Norway
Tel: 4795404205
E-mail: Jan.Norum@helse-nord.no
Received Date: July 04, 2016; Accepted Date: July 20, 2016; Published Date: July 26, 2016
Citation: Norum J, Svee TE, Olsen IP, Steinholt M, Kumle M, et al. (2016) The National Quality Plan and More Caesarean Sections, Less Wound Infections, more Gestational Diabetes (GDM) and Fewer Smokers in Northern Norway: A Registry-based Retrospective Study. J Preg Child Health 3:268. doi:10.4172/2376-127X.1000268
Copyright: © 2016 Norum J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Background: The Ministry of Health and Care Service’s plan for improved maternity and delivery care was implemented in Northern Norway in March 2012. Selection criteria were standardized and economic resources allocated. Methods: We explored the effects in a retrospective quality of care study employing data from the Medical Birth Registry of Norway (MBRN). The prior study (2009-11) was compared with the 2012-14 period. The levels of care were Midwife administered maternity units (MAMU), Departments of Obstetrics and Gynaecology (DOG) and Regional Clinics of Obstetrics and Gynaecology (RCOG). National data on post-caesarean surgical wound infection (2009-2014) was added. Quality of care was defined as rate of multiple pregnancies, eclampsia, vacuum or forceps assisted delivery, births during transportation, caesarean section rate, post-caesarean wound infection, perineal rupture, smoking habits, body mass index (BMI), Apgar score <7, birth weight <2.5 kg and stillbirth. There were in total 30,516 and 362,013 births during study period in Northern Norway and Norway, respectively. Results: In Northern Norway, the quality commitment did not affect the balance between levels of care. In the northern region, birth weight<2.5 kg, stillbirth rates and Apgar score <7 was stable and similar to national figures. Caesarean section rate increased in the northern region from 16.1% to 16.9% (P=0.04). It dropped at the MAMUs (2.8% vs. 1.4%, P=0.019), and increased at the RCOGs (17.4% vs. 18.2%, P=0.017). Post-caesarean wound infection rate was reduced both in Northern Norway (10.5% vs. 8.3%, P=0.069) and nationally (7.1% and 4.6%, P<0.001). The use of forceps and vacuum assisted delivery was stable and below national levels. Perineal rupture grade 3 and 4 and eclampsia rates were unchanged. However, gestational diabetes mellitus (GDM) rate increased from 1.7% to 2.9% (P<0.001), but body mass index (BMI) did not change. Number of smokers dropped (11.6% vs. 8.2%, P<0.001). Conclusion: The national commitment did not alter the balance between institutions in Northern Norway. The caesarean section rate increased at the RCOGs and the Apgar score did not improve. GDM rate increased and the number of smokers dropped.
Keywords
Quality; Obstetrics; Norway; Registry; Gestational diabetes; Body mass infection
Abbreviations
RCOG: Regional Centre for Obstetrics and Gynaecology; DOG: Department of Obstetrics and Gynaecology; MAMU: Midwife Administered Maternity Unit, MBRN: Medical Birth Registry of Norway; NNRHA: Northern Norway Regional Health Authority; NOIS: Norwegian Surveillance Program for Infections in Hospitals
Background
Northern Norway covers almost half of Norway’s land mass and is about two-thirds of the size of the UK. The population is only 480.740 inhabitants (as 1st of January 2015), one fourth of whom live in the main cities (Bodø and Tromsø). About 2,500 people live in the Norwegian Arctic, mainly on the Svalbard islands. Vast distances have been a constant challenge to the Northern Norwegian specialised health care in terms of quality of care, costs and logistics. The area has a subarctic and arctic climate that may cause logistic hindrances, especially during winter time.
In the specialized health care, maternity care and delivery service have been organized in three levels of care. Level 1: Midwife administered maternity units (MAMUs). Level 2: Department of obstetrics and gynaecology (DOG), Level 3: Regional centre for obstetrics and gynaecology (RCOG). To secure high quality of care, Norwegian women have been selected to institution/unit of delivery according to risk factors [1,2], but none of them have been national common guidelines. Those at low risk may deliver at MAMUs. Women with intermediate risk are referred to second-level perinatal care units at local hospitals, and those with high risk to a regional specialist hospital for delivery. Whereas the MAMUs generally are staffed withs midwives and have a general practitioner on duty available in the community, they have no gynaecologist/obstetrician in the unit. The second level has such a specialist on duty 24 h a day and emergency caesarean section may be performed within 15-20 min at any time. The regional specialist hospital is superior to the departments at local hospitals in terms of access to paediatricians on duty and a paediatric intensive care unit. In addition to being a regional centre, the RCOG serve as a local hospital for women in the hospital’s catchment area. Consequently they also handle low-risk cases.
In 2009, the Ministry of Health and Care Services launched a plan for improved maternity and delivery care entitled ‘A Happy Occasion’ and incorporated it in the ‘Coordination Reform’ [3,4]. The main aim was to improve continuous maternity, delivery and postpartum care. The new national guidelines included a detailed description of key staff available at the different level of care; at the RCOG a minimum of one obstetrician present at the unit 24 h a day, at least a team of four gynaecologists at each DOG, at least two midwives constantly available at each delivery care unit. Midwives should also be available to accompany women in labour during transport and referral to delivery units. Anaesthesiologist or nurse anaesthetist must be available within a defined time frame as caesarean section must be performed within 15 min after decision, when necessary.
Based on the national plan, new selection criteria and guidelines for transportation were implemented in Northern Norway the 1st of March 2012 [5]. A registry-based study on the quality of maternal health care services prior to the introduction of the national plan has been reported [6]. Now, we aimed to employ these results as the comparator and explore whether the national quality of care commitment had resulted in any centralisation or gain in quality of care, especially in the northern region. The hypothesis was that a centralization effect had occurred and quality of care had been improved.
Methods
Study design
This study was designed as a registry-based retrospective quality of care study focusing maternal health care services. Norway and especially the northern region was explored. The hypothesis was that following the prior study [6] and the implementation of the nationals quality plan [5] a centralization effect had occurred and quality of care had been improved.
Norway has a population of 5.2 million inhabitants and is divided into four health regions (southeast, western, central and northern region). The northern region has only 9.4% of the total population, and people are scattered within an area of 112,946 km2, 45% of Norway’s land mass. To serve the population, the Northern Norway Regional Health Authority (NNRHA) trust runs six midwife managed maternity units (MAMU) (Brønnøysund, Mosjøen, Nordland hospital (NH) Gravdal, Lenvik, Sonjatun, Alta), seven departments of obstetrics and gynaecology (DOG) [Helgeland hospital (HH) Sandnessjøen, HH Rana, Nordland hospital (NH) Vesterålen, University hospital of north Norway (UNN) Harstad, UNN Narvik, Finnmark hospital (FH) Hammerfest, FH Kirkenes] and two regional centres (RCOG) (NH Bodø, UNN Tromsø). The hospitals are organized in four hospital trusts: Finnmark hospital, University hospital of North Norway, Nordland hospital and Helgeland hospital. The selection concerning level of care starts at the first visit to GP or midwife, and is a continuous process during pregnancy and labour. Possible occasions are the follow up visits in primary health care or at ultrasound screening at 18th week of pregnancy. Based on the national plan, national and regional selection criteria and guidelines for transportation were implemented in Northern Norway the 1st of March 2012 [5]. A short summary is shown in Table 1.
| May give birth at midwife administered maternity units (MAMU) Healthy multipara Healthy primipara<35 years A normal pregnancy Facial presentation Pre-pregnancy body mass index (BMI) 27-30, after consulting DOG. No disease that may cause complications. Prior normal pregnancy/birth Birth starts spontaneously between 36w + 0 days and 41w +3 days. Defined as a low risk birth when labor starts. Prior support by forceps or vacuum, but not considered necessary this time. May give birth at departments of obstetrics and gynecology (DOG) Age < 18 years and primipara>35 yrs. Hypertension, mild or moderate preeclampsia. Serious preeclampsia. Pre-pregnancy BMI <19,>30 and <35, 35-40 after consulting RCOG. Estimated birth weight >4.5 kilo Thrombophilia with moderate risk Prior caesarean section or prior serious complications during pregnancy and/or delivery.Induced birth. Circumcised women. Birth starts spontaneously between >41w +3days. Mother has experienced less signs of a living fetus during several days. Energy intake regulated gestational diabetes mellitus (GDM). Long lasting rupture of membranes. Pre-term birth >35w + 0 days. Epilepsy without any seizures during pregnancy. Twins >35w. General considerations based on smoking habits and multipara (>4 births) should be added. Shall give birth at Regional Clinics of Obstetrics and Gynaecology (RCOG). Insulin dependent GDM and poorly regulated GDM. Serious preeclampsia. Foetal malformations and need for intervention after birth. Growth retardations and <37w. Multiple births Breech birth Placenta praevia. BMI>40 Preterm birth (<35w + 0 days) Serious diseases affecting mother (cardiac, lung, kidney, thyroid or rheumatic diseases), Other causes: Drug addicted, HIV infection, serious thrombophilia. |
Table 1: The table shows the main national and regional selection criteria implemented in 2012 in Northern Norway.
Data included
In Norway, all births are reported to the Medical Birth Registry of Norway (MBRN) (www.fhi.no/mfr). The registry was established in 1967. Today it is a national health registry containing information about all births in Norway. The registry aim to clarify the causes and consequences of health problems related to pregnancy and birth, as well as to monitor the incidence of congenital abnormalities. Data for the study period was available online from the MBRN database (www.fhi/mfr). In this study, we accessed data (as of June 3rd 2015) reported from the 15 institutions in Northern Norway and cumulative data from all institutions in Norway. The results of the prior study (2009-11) [6] was compared with the time period (2012-14) after the introduction of the national quality of care plan. The following data were accessed: Births, frequency of multiple pregnancies, eclampsia, vacuum or forceps assisted delivery, perineal rupture grade 3 (partial or total tear through the anal sphincter) or 4 (grade 3 with extension through the rectal mucosa), births during transportation, caesarean section rate, post-caesarean wound infection, smoking habits, gestational diabetes mellitus (GDM), body mass index (BMI), Apgar score <7, birth weight <2.5 kg and stillbirth.
The mentioned outcomes were chosen to describe the quality of care as they were available from the MBRN’s online databank. Other factors as atonic uterus, bleeding (500-1500 ml and >1500 ml) and blood transfusion were not available from the online databank and consequently not included in our study.
The Norwegian Surveillance Program for Infections in Hospitals (NOIS) was established in 2005. In this registry, surgical wound infections within 30 days after caesarean section was registered prospectively from Sept 1 to Nov 30 each year. Women were followed up after surgery by mail and a phone call from specialized nurses. Any infection within 30 days after surgery was registered. Superficial infections could be reported by the women themselves, but all other infections had to be confirmed by a medical doctor. Since December 2012, the registration has been performed continuously around the year. We collected these data for the time period 2009-2014. Some minor institutions (Narvik, Lofoten, Sandnessjøen) did not report their figures during the whole study period. They were included with the numbers reported.
Quality control, statistical analysis and authorisation
Individual data are recorded and analyzed by the MBRN. The quality assurance of the primary data included linking to the National Population Register (NPR) to identify and confirm the women and collect available information about date of birth and death (in case of death). Furthermore, the reporting institutions were requested to supply additional information when needed. We accessed anonymous and aggregated data from this open source. Similarly data were accessed from the NOIS-registry. The aggregated data were imported to a database at the NNRHA. Microsoft Excel 2007 version was used for the final database, calculations and statistical analysis. The comparison between subgroups, institutions and health regions with regard to quality of care figures was performed using descriptive statistics and the Chi-square test. Significance was set to 5%.
The network for Enhancing the Quality and Transparency Of health Research’s (EQUATOR) tool, the Reporting of studies conducted using Observational Routinely-collected health Data (RECORD) statement, was employed as a guide [7].
Data from the MBRN was available on the Web free of cost, we imported aggregated data and the study was run as a quality of care analysis. Consequently, no consent of participation, consent for publication or ethical committee or Data Inspectorate approval was necessary. Similarly, no approval from the Regional Committees for Medical and Health Research Ethics (REK) or the Norwegian Social Science Data Services (NSD) was required.
Results
Births and complications
During study period, there were in total 30,516 births in Northern Norway. This accounted for 8.4% of all births in the country. The figures during the two periods were 8.6% (2009-2011) and 8.3% (2012-2014), respectively. There was a 5.3% and 2.4% reduction in the total number of births from the first (2009-2011) to the latter (2012-2014) period in Northern Norway versus Norway, respectively. Absolute figures are shown in Table 2. Within Northern Norway, no significant change of volume of births at each level of care was observed. The figures at MAMUs were 8.6% and 8.3% (P=0.43), DOGs 43.0% and 43.1% (P=0.99) and RCOGs 48.4% and 48.6% (P=0.71).
| Births | Caesarean (%) | Vacuum assisted (%) | Forceps delivery (%) | Apgar score <7 (%) | Weight <2500g (%) | Still-birth per 1000 | Perineal rupture G 3-4 (%1) | Eclampsia per 1000 | Pregancy induced diabetes per 1000 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Institutions | 2009-11 | 2012-14 | 2009-11 | 2012-14 | 2009-11 | 2012-14 | 2009-11 | 2012-14 | 2009-11 | 2012-14 | 2009-11 | 2012-14 | 2009-11 | 2012-14 | 2009-11 | 2012-14 | 2009-11 | 2012-14 | 2009-11 | 2012-14 |
| FHKirkenes | 681 | 577 | 18,9 | 16,3 | 8,4 | 4,8 | 0,0 | 0,0 | 0,9 | 0,5 | 2,6 | 0,5 | 1,5 | 1,5 | 1,3 | 2,5 | 0,0 | 1,8 | 9,0 | 31,9 |
| FH Hammerfest | 1354 | 1231 | 19,4 | 17,7 | 5,5 | 6,8 | 0,5 | 0,7 | 2,8 | 1,5 | 4,2 | 3,3 | 5,1 | 9,3 | 1,9 | 2,1 | 0,7 | 1,6 | 20,8 | 27,7 |
| Alta* | 289 | 276 | 0 | 0,0 | 0,0 | 0,0 | 0,0 | 0,0 | 2,8 | 1,7 | 0,7 | 2,2 | 0,0 | 0,0 | 0,7 | 0,4 | 0,0 | 3,6 | 10,4 | 7,3 |
| Sonjatun* | 76 | 92 | 0 | 0,0 | 1,3 | 1,2 | 0,0 | 0,0 | 1,3 | 2,3 | 1,3 | 0,0 | 0,0 | 0,0 | 1,3 | 0,9 | 13,0 | 0,0 | 26,0 | 24,4 |
| UNNTromsø | 4390 | 4135 | 18,3 | 20,6 | 5,3 | 6,1 | 0,1 | 0,3 | 2,9 | 2,9 | 7,1 | 7,4 | 4,5 | 5,2 | 1,5 | 1,9 | 0,5 | 1,2 | 16,1 | 27,3 |
| UNNNarvik | 786 | 683 | 13,5 | 16,6 | 6,0 | 5,9 | 0,3 | 0,2 | 1,1 | 1,6 | 1,4 | 1,0 | 5,1 | 4,4 | 1,2 | 1,4 | 1,3 | 1,5 | 14,1 | 13,3 |
| UNNHarstad | 1164 | 1076 | 17,4 | 20,4 | 6,7 | 5,4 | 0,0 | 0,1 | 0,9 | 1,6 | 2,5 | 1,6 | 2,6 | 3,7 | 2,1 | 2,5 | 0,9 | 0,0 | 12,9 | 16,9 |
| Lenvik* | 317 | 324 | 0 | 0,0 | 0,6 | 0,3 | 0,0 | 0,0 | 0,9 | 0,0 | 0,6 | 0,0 | 0,0 | 0,0 | 1,6 | 0,3 | 0,0 | 0,0 | 0 | 6,4 |
| NH Bodø | 3222 | 3052 | 15,7 | 16,3 | 9,0 | 8,8 | 0,3 | 0,6 | 2,3 | 2,0 | 7,4 | 7,3 | 4,8 | 2,9 | 1,9 | 1,7 | 0,6 | 1,0 | 28,5 | 48,5 |
| NH Vesterålen | 850 | 959 | 17,5 | 19,4 | 4,4 | 7,9 | 0,8 | 0,2 | 1,9 | 1,1 | 2,6 | 1,1 | 7,0 | 2,1 | 2,5 | 2,7 | 0,0 | 0,0 | 10,7 | 15,8 |
| NH Lofoten* | 370 | 302 | 11,8 | 6,1 | 3,8 | 3,0 | 0,5 | 0,3 | 1,9 | 1,1 | 1,9 | 2,3 | 2,7 | 0,0 | 3,4 | 2,2 | 0,0 | 0,0 | 8,2 | 13,5 |
| HH Rana | 1132 | 1085 | 15,2 | 15,9 | 7,9 | 9,3 | 0,4 | 0,2 | 1,9 | 1,5 | 1,8 | 1,6 | 2,6 | 2,8 | 2,5 | 3,1 | 0,9 | 0,0 | 9,7 | 24,1 |
| HHSandnessjøen | 792 | 765 | 17,6 | 15,7 | 7,6 | 6,6 | 0,3 | 0,1 | 2,5 | 1,6 | 2,1 | 2,3 | 8,8 | 2,6 | 1,5 | 2,7 | 1,3 | 0,0 | 15,2 | 48,5 |
| HHMosjøen* | 171 | 117 | 0 | 0,0 | 0,0 | 0,9 | 0,0 | 0,0 | 0.0 | 0,0 | 0,5 | 0,6 | 0,0 | 0,0 | 0,6 | 0,0 | 0,0 | 0,0 | 11,8 | 34,2 |
| Brønnøysund* | 123 | 117 | 0 | 0,0 | 0,0 | 0,0 | 0,0 | 0,0 | 0.0 | 1,7 | 0,0 | 0,9 | 0,0 | 0,0 | 0,0 | 0,0 | 0,0 | 0,0 | 0 | 8,6 |
| Northern Norway | 15730 | 14786 | 16,1 | 16,9 | 6,3 | 6,6 | 0,2 | 0,3 | 2,1 | 1,9 | 4,7 | 4,5 | 4,3 | 3,7 | 1,8 | 2,0 | 0.6 | 0,9 | 16,9 | 29,1 |
| Norway | 183737 | 178276 | 16,7 | 16,5 | 8,3 | 8,8 | 1,7 | 1,5 | 1,8 | 1,8 | 5,0 | 4,9 | 3,9 | 4,0 | 2,3 | 2,0 | 0,5 | 0,6 | 17,7 | 30,5 |
Table 2: Number of births, stillbirths and other birth associated factors in Northern Norway and Norway in the time periods 2009-2011 and 2012-2014, respectively (National Norwegian Birth Registry as of 7th July 2015); *-Midwife administered maternity unit (MAMU) The percentage was calculated according to the number of vaginal births).
The northern region diverged from the national figures in several aspects. Multiple pregnancies were less common (P<0.001). The mean percentage was 1.3% (range 1.1-1.5%) and 1.7% (range 1.6-1.8%), respectively. The use of forceps delivery was less frequent in Northern Norway (0.3% vs. 1.6%, P<0.001), but did not alter significantly during study period (P=0.11). None of the northern institutions reached the national mean level. Vacuum assisted delivery was also less common in our region (6.6% versus 8.6%) (P<0.001) and did not change during study period (P=0.23). Only three of the northern institutions reached the national level. Details are shown in Table 2. Apgar scores below 7 are considered moderately low (critically low<4). The percentage of Apgar score <7 (measured five minutes after birth) was higher in Northern Norway than the national figures (1.8 vs. 2.0, P<0.001). There was no difference in Northern Norway between the two study periods (2.1% vs. 1.9%, P=0.21). Due to selection criteria, the three hospitals (FH Hammerfest, UNN Tromsø and NH Bodø), with a paediatric unit, had consequently more newborns with lower Apgar score than the others. Details are shown in Table 2.
Low birth weight<2.5 kg, was less common in our region as compared with national figures (4.6 vs. 5.0%) (P=0.006). According to the national guidelines and selection criteria, these children should be delivered in RCOGs or DOGs if possible. Consequently, the RCOGs did have the greatest share of this subgroup (RCOG-7.3%, DOG-2.2%, P<0.001)). Details are shown in Table 2.
During study whole period, there were no difference in stillbirth rate per 1,000 births between the northern region and Norway (P=0.83) or the DOGs and RCOGs (P=0.93). Furthermore, no significant change was observed during study period (Northern Norway P=0.40, Norway P=0.67). Details are shown in Table 2. This indicates that maternity care and delivery services are of the same quality throughout all of Norway. The rates of perineal rupture grade 3 and 4 were similar in the northern region as observed in Norway in general. In Northern Norway, there was no difference between the two periods analyzed (P=0.21), but perineal rupture was less frequent at the RCOGs than at the DOGs (1.8% vs. 2.2%, P=0.02). More details are given in Table 2.
The frequency of eclampsia was similar in our region as in the other health regions (0.8 vs. 0.5 per 1,000, P=0.10). There were no difference between study periods (0.6 vs. 0.9 per 1,000, P=0.44). Details are shown in Table 2.
Centralisation of births may increase the number of unplanned deliveries outside institutions due to longer distances and consequently increased time of travelling. However, such a trend was not observed in our study. During both time periods (2009-2011 and 2012-2014) 0.8% of the deliveries in Northern Norway were unplanned outside institutions (40 at home, 57 during travel, and 33 unspecified) (44 at home, 51 during travel, 25 unspecified). The corresponding national figure was 0.7% in both periods (539 at home, 540 during transport, and 150 unspecified) (543 at home, 421 during transport, 239 unspecified). The difference was statistically significant (P=0.001). The difference is probably due to the weather conditions and the geography of Northern Norway.
Caesarean section
There were no differences in the use of caesarean section in Northern Norway and Norway (P=0.61). The frequency (all Robson groups) of caesarean section in Northern Norway increased from 16.1% to 16.9% (P=0.04). In the Northern Norwegian figures, women from Africa south of Sahara, South-East Asia, East Asia, Oceania, Latin-America and Caribbean experienced a higher frequency of caesarean section (24.1%, range 23.4-30.6%, P<0.001). Comparing the various levels of care in Northern Norway, there was a planned significant drop in caesarean sections at the MAMUs (2.8% vs. 1.4%, P=0.019), no change at the DOGs (17.2% vs. 17.6%, P=0.51) and an increase at the RCOGs (17.4% to 18.8%, P=0.017). Except for NHLofoten, no MAMU had any caesarean section performed. [Due to distance to nearest DOG and rough weather conditions, especially during winter times, NH-Lofoten has a gynaecologist on duty who may perform caesarean sections]. This model is not present at any other MAMU and it was not recommended in the national plan.
According to the NOIS data, the percentage of infections following caesarean infection dropped from 10.5% to 8.3%, but it did not reach statistical significance (P=0.069). However, the national figure was significantly lowered (7.1% and 4.6%, P<0.001). Details are shown in Table 3.
| 2009-11 | 2012-14 | |||||
|---|---|---|---|---|---|---|
| Institution | No CS | No infections | % | No CS | No infections | % |
| FH Kirkenes | 33 | 2 | 6.1 | 29 | 0 | 0 |
| FH Hammerfest | 71 | 13 | 18.3 | 177 | 22 | 12.4 |
| UNN Tromsø | 203 | 35 | 17.2 | 677 | 62 | 9.2 |
| UNN Narvik | 20 | 3 | 15 | 85 | 10 | 11.8 |
| UNN Harstad | 54 | 2 | 3.7 | 179 | 9 | 5 |
| NH Bodø | 133 | 2 | 1.5 | 387 | 21 | 5.4 |
| NH Vesterålen | 25 | 0 | 0 | 61 | 3 | 4.9 |
| NH Lofoten* | 7 | 0 | 0 | 5 | 0 | 0 |
| HH Rana | 35 | 4 | 11.4 | 140 | 10 | 7.1 |
| HH Sandnessjøen | - | - | 24 | 5 | 20.8 | |
| Northern Norway | 581 | 61 | 10.5 | 1,764 | 142 | 8 |
| Norway | 6,870 | 489 | 7.1 | 19,946 | 919 | 4,6 |
Table 3: The table shows the percentage of infections after caesarean section (CS) according to institutions and time period. The national figure was significantly lowered (P<0.001), but not the Northern Norwegian ones (P=0.097); *Midwife administered maternity unit (MAMU).
Gestational diabetes
One of the major findings in this study was a significant increase of GDM (P<0.001). The absolute figure rose from 1.7% to 2.9%. A similar trend was also observed at the national level (1.8% to 3.1%). There were no difference between Northern Norway and the other regions (P=0.17). Due to the selection criteria, GDM was more common in RCOGs than in DOGs (2.9% vs. 1.9%, P<0.001). Details are presented in Table 2.
The incidence of diabetes increases with age. Comparing age subgroups of the two cohorts (2009-2011 and 2012-2014) of mothers, the percentage of women aged 30-34 years (26.9% vs. 27.4%), 35-39 years (14.7% vs. 14.1%) and 40-44 years (2.9% vs. 3.0%) did not show any significant change. Consequently, a possibly more elderly population of mothers during the last period (causing an increased frequency of GDM) could not be indicated.
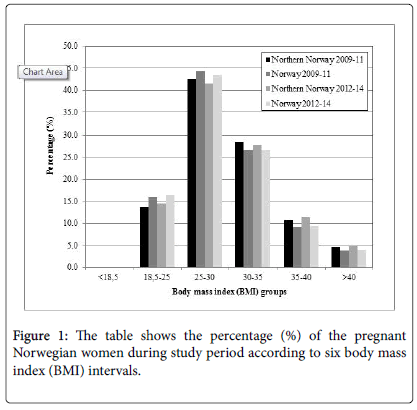
Based on this finding, it is of interest to access and analyse body mass index (BMI) data as there is a well-known correlation between increasing BMI and GDM. The largest group were in the BMI interval 25-30. We did not detect any increasing percentage of women in the BMI>35 group during study period. Details are shown in Figure 1. Consequently, BMI do not explain the revealed increase in GDM.
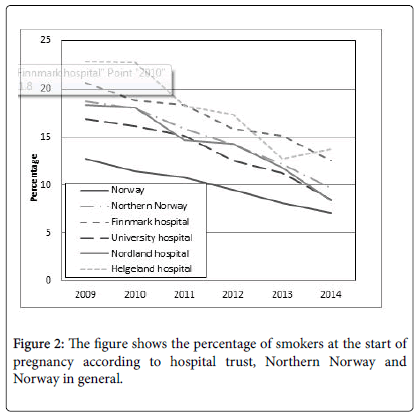
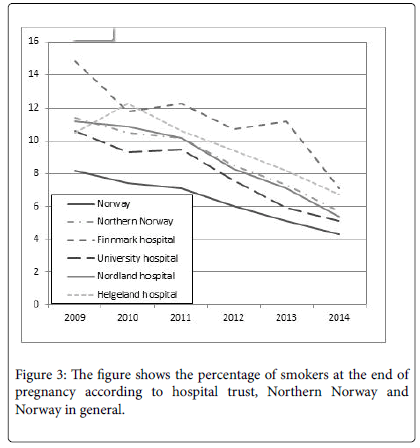
Looking at smoking habits, the share of smokers among pregnant women at start of pregnancy dropped significantly between the study periods, both nationally (11.6% vs. 8.2%, P<0.001) and in Northern Norway (17.5% vs. 12.0%, P<0.001). A similar situation was also confirmed at the end of pregnancy. Details are shown in Figures 2 and 3.
Discussion
Key results
In this study, we have revealed that the Norwegian national quality commitment did not influence on most quality of care indicators. This strongly indicates a delivery service of high quality prior to the introduction of the national plan. However, some significant changes were observed after the introduction of the national plan. The percentage of GDM increased, fewer pregnant women were smokers, more caesarean sections were conducted, and there was a decrease in post-caesarean surgical wound infections.
Limitations and strengths
This study has both limitations and strengths. As mentioned in the methods section, more outcomes could beneficially have been included. Furthermore, we analysed aggregated data both from the MBRN and the NOIS database. Consequently, sub-analyses on specific subgroups could not be performed. We analysed a limited time period (2009-2014). Trend perspectives will need a time perspective of about 10-15 years and could therefore not be analysed in this study. It should also be kept in mind that data included in the NOIS and MBRN registries are collected for the monitoring of quality of care and not for clinical studies. In this setting the main factors will be effects, safety, availability, equality, patient focus and effectiveness. Furthermore, other external factors may have influenced on the trends revealed. In example the growing focuses on quality of care based on the supervision reports published by the Norwegian Board of Health Supervision (HBHS) and the data from the Norwegian System of Patient Injury Compensation (NSPIC) [8].
The strength of this study is that it included all births in Norway and Northern Norway. By law Norwegian medical institutions and doctors must register every birth and its outcome. This fundament of the MBRN is one of the reasons for their good quality of data. The fact that the MBRN data are reported, in annual reports and as easily available online services to institutions and medical doctors, may improve quality and strengthen the reporting doctors’/institutions’ ownership and interest in high quality data. On the other hand, some workers have commented that a heavy burden of registration work may influence negatively on the quality of the reporting.
Neonatal mortality or maternal mortality was not monitored in our survey. The Norwegian figure of neonatal mortality was not available at hospital trust level. According to the MBRN (www.mfr.no), the neonatal mortality rate per 1,000 births in the time period 2002-2011 was 2.3 and 2.2 in Norway and Northern Norway, respectively. The corresponding late neonatal mortality rate (7-27 days after delivery) figures were 0.5 and 0.6 respectively. Maternal mortality ratio (MMR) has been analyzed in 22 European countries [9]. The overall figures were 6.3 per 100,000 live births (range 0-29.6). The Norwegian figure in this survey was 3.5. This strongly indicated maternal death is a rare occasion and not a suitable marker to analyse within the short time interval of our study.
Interpretation
We assumed that the new selection criteria would influence the balance between the three levels of care. A ten percent drop in the number of births at the MAMUs was anticipated. Looking at the figures, such a trend was observed at the MAMUs in Mosjøen and Lofoten, but other locations strengthened their positions (Finnsnes and Sonjatun). Women´s choice (when appropriate according to selection criteria, they may choose level of care) may have been the main factor counteracting centralisation. As we included anonymous aggregated data, specific analysis of a centralization effect based on subgroups could not be performed.
It could be argued that the selection criteria were sabotaged. However, based on our close dialogue with the members of the regional council of obstetrics and gynaecology in Northern Norway and the leading clinicians within the region, we have no such indication. Based on the feedback from the clinicians, we believe a centralisation of the high risk pregnancies did occur. At the same time more women delivered at the MAMUs. The new criteria included low risk primiparas to give birth at the lowest level of care.
In Northern Norway, the caesarean section rate increased from16.1% to 16.9%. Since 2001, the national figure of caesarean section has been stable around 16-17% (www.fhi.no). The causal correlation between caesarean section rate and the quality plan could be questioned in our study. When introducing the national quality plan, a centralisation effect was anticipated and especially the RCOGs may more easily have accepted a growing caesarean section rate without questioning the trend. However, this statement can not be tested in a retrospective study and must be analyzed in randomized clinical trials.
Furthermore, the inter DOGs variation was around 5% (13.5-19.4 % and 15.7-20.4 %) in the two time periods. Within Norway, the lowest figure (12%) has generally been reported from the Western region [10]. The national figures have increased during the last decade [10]. In England, Scotland, Finland, Sweden and Denmark, figures have been reported rising from around 4-5% in 1970 to 20-22% in 2001 [11]. Today, across Europe figures vary widely from about 14% in Nordic countries to 40% in Italy [12]. Avoidance of unnecessary caesarean section has been a quality target [3,13] and has been one among several topics at the International Forum on Quality and Safety in Healthcare’s meetings. Overuse of caesarean section exposes both the mother and the foetus to unnecessary risks. In example, caesarean section may be a risk factor for childhood food allergy and asthma [14-18]. To counteract the rise, policy related interventions include the requirement for a second obstetric opinion, education of health professionals, patient and community education, clinical audit and feedback mechanism, clinical practice guidelines, quality improvements strategies and financial incentives [11,13]. When aiming for a less variation in caesarean delivery rate, the trends needs to be monitored carefully in order to prevent a shift from planned to emergency caesarean delivery, as the latter has additional deliveryrelated risk factors [18]. In the future, we believe second obstetric opinion and clinical audit may be important ways to follow up our inter-DOG variation. Based on our findings, we have already discussed to implement this strategy in Northern Norway. Such an instrument may also be beneficial in the struggle for less post-caesarean wound infections.
In this study, we found a significant increase in gestational diabetes. Several investigators have documented that an increasing prevalence of overweight/obesity, older age at pregnancy and non-Caucasians are important risk factors for GDM [19-21]. Consequently, there are four major causes of an increasing number of gestational diabetes that should be elucidated: A) An increased incidence of diabetes among females of fertile age. B) Increasing age among pregnant women. C) An increasing number of immigrants. D) Improved diagnostics and follow up.
We do not have any national registry of diabetes. However, the Norwegian Prescription database (NPD) offer online access to data on individuals treated with any anti-diabetic drug. In this database, diabetic patients treated with food monitoring (diabetes type 2) alone are not included and this is the most frequent therapy approach for GDM. However, based on the NPD database, we revealed 1.17% and 1.15% of women in Northern Norway aged 20-39 years treated with any anti-diabetic drug during study periods. Consequently, no increased use of anti-diabetic drugs among the female fertile population was observed. This finding is also in accordance with the findings of Strøm et al. [22]. Furthermore, the prevalence of diabetes increases with age in the general Norwegian population. Consequently, an older median age at pregnancy during the last study period would simply cause a raised incidence of gestational diabetes. However, as shown in our study, such a trend was not revealed.
Body mass index (BMI) is a well-known risk factor for gestational diabetes [23-25]. In our study, we accessed data on BMI and did not reveal any difference between the two cohorts. This is also in accordance with the non-changing data on eclampsia [25-25]. Furthermore, there was no difference regarding the share of children born with a weight above 3.5 kg (52% in both time periods). This was also in accordance with the stabilisation of patients with diabetes reported by Strøm et al. [22]. However, the percentage of pregnant women who had their BMI reported varied between 40-70% during study period. Consequently, these data should be handled with caution.
The prevalence of GDM appears to be particularly high among women from South Asia and South East Asia, compared to Caucasian, African-American and Hispanic communities [26,27]. McDonald et al. recently reported that Asian countries have a 3-fold increased risk of GDM compared to women from Australia and New-Zealand [26]. We had limited data on immigrants and their homeland in the MBRN database. Consequently, we could not document whether immigrants from Asia had influenced on the figures. However, 2015-data from Statistics Norway [28] summarized that 13% of the Norwegian population are immigrants and 26% out of them were from Asia. During the time period 2012-14, the figures have been decreasing. Consequently, these figures strongly indicate that immigration cannot explain our findings.
We believe an improved follow-up of pregnant women according to national Norwegian guidelines and selection criteria caused an improved detection of GDM [29-30]. The effect has probably occurred both within hospitals and among GPs. An improved registration of these data in the electronic patient record (EPR) system may also have played a role in this improvement. Recently, a specific journal system (NOKLUS®) for the follow up of patients with diabetes was launched in the primary health care.
In this study, another major finding was the decreasing number of maternal smokers. It could be argued that there are no causal connection between the national quality plan and smoking habits. However, according to the selection criteria, midwives/obstetricians are requested to consider heavy smoking habits as a risk factor when final decision on level of care is to be taken. This focus on smoking could obviously influence on percentage of smokers at the end of pregnancy. Despite a higher percentage of maternal smokers in our region, the risk of low birth weight was less in our region compared to Norway in general. Tobacco may cause significant risk to mother and child [31-36]. Preterm delivery rate is higher in the smoking group. New-borns of active smokers are more likely to weigh less, suffer from respiratory distress syndrome, from cardiac malformation and perinatal death [35]. Mitchell et al. [33] documented a correlation between tobacco smoking mothers and sudden intrauterine death syndrome (SIDS) of the infant. Assuming a causal association between smoking and SIDS, they argued that about one-third of SIDS deaths might have been prevented if no fetus was exposed to maternal smoking. Based on these risk factors, we were happy to reveal the falling trend of maternal smoking in our country. We revealed a not significant drop in infant death per 1,000 births from 4.3 to 3.7.Assuming one third of these deaths was due to maternal smoking and implementing a 50% reduction of maternal smokers, the infant death rate can be calculated to drop from 4.3 to 3.6 thousandth.
It is not easy to quit smoking. One alternative could be midwife supported tobacco cessation programs. In Poland, such programs have shown promising results [32]. We know that many pregnant women who stop smoking often turn to smokeless tobacco (ST). The most common alternative is the use of snuff tobacco. Recently, a review of maternal ST use in pregnancy and adverse health outcomes in newborns was published [35]. A total of nine studies were detected. Significant association with ST use were seen in 5/7 studies for low birth weight, in 3/6 studies for preterm, in all 4 studies for stillbirth and in ½ studies assessing small for gestation age. The authors conclude a need for quality observational studies to strengthen the evidence base. Unfortunately, we had no data on the use of snuff tobacco in our study.
We have shown the decentralized structure of the obstetric care in Northern Norway with 15 delivery units and a population of less than half a million inhabitants scattered within a large geographic area. During the last thirty years (1979-2009), the number of delivery institutions in Norway has declined from 95 to 51 [33]. Despite this centralization, Engjom and colleagues [37] did not reveal the expected decrease in maternal morbidity. However, the proportion of women living outside the 1-hour zone increased from 7.9% to 8.8% and the number of unplanned deliveries outside institutions increased from 0.4% in 1979-1983 to 0.7% in 2004-2009. During our study period, no reduction in the number of institutions occurred in Northern Norway, and the number of unplanned deliveries outside institutions stayed significantly higher in the northern region (0.8% vs. 0.7%). We argue that this is due to the mentioned characteristics concerning geography and population of Northern Norway. However, the figures indicate that caution should be taken when reductions in the number of institutions in Northern Norway are considered in the future.
Conclusion
The Northern Norway Regional Health Authority provides obstetric health care of good quality. Further work is required to investigate the reasons for an increasing and variable caesarean section rate between units and raising numbers of GDM. The documented decrease in caesarean surgical wound infection rate and maternal smoking habits are welcome. The possible effect of the common selection criteria in the long run should be followed up.
Competing Interests
The authors declare that they have no competing interests.
Authors’ Contribution
JN, TS and RS initiated the study and designed the protocol. JN, TS, IPO participated in the acquisition of data. Statistical analysis was done by JN and evaluated by MK. Suggested sub-analysis, interpretation of data and comments with regard to the results were given by all authors. All study participants have participated in the writing process of the manuscript and given their approval of the final version.
Acknowledgement
The authors are thankful to the Medical Birth Registry of Norway who offered data available online on their Website. We also acknowledge the support from the library at the UiT-The Arctic University of Norway and the access to necessary infrastructure at the Northern Norway Regional Health Authority trust. We are also grateful for comments given by Ingard Nilsen, the head of RCOG at the UNN, and the advisory board at the NNRHA trust.
References
- Nesheim BI, Eskild A, Gjessing L (2010) Does allocation of low risk parturient women to a separate maternity unit decrease the risk of emergency caesarean section? ActaObstetGynecol Scand. 89: 813-816.
- Holt J, Vold IN, Johansen MV, Oian P (2012) Child birth in a modified midwife managed unit: selection and transfer according to intended place of delivery. ActaObstetScand 80: 206-212.
- Ministry of Health and Care Services (2009) A happy occasion. A continuous maternity, delivery and postpartum care Oslo, Norway: Ministry of Health and Care Services. Stortinget 12: 2008-2009.
- Ministry of Health and Care Services (2009) The coordination reform. Correct treatment-at the right place-at the correct time. Oslo, Norway: Ministry of Health and Care Services. Stortinget 47: 2008-2029.
- Northern Norway Regional Health Authority trust (NNRHA) (2010) A regional plan for a comprehensive prenatal, birth and postnatal care in Northern Norway. Consequences of the proposed national quality standards. Bodø: Northern Norwegian Regional Health Authority trust.
- Norum J, Heyd A, Hjelseth B, Svee T, Murer FA, et al.(2013) Quality of obstetric care in sparsely populated sub-arctic area of Norway 2009-2011. BMC Pregnancy Childbirth.
- BenchimolEI, Smeeth L, Guttmann A, Harron K, Moher D, et al.(2015) Record Working Committee. The Reporting of studies Conducted using Oservational Routinely collected Health Data (RECORD) Statement. PLoS Med 12: 1001885.
- Bouvier-Colle MH, Mohangoo AD, Gissler M, Novak-Antolic Z, Vutuc C, et al.(2012) What about the mothers? An analysis of maternal mortality and morbidity in perinatal health surveillance systems in Europe. BJOG 119: 880-890.
- Norwegian Board of Health Supervision (2015) serious adverse events in hospitals-status and experience from the investigation unit for serious adverse events 2014. Oslo, Norway: Norwegian Board of Health Supervision.
- Norwegian Institute of Public Health (2012) Annual tables for medical birth registry 2010. Births in Norway. Oslo, Norway: Norwegian Institute of Public Health.
- Khunpradit S, Tavender S, Lumbiganon P, Laopaiboon M, Wasiak J, GruenRL (2011) Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database of Systematic Reviews 6: 5528.
- British Broadcasting Cooperation (BBC) (2011) Women can choose caesarean birth.
- Mohammade S, Källestål C, Essen B (2012) Clinical audits. A practical strategy for reducing caesarean section rates in a general hospital in Theran, Iran. J Reprod Med 57: 43-48.
- Eggesbø M, Mandal S, Midtvedt T (2015) Factors affecting gut microbiota and possible consequences for health. MicrobiolEcol Health Dis 26: 28062.
- Salam MT, Margolis HG, McConnell R, McGregor JA, Avol EL, et al. (2006) Mode of delivery is associated with asthma and allergy occurrences in children. Ann Epidemiol 16: 341-346.
- Eggesbø M, Botten G, Stigum H, Nafstad P, Magnus P (2003) Is delivery by caesarean section a risk factor for food allergy? J Allergy ClinImmunol 112: 420-426.
- Tollånes MC, Moster D, Daltveit AK, Irgens LM (2008) Caesarean section and risk of severe childhood asthma: A population-based cohort study. J Pediatr 153: 112-166.
- Skjeldestad FE, Øian P (2012) Blood loss after caesarean delivery. A registry based study in Norway 1999-2008. Am J ObstetGynecol 206: 7.
- Pu J, Zhao B, Wang EJ, Nimbal V, Osmundson S, Kunz L, et al.(2015) Racial/Ethnic Differences in Gestational Diabetes Prevalence and Contribution of Common Risk Factors. PaediatrPerinatEpidemiol 29: 436-439.
- Shao P, Zhang C, Tian H, Zhang F, Zhang S, et al. (2015) Prevalence of gestational diabetes mellitus and its risk factors in Chinese pregnant women: a prospective population-based study in Tianjin, China. PLoS One 10: 121029.
- Abouzeid M, Versace VL, Janus ED, Davey MA, Philpot B, et al. (2014) A population-based observational study of diabetes during pregnancy in Victoria, Australia, 1999-2008.
- Strøm H, Selmer R, Birkeland KI, Schirmer H, Berg TJ, et al. (2014) No increase in new users of blood glucose-lowering drugs in Norway 2006-2011: a nationwide prescription database study. BMC Public Health 29: 520.
- Barau G, RobillardPY, Hulsey TC, Dedecker F, Laffite A, et al.(2006) linear association between maternal pre-pregnancy body mass index and risk of caesarean section in term deliveries. BJOG 113: 1173-1177.
- Dietz PM, Callaghan WM, Sharma AJ (2009) High pregnancy weight gain and risk of excessive fetal growth. Am J ObstetGynecol 201: 1-6.
- Bowers K, Laughon SK, Kiely M, Brite J, Chen Z, et al. (2013) Gestational diabetes, pre-pregnancy obesity and pregnancy weight gain in relation to excess fetal growth: variations by race/ethnicity. Diabetologica 56: 1263-1271.
- McDonald R, Karahalios A, Le T, Said J (2015) A Retrospective Analysis of the Relationship between Ethnicity, Body Mass Index, and the Diagnosis of Gestational Diabetes in Women Attending an Australian Antenatal Clinic. Int J Endocrinol 297: 420.
- Yuen L, Wong VW (2015) Gestational diabetes mellitus: Challenges for different ethnic groups. World J Diabetes 6: 1024-1032.
- Statistics Norway (2015) Key figures concerning immmigrants and immigration. Oslo, Norway: Statistics Norway.
- Northern Norway Regional Health Authority trust (2013) From action to interaction 2014-2019, the regional plan for diabetes. A report from the regional diabetes council. Bodø, Norway: Northern Norway Regional Health Authority trust.
- Norwegian Directorate of Health (2009) National guidelines for diabetes. Prevention, diagnostics and treatment. Oslo, Norway: Norwegian Directorate of Health.
- Kandel DB, Griesler PC, Schaffran C (2009) Educational attainment and smoking among women: risk factors and consequences for offspring. Drug Alcohol Depend 104: 24-33.
- Polanska K, Hanke W (2006) Effectiveness of smoking cessation interventions for pregnant women-meta-analyses of randomized trials andf description of the study performed in Poland. Ginekol Pol 77: 422-428.
- Mitchell EA, Milerad J (2006) Smoking and the sudden infant death syndrome. Rev Environ Health 21: 81-103.
- Mei-Dan E, Walfisch A, Weisz B, Hallak M, Brown R, et al. (2015) The unborn smoker: association between smoking during pregnancy and adverse perinatal outcomes. J Perinat Med 43: 553-558.
- Inamdar AS, Croucher RE, Chokhandre MK, Mashyakhy MH, Marinho VC (2015) Maternal Smokeless Tobacco Use in Pregnancy and Adverse Health Outcomes in Newborns: A Systematic Review. Nicotine Tob Res 17: 1058-1066.
- Murin S, Rafii R, Bilello K (2011) Smoking and smoking cessation in pregnancy. Clin Chest Med 32: 75-91.
- Engjom HM, Morken NH, Norheim OF, Klungsøyra K (2014) Availability and access in modern obstetric care: a retrospective population-based study. BJOG 121: 290-239.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11740
- [From(publication date):
August-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10771
- PDF downloads : 969