The Lower Kinetic Injury Chain: A Musculoskeletal Biomechanical Perspective into Lower Extremity Injury and Modalities to Remediate them
Received: 25-Sep-2022 / Manuscript No. JPAR-22-77452 / Editor assigned: 27-Sep-2022 / PreQC No. JPAR-22-77452 / Reviewed: 10-Oct-2022 / QC No. JPAR-22-77452 / Revised: 17-Oct-2022 / Manuscript No. JPAR-22-77452 / Published Date: 24-Oct-2022 DOI: 10.4172/2167-0846.1000465 QI No. / JPAR-22-77452
Abstract
The aim of this article is to highlight the importance of interventions for successful recovery from an injury sustained in the lower kinetic chain. The article is intended to give a background and understanding to the general population, working professionals, athletes, military personnel, first responders or anyone that has experienced pain and discomfort from a lower extremity injury about the biomechanical intricacies of the lower extremity and how injury affects each component. The kinetic chain is a musculoskeletal biomechanical theory on how the lower extremity moves within itself to produce movement such as walking, running, standing and sitting. Within these movements, each component of the kinetic chain has an effect on each component which surrounds the joint. When injury occurs in the musculoskeletal system there is a cumulative injury cycle effect throughout the kinetic chain. The cumulative cycle affects the skeletal, muscular, and articular systems and will impair move In summary, the cumulative injury cycle can impede function and lower kinetic chain performance. During and after an injury, it is important to remain active and mobile as much as possible. Interventions such as osteopathic/myofacial manual therapy treatment and corrective exercises are good modalities to use to help alleviate pain (both chronic and acute), but also to reduce the effects of the lower extremity kinetic chain from becoming stuck in the inflammatory or proliferative phase of healing. Being stuck in one of the 2 phases of the injury cycle contributes to the cumulative injury of the area that is being injured and causes prolonged recovery. In addition, stretching and self-myofacial release (SMR) can benefit a person in maintaining flexibility within the human movement system. A duration of as little as 10 minutes devoted to SMR (up to a minute on each extremity, the back and chest) can increase flexibility, decrease accumulation of adhesions formed on muscle fibers and prevent stiffness and changes in muscle fiber (degenerative changes) caused from sedentary lifestyle. Both OMT/MMR and corrective exercise treatment are underutilized in majority of outpatient clinics and therefore needs to be strongly emphasized for all practitioners to learn, especially if the goal of the practitioner is to decrease pain/discomfort and to increase functional mobility within their patient populations. Mobility and proper conditioning of the musculoskeletal system equates kinetic chain functionality and good health throughout the extremity in the lower extremity. Treatment modalities need to focus on the specific area of injury. The modalities can be in the form of stretching, manual osteopathic treatment (OMT)/ Manual myofacial release (MMR), therapeutic/corrective exercise programming. Research supports eccentric exercises effectiveness in helping retrain the body back into conditioning for sports or every-day-functionality. These treatment modalities have the greatest effect on correcting and stopping the cumulative injury cycle in the lower kinetic chain.
Keywords: Central nervous system; Body movement; Kinetic Chain; Injury; Inhibition; Myofacial release
Keywords
Central nervous system; Body movement; Kinetic Chain; Injury; Inhibition; Myofacial release
Introduction
The musculoskeletal system is made up of multiple components that are interconnected with one another. These components are seen as parts that make up the human movement system. The key integrated systems that make up the human movement system are: central nervous system (brain and spinal cord), the skeletal muscular system and the articular system (ligaments, joints, & capsules). These systems coordinate with each other to give a person optimal movement performance. Another name of the human movement system is known as the kinetic chain. The kinetic chain system is reliant on optimal length tension relations and neuromuscular efficiency between each of these respected systems. The human movement as a whole is made up of two major parts; upper and lower kinetic chains. The upper kinetic chain is made up of the upper extremities; hand/wrist, elbow and shoulder as well as the cervical and thoracic spine. The lower kinetic chain is made of the joints of the lumbar spine, sacroiliac joints, hips, knee, and ankle and foot joints. Each joint in the lower kinetic chain is surrounded with muscles and tendons which work as levers and forces producing systems to move the joints and bones through space which constitutes body movement. During movement (i.e., gait, running, climbing stairs etc.) each joint of the lower extremity is connected to another joint both proximally and distally through muscular and ligament connections. As muscles contract and extend during active motion each joint of the kinetic chain needs to perform joint motions such as sliding, gliding, compressing and distraction. The muscles within the lower kinetic chain provide propulsion moments during gait or running. During injury, both muscles and the joints become impaired and motion is not fully executed or is not biomechanically aligned to perform the motion properly without pain. It is important to recognize the injury cycle, its causes, and treatment modalities to ensure proper motion is always maintained in order to reduce massive energy expenditure and decrease inflammatory processes within the somatic kinetic chain movement system.
During an injury, the component that is affected (i.e., the knee joint) will significantly impair movement within the other components in the lower kinetic chain. The injury causes trauma to the tissue surrounding the knee joint (i.e. the vastus medial oblique (VMO), the quadriceps tendon, collateral ligaments etc...) and inflammation will surround the tissues. This will cause the tissues (i.e., muscles, tendons) around the area to go into spasm creating pain and decrease in proper function of concentric knee extension and eccentric knee flexion during normal gait. During the healing process, the inflammation is the first process of the cumulative injury cycle and last from 24 hours to 7 days [1]. The injured area is bombarded with neutrophils and macrophages that predominately prevent infection and clean up debris from dead cells and small bacteria traces. After the inflammation phase, the proliferation phase begins. In this phase scar tissue is laid down to repair the injury in the muscle [2]. The last phase of inflammation is the remolding or maturation stage. In this stage, the scar tissue is remolded into permanent scar tissue (type 3). The scar tissue does not replace the ease of motion as the original anatomical muscle tissue. As a result, the scar tissue does not allow ease of normal sliding within the fascia. This lack of ease of the sliding motion will cause the scar tissue to get “stuck” like a fly on flypaper. The “stuck” scar tissue is known as an adhesion. These adhesions disturb the natural sliding filaments of the actin and myosin fibers and prevent proper contraction to take place. Knots of non-mobile bounded up muscle fibers also can become "stuck" to each other like glue; these become another type of adhesion. When the adhesions are settled in the muscle; optimal movement is prevented. The formation of the adhesions will cause tightness in the muscle causing the normal length tension relationship within the lower kinetic chain to be imbalanced and cause dysfunction. This is known as the cumulative injury cycle. This concept is considered a cycle because this phenomenon can continue over and over again creating movement compensations. Muscle imbalances are formed because of the adhesions in the muscle and the increased formation of scar tissue on the fascia covering the muscles bellies [3]. The fascia surrounds the muscle and allows sliding of tendons and adjoining muscles bellies to slide/glide over one another
In the knee joint, the muscles around the joint create the motion. Some muscles around the knee joint can create tightness on the lateral side of a joint (i.e., vastus lateralis and IT-band) and weakness or lengthening of muscles (i.e., VMO) on the medial side of the joint. As for the example of the injury to the knee joint, the muscular imbalance is caused by tightness of the vastus lateralis in relation to the other muscles in the lower kinetic chain. Muscles in the lower kinetic chain such as the VMO, anterior and posterior tibialis, medial gastrocnemiussoleus and medial hamstrings become weak and lengthened. These altered length tension relationships will cause altered neuromuscular movement and reduced optimal performance [4]. The muscular imbalances will decrease neural drive from the central nervous system into the main muscle group and increase neural drive into the opposing muscle groups causing reciprocal inhibition. Reciprocal inhibition is caused by altered neural drive into the antagonist instead of going to the primary agonist (quadriceps) muscle. The area of muscular imbalance (the agonist with the adhesions that are formed in it) will not activate properly. This muscular imbalance will cause the increase in the neural drive to the antagonist creating compensations in movement during walking, squatting and other functional movements [5]. This is the biomechanical effect on the muscular system of the lower kinetic chain the cumulative injury cycle has on overall movement.
This cycle will continue until proper intervention of modalities such as osteopathic manual treatment or corrective exercise is presented to the lower kinetic chain dysfunction [6]. Without effective interventions of this nature, such as osteopathic manual treatment (OMT)/ Manual myofacial release (MMR) and/or corrective exercise, the cumulative injury cycle will continue to contribute to dysfunctional movement compensations (Figure 1). This will cause a decrease in movement efficiency and simultaneously increase the risk and frequency of future injuries to other areas of the kinetic chain as a result of this muscular imbalance. Some examples of stretching, exercise programming and manual interventions and their benefits are described below
Manual Myofacial Release treatment application
Osteopathic or manual myofacial release treatment can be of great help with musculoskeletal pain and dysfunction in the lower extremity (Figure 2). Osteopathic manual treatment (OMT) or Manual myofacial release (MMR) are hands-on modalities that are performed by trained manual physiotherapists, chiropractors, athletic trainers, podiatrists, naprapathy and manual osteopathic doctors [7]. The most popular application of both MMR and OMT are used to alleviate pain/discomfort and somatic dysfunction of the lower kinetic chain [8]. OMT/MMR has been used for assessment of dysfunctional soft tissue around different joints of the lower extremity. Joint pathologies in joints such as knees, and ankle/foot can be detected by careful palpation of the soft tissue and muscles around the joint. A skilled osteopathic practitioner can use OMT/MMR techniques to detect dysfunction in joints along the kinetic chain during a general passive range of motion lower extremity assessment to detect the origin of problems or of chronic pain when the patient presents with chronic pain from walking, stair climbing, getting out of a car or climbing in or out of bed. These joint dysfunctions may not be apparent until a gross assessment of kinetic chain of the lower extremity is done. As an example, if a patient is complaining of foot pain during ambulation, a skilled manual practitioner may discover through palpation proximal joint pathology could be the real root cause of the problem; the knee and/or hip joint is restricted through a normal range of motion. These proximal joint pathologies can be contributing to abnormal gait which is having secondary or tertiary effects on the foot which is causing pain to the patient. According to the article by Cholewicki et. al 2021; The use of OMT on a group of patients suffering from non-specific neck pain originating from somatic dysfunction was successful (Figure 3(a)). The patients in this study aged 21-65 years old received 2-4 OMT sessions spanning 4-6 weeks of treatment showed improvements in pain using a numeric rating system (aka the visual analog scale (VAS)) and a decrease in dysfunction of the region of the original symptoms [9].
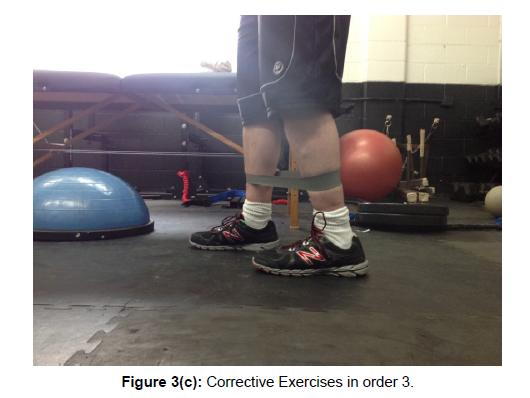
For muscles and tendons such as the quadriceps, hamstrings, gastrocnemius-soleus complex, osteopathic/myofacial release manipulation can be applied to restore lost motion from an injured, dysfunctional joint. For example, during runner’s knee/ IT- band syndrome; the muscle/tendon of the Iliotibial band is usually injured. During the inflammatory and proliferation stage of the injury the muscle becomes inflamed and then scar formation occurs. When the scar tissue gets applied to the tendon, the added tissue bounds down the tendon and does not allow it to glide smoothly over the fascia bands surrounding the tissue. As a result, during motion of the knee of flexion and extension, the tendon will get caught and the muscle will go into the spasm causing pain. Using OMT/MMR, the practitioner can use both the indirect and direct supine knee flexion and extension muscle energy technique to alleviate the pain and restore active range of motion to the knee joint (Figure 3(b)). The practitioner can start with several sessions directed at the quadriceps and then the hamstrings. Each session focusing on increasing more range of motion to the knee until full range of motion without pain is restored. Common knee pathology is osteoarthritis or degenerative joint disease (DJD). In this pathology, the joint space of the femoral tibia joint becomes narrowed. This is due to the reduction of height of the meniscus within the knee joint or the meniscus has been worn down to the point that both of the articular joint surfaces of both the tibia and femur are now in close approximation or they are in direct contact with each other [9]. During full extension of the knee, the compression force causes pain on the articular surfaces of the both the tibia and femur bones. Sometimes the constant grinding and compression of both of these will contribute to formation of osteophytes which will make the pain worse during the weight-bearing. The OMT/MMR technique to use for DJD is the long axis traction technique (Figure 3(c)). The practitioner would flex the knee from 5-10 degrees, then stabilize the proximal portion of the joint, distract the distal end(tibia). This will alleviate the compression and gap the joint to decompress the compressed, inflamed articular surfaces of the both the femur and tibia bones [10].
Another common pathology is Achilles’ tendonitis. Achilles’ tendonitis is caused by overuse of the muscles of the lower leg. The muscles that make up the Achilles’ tendon are the gastrocnemius, the solus and the plantaris. There are 2 main sources that contribute to Achilles’ tendonitis. There are intrinsic factors which include foot deformities, muscular imbalances between anterior and posterior muscle groups of the lower leg, ankle instability. Extrinsic factors affecting Achilles’ tendonitis include, mechanical overload, ineffective shoes, obesity, or insufficient stretching. The application of osteopathic manual treatment can be used on the gastrocnemius such as the supine gastrocnemius and soleus release. Manual posterior joint mobilization on the talus which would promote more dorsiflexion at the joint could also alleviate dysfunction at the joint and allow more range of motion and lengthening of the Achilles’ tendon [11].
Corrective Exercise Intervention
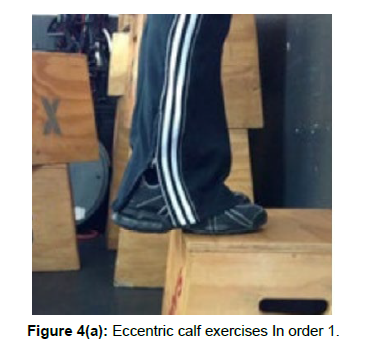
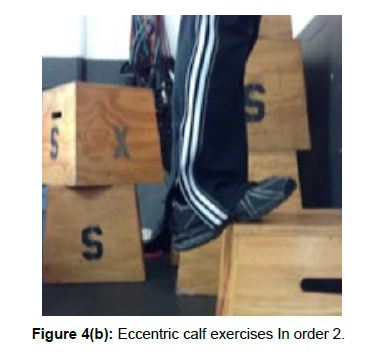
A corrective exercise intervention is used to prevent adhesions from forming on muscles. Static stretching is an example of an effective corrective exercise intervention. Stretching promotes flexibility within muscles and increases range of motion (ROM) within the joints. Two kinds of stretching are static stretching and self-myofacial release (SMR) (Figure 4(a)). Static stretching can be performed my holding either the distal or proximal portion of the tendon attachment to the bone and move the opposite component away from starting position (i.e.: to stretch the quadriceps muscles; stand erect and hold on to a wall; grab the foot of the side of the quads you wish to stretch, flex the knee and bring the foot behind you towards the buttocks area). According to research, holding a static stretch for 30 seconds is the appropriate time to cause deformation of the stiffness of the muscle to gain an adequate stretching effect. Other types of stretching are active and dynamic stretching. Active stretching refers to stretching a joint and/or muscles around the joint to its limits of range of motion. Active stretching involves activating the agonist muscle to stretch the antagonist (i.e., stretching the triceps by performing elbow flexion using the biceps muscle: the biceps is the agonist and the triceps are the antagonist) [12]. Active stretching usually targets muscles that are either single or multiple joints in function (i.e., soleus vs. rectus femoris) (Figure 4(b)). Dynamic stretching refers to an activity that brings the joint to its limits of range of motion but can be used as an exercise (i.e., a lunge or shackles walks).
Another form of stretching is known as self-myofacial release. Using a foam roller is one of the common methods to perform selfmyofacial release. Myofacial release is performed by using one's own body weight and gravity to induce an ischemic pressure over an extremity or portion of the body to "release" a tight muscle fibre.
According to research, MacDonald et al, 2013; a bout of self-myofacial release for approximately 2 minutes in duration decreased pain and increased the range of motion of the knee joint by releasing the muscles of the quadriceps group that were tight and restricting normal ROM [13]. The duration of performing SMR varies depending on the size and length of the extremity being rolled. However, it is important that the foam rolling needs to be performed correctly and in conjunction with an exercise program. To perform foam rolling correctly, first assume a position in which the foam roller is under the extremity (i.e., thigh) and the roller is positioned superiorly or inferiorly to the muscles to be rolled. It is important that the person takes their time and slowly rolls over the entire area to be stretched. When a tender spot is identified, the person should stop and allow the ischemic pressure to commence for 10-20 seconds over the tender spot. The tender spots that are encountered in the muscles are the adhesions that have formed from past injuries (results from the cumulative injury cycle or from sedentary practices which results in muscles becoming tight). It is important that when performing SMR, each tender spot is identified and treated using the foam roller and body weight. According to research, the total duration of foam rolling for the upper portion of the lower extremity (thigh muscles) was approximately 1 minute [14]. This includes the 10- 20 second pauses over the tender areas within the muscle belly.
Some corrective exercises to address the strengthening of the tendons of the lower extremity including the Achilles tendon revolve around eccentric exercises. According to research, there have been many positive and effective articles around the use of eccentric exercises to repair damaged muscles caused from overuse and prolonged inflammatory staged injuries. Eccentric exercises are performed by loading the muscle or tendon with an appropriate weight (i.e., 10% of 1 rep max of the muscle group). When the muscle or tendon is loaded, the exercise starts at the concentric point (most shortened) of the muscle length. The exercise is focused on the lengthening portion of the range. With the tendon loaded and is allowed to move through the lengthening portion of the range, the fibres of the muscle/tendon will become stronger as the fibres become denser. This strengthening will help alleviate pain, but also help to build endurance against future injuries. The use of eccentric exercises will help the lower kinetic chain absorb forces from outside the kinetic chain (i.e. ground reaction forces) and help control internal forces during activities such as jumping, descending stairs, or decelerating the body during sports or running events. During descending stairs, the body decelerates joint motion of the hip, knee, and ankle to allow more absorption of forces through the musculoskeletal system. This will reduce increased friction on the joints, saving the articular joint surface from breaking down the joint. The biomechanical mechanism within an eccentric exercise has an elastic recoil energy component and contributes to the coupling phases of the stretch-shortening cycle. This component of stretch-shortening cycle has real world applications which includes recovery from injury due to everyday motions and human body movement and includes sports as eccentric shortening and lengthening occurs constantly at a high rate of speed and frequency [15].
Conclusion
In summary, the cumulative injury cycle can impede function and lower kinetic chain performance. During and after an injury, it is important to remain active and mobile as much as possible. Interventions such as osteopathic/myofacial manual therapy treatment and corrective exercises are good modalities to use to help alleviate pain (both chronic and acute), but also to reduce the effects of the lower extremity kinetic chain from becoming stuck in the inflammatory or proliferative phase of healing. Being stuck in one of the 2 phases of the injury cycle contributes to the cumulative injury of the area that is being injured and causes prolonged recovery. In addition, stretching and self-myofacial release (SMR) can benefit a person in maintaining flexibility within the human movement system. A duration of as little as 10 minutes devoted to SMR (up to a minute on each extremity, the back and chest) can increase flexibility, decrease accumulation of adhesions formed on muscle fibres and prevent stiffness and changes in muscle fibre (degenerative changes) caused from sedentary lifestyle. Both OMT/MMR and corrective exercise treatment are underutilized in majority of outpatient clinics and therefore needs to be strongly emphasized for all practitioners to learn, especially if the goal of the practitioner is to decrease pain/discomfort and to increase functional mobility within their patient populations. Mobility and proper conditioning of the musculoskeletal system equates kinetic chain functionality and good health throughout the lower extremity.
References
- Clark MA, Lucett SL (2011) NASM Essentials of Corrective Exercise Training. LWW 1st Edn US 9: 1-14.
- Sands W, McNeal JR, Murray SR, Ramsey MW, Sato K, et al. (2013) Stretching and Its Effects on Recovery: A Review. J Strength Cond Res US 35: 30-36.
- MacDonald GZ, Penney MDH, Mullaley ME, Cuconato AL, Drake CDJ, et al. (2013) An Acute Bout of Self-Myofascial Release Increases Range of Motion without a Subsequent Decrease in Muscle Activation or Force. J Strength Cond Res US 27: 812-821.
- Okamoto T, Masuhara M, Ikuta K (2014) Acute effects of self-myofascial release using a foam roller on arterial function. J Strength Cond Res. US 28: 69–73.
- Mishra A, Woodall J, Vieira A (2009) Treatment of Tendon and Muscle Using Platelet-Rich Plasma. Clin Sports Med 28: 113-125.
- Tramontano M, Tamburella F, Dal Farra F (2021) International Overview of Somatic Dysfunction Assessment and Treatment in Osteopathic Research: A Scoping Review Healthcare EU 10: 1-28.
- Medina Pabón MA, Naqvi U (2022) Achilles Tendonitis. Stat Pearls Treasure Island FL 30: 76-84.
- Kanniappan V, Sathosh AM (2020) To Compare the Effect of Eccentric Exercises and Isometric Exercises for Achilles Tendinitis in Skaters. J Lifestyle Med US 10: 49-54.
- Harris-Love MO, Gollie JM, Keogh JWL (2021) Eccentric Exercise: Adaptations and Applications for Health and Performance. J Funct Morphol Kinesiol EU 6: 90-96.
- Bagagiolo D, Rosa D, Borrelli F (2022) Efficacy and safety of osteopathic manipulative treatment: an overview of systematic reviews. BMJ Open UK 12: 1-15.
- Cholewicki J, Popovich Jr JM, Reeves NP (2022) The effects of osteopathic manipulative treatment on pain and disability in patients with chronic neck pain: A single‐blinded randomized controlled trial. PM&R UK 31: 1-27.
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
IndexedAt , Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Citation: Chittenden K (2022) The Lower Kinetic Injury Chain: A Musculoskeletal Biomechanical Perspective into Lower Extremity Injury and Modalities to Remediate them. J Pain Relief 11: 465. DOI: 10.4172/2167-0846.1000465
Copyright: © 2022 Chittenden K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4696
- [From(publication date): 0-2022 - Nov 27, 2025]
- Breakdown by view type
- HTML page views: 4110
- PDF downloads: 586