The Influence of Mode of Delivery on the Neurodevelopment of Children and Adolescents
Received: 02-May-2018 / Accepted Date: 23-May-2018 / Published Date: 30-May-2018 DOI: 10.4172/2376-127X.1000378
Abstract
Background: Cesarean section is one of the most frequently performed surgical procedures in the world and its rates have been increasing worldwide over the past decades. Despite being a lifesaving procedure in emergent situations, it can be associated with a range of adverse maternal and childhood health outcomes. To date, there is a lack of consistent studies regarding the association between mode of delivery and a child’s neurodevelopment.
Objective: The aim of this review is to highlight the possibility of neurocognitive outcomes during childhood and adolescence being affected by the child’s mode of delivery.
Method: Literature review based on studies published between 2005 and 2018, available on PubMed.
Results: Regarding uncomplicated pregnancies and deliveries most studies found no difference in neurodevelopment according to mode of delivery, apart from nonplanned cesarean, which usually correlates to worse outcomes. In breech presentation, shortterm outcomes of children born vaginally were poorer while long-term neurological outcomes were contradictory. Preterm infants were more commonly associated with adverse neurological outcomes and these varied according to the age at which children were assessed. Considering drug administration during delivery, the long-term neurological effects of children exposed to exogenous oxytocin are not known and transitory neonatal exposure to anaesthetic drugs during delivery probably won’t harmfully influence longterm neurodevelopment.
Conclusions: Neurodevelopment is influenced by a vast number of genetic and environmental variables, becoming impracticable to account for all factors that may affect neurocognitive outcomes. Therefore, future investigation is necessary to enlighten if neurodevelopment is in fact associated with mode of delivery or if underlying causes are the real influencers. Thus, when considering mode of delivery, every obstetrical case should be individually analysed, maternal and neonatal risks and benefits should be balanced and common beliefs demystified to help mothers make an informed decision and promote their children’s healthy development.
Keywords: Vaginal delivery; Cesarean section; Neurodevelopmental outcomes; Children; Breech presentation; Preterm
Abbreviations
CS: Cesarean Section; IQ: Intelligence Quotient; VD: Vaginal Delivery
Introduction
Cesarean section is one of the most frequently performed surgical procedures in the world, representing the most executed major obstetrical intervention, with rates varying between 5-60% [1]. Some situations constitute absolute indications for cesarean section, such as placenta praevia, truly obstructed labour from a contracted pelvis or significant fetal macrosomia. Relative indications for this procedure are those where it is considered that the risk of a vaginal birth exceeds the risk of cesarean [2]. Therefore, cesarean section can be a lifesaving procedure in emergent situations, being responsible for the decrease in mother and child mortality during childbirth. According to the World Health Organization, the ideal rate for cesarean sections worldwide, justified from a medical perspective, would be around 10-15% [3].
Over the last decades there has been a global rise in the rate of cesarean section, which is believed to have as major contributors the increase in maternal request and changes in clinical practice [4- 6]. Furthermore, rates well above the World Health Organization’s recommended 15% ceiling suggest a high number of unnecessary procedures [7].
Since a cesarean section constitutes a surgical procedure, it can be associated with a range of adverse maternal and childhood health outcomes [8,9]. Some relations between cesarean birth and adverse child health outcomes have already been established, such as asthma, type 1 diabetes, allergies and obesity [10-13].
Contrarily, there is a lack of consistent studies regarding the association between mode of delivery and a child’s neurodevelopment, particularly referring to cognitive development, such as intelligence and learning abilities. Despite the shortage of evidence on this subject, it is a common opinion that a child’s cognitive function is negatively affected by the pressure of passing through the birth canal during vaginal delivery and this constitutes one of the main reasons in developing societies for the increase of cesarean delivery on maternal request [5,6]. Additionally, some modes of delivery, such as instrumental vaginal delivery (forceps or vacuum) and cesarean delivery in labour, are invariably related to a higher risk of intracranial injury, however data regarding long-term neurological outcome of children born by these procedures is sparse [14,15].
An extremely important aspect to account for when assessing a child’s neurodevelopmental outcome according to mode of delivery is fetal presentation. Breech presentation at term occurs in 2-3% of all singleton pregnancies and according to the Term Breech Trial a planned vaginal birth of a breech baby was associated with significantly increased perinatal or neonatal mortality or serious neonatal morbidity in comparison with planed cesarean section [16-19]. However, this trial also stated that no differences in neurodevelopment in children at 2 years of age could be verified according to planned mode of delivery [20]. Therefore, mode of delivery in breech infants may influence short and long-term outcomes, such as cognitive development, but there have been few studies on the subject and their results are unclear [21-23].
Likewise, premature birth exerts a significant influence in neurodevelopmental outcomes of children, mainly since fetal brain development suffers a rapid acceleration as of 32 weeks of gestation, making it vulnerable to disturbance in a shortened pregnancy [24,25]. Accounting for these infant’s patent fragility, it’s of utmost importance to consider how mode of delivery might further affect their neurodevelopment, but data is limited regarding these outcomes [26]. Even though there is no consensus regarding optimal mode of delivery, the rate of cesarean section exceeds that of vaginal delivery in this group of infants, mainly because it is believed that cesarean will allow for a less traumatic birth [27].
Furthermore, human neurodevelopment is particularly vulnerable to pharmacological and environmental agents between the third trimester of pregnancy and up to 3-4 years of age [28,29]. Therefore, given the evolution of obstetrical interventions and consequent increase in drug administration during delivery, it becomes of extreme relevance to consider the effects of the latest on children’s long-term neurological outcomes. For instance, use of oxytocin is currently one of the most common medical practices in obstetrics and it’s included in the recommendations of the World Health Organization for labour induction [30,31]. However, some studies have suggested that excess in circulating oxytocin may cross the placental barrier and reach the neonate’s brain through the bloodstream, desensitizing their oxytocin receptors and producing adverse effects [32,33]. Regarding anaesthetics and analgesics, numerous studies have shown that neonates may be briefly affected by their usage during labour and delivery, nevertheless the long-term effects of these drugs in children’s neurodevelopment is not well established [34,35].
In short, a child’s neurodevelopment is a key outcome that needs to be accounted for when assessing mode of delivery, even though it can be influenced by several other variables. To date, studies conducted in this area have shown inconsistent results and may be unrepresentative of the general population.
Objectives
The aim of this literature review is to highlight neurodevelopment/ cognitive performance during childhood and adolescence while assessing the possibility of it being affected by the child’s mode of delivery. To this end, outcomes of vaginal delivery and cesarean section will be analysed regarding neurodevelopment, concurrently considering possible influencing factors such as emergency delivery, instrumental birth, breech delivery, premature birth and effects of drugs administered during labour and delivery.
Methods
Search strategy
The online platform used for this review was PubMed, resorting to the following search phrases: Mode of delivery/Type of delivery/ Cesarean/Vaginal delivery/Dystocia birth/Eutocia birth/Forceps and child development, Mode of delivery/Type of delivery/Cesarean/ Vaginal delivery and cognitive performance, Mode of delivery and learning disabilities, Mode of delivery/Type of delivery/Cesarean/ Vaginal delivery/Dystocia birth and neurodevelopment and MeSH word formula: (“delivery, obstetric”[MeSH Terms] OR “parturition”[MeSH Terms] OR “dystocia”[MeSH Terms] OR “surgical instruments”[MeSH Terms] OR “cesarean section”[MeSH Terms] OR “vagina”[MeSH Terms] OR “extraction, obstetrical”[MeSH Terms] OR “vacuum extraction, obstetrical”[MeSH Terms] OR “obstetrical forceps”[MeSH Terms]) AND (“infant”[MeSH Terms] OR “child”[MeSH Terms] OR “adolescent”[MeSH Terms]) AND (“cognition”[MeSH Terms] OR “intelligence”[MeSH Terms] OR “learning disorders”[MeSH Terms] OR “child development”[MeSH Terms] OR “adolescent development”[MeSH Terms]).
Inclusion criteria
In this review were eligible for inclusion case reports, case control studies and cohort studies, written in English or Portuguese that dated between 2005 and 2018, regarding neurocognitive development and mode of delivery, in study populations under 19 years of age.
Exclusion criteria
For this review were excluded review articles and all studies regarding: Behavioural disorders, autism spectrum disorders, children born from artificial insemination, effects of drug usage during pregnancy, twin pregnancy.
Article selection
20 original studies were chosen and analysed in this review and their main characteristics are summarized in (Table 1). Particularly, it should be noted that at some point during the execution of each of the aforementioned studies, a statistic analysis was performed to adjust for potential confounding factors. Commonly included covariates in these studies were: Maternal age at birth, parity, parental education, maternal occupation and employment, socioeconomic position (parental income), smoking habits during pregnancy, complications during pregnancy or labour, birth order, gestational age at birth, gender, birthweight, small for gestational age, 5 min Apgar score (Table 1).
| Study | Design | Sample size | Population focus | Quality score (adjustment for confounding variables?) | Outcomes measured |
|---|---|---|---|---|---|
| Smithers, 2016 [2] | Case-control | N=3609 | Previous cesarean | Yes | School achievement |
| Khadem, 2010 [5] | 1st stage: cross-sectional 2nd stage: case-control |
1st stage: N=5000 2nd stage: N=378 |
Uncomplicated pregnancies and deliveries | Yes (2nd stage) | IQ |
| Li, 2011 [6] | Cohort | N=4144 | Primiparous women | Yes | IQ |
| Robson, 2015 [8] | Cohort | N=4865 | Uncomplicated pregnancies and deliveries | Yes | General development |
| Bahl, 2007 [15] | Cohort | N=263 | Operative delivery | Yes | Neurodevelopment at 5 years of age |
| Eide, 2005 [21] | Cross-sectional | N=393570 | Breech presentation | Yes | Intellectual performance |
| Mackay, 2015 [22] | Cross-sectional | N=456947 | Breech presentation | Yes | Apgar score Level of educational attainment |
| Macharey, 2018 [23] | Cohort | N=8374 | Breech presentation | Yes | Adverse neurodevelopment at 4 years of age |
| González-Valenzuela, 2014 [30] | Cohort | N=400 | Oxytocin during delivery | Yes | Battelle Developmental Inventory scores |
| Sprung, 2009 [34] | Cohort | N=5320 | Anaesthesia during delivery | Yes | Learning disabilities |
| Flick, 2011 [35] | Cohort | N=5718 | Anaesthesia during delivery | Yes | Learning disabilities |
| Ahlberg, 2014 [36] | Cohort | N=126032 | Vacuum extraction delivery | Yes | Mean grade point average Mean score on national mathematics test |
| Polidano, 2017 [37] | Cohort | N=3666 | Uncomplicated pregnancies and deliveries | Yes | Cognitive development |
| Black, 2016 [38] | Cohort | N=40145 | Previous cesarean | Yes | Obesity at age 5 Hospitalization with asthma Learning disability Cerebral palsy Death |
| Molkenboer, 2006 [39] | Case-control | N=183 | Breech presentation | Yes | Abnormal development with the Ages and Stages Questionnaire |
| Obican, 2015 [42] | Cohort | N=158 | Preterm infants | Yes | Mental and Psychomotor Bayley II scores at 2 years of age |
| Kimura, 2017 [43] | Cohort | N=2138 | Preterm infants | Yes | Death before 3 years Neurodevelopmental impairment at 3 years |
| Bentley, 2016 [45] | Cohort | N=153730 | Preterm infants | Yes | Developmental high risk |
| Minguez-Milio, 2011 [47] | Cohort | N=138 | Extremely low birth weight infants | Yes | Survival and short-term morbidity Long-term neurocognitive and motor development |
| Zhu, 2014 [48] | Case-control | N=710 | Very low birth weight infants | Yes | Neonatal mortality Medical conditions Neurodevelopment |
Table 1: Studies analysed in the literary review.
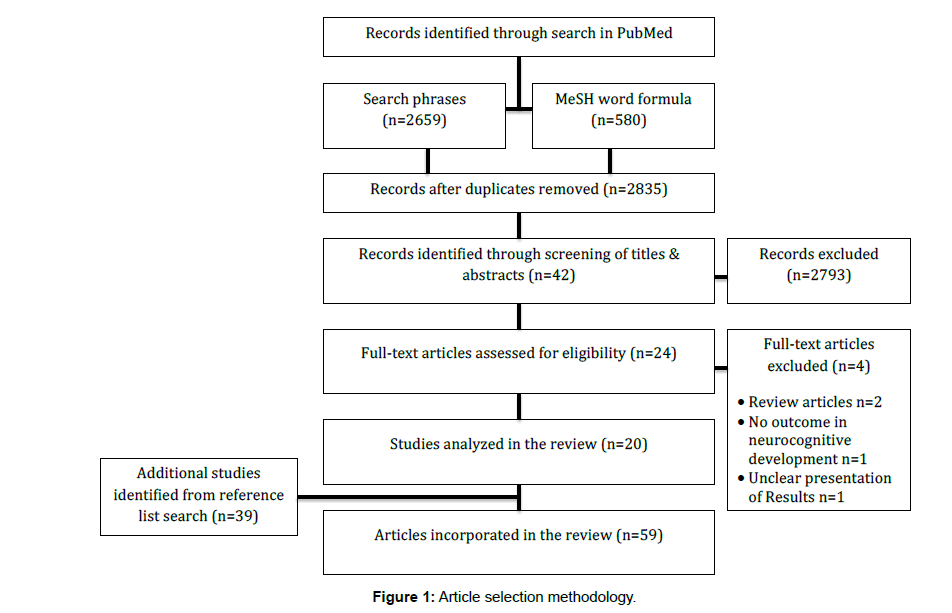
Furthermore, bibliographic references of the selected studies were also considered and incorporated in this review when found relevant. The schematics of article selection are shown in Figure 1.
Results
Vaginal delivery vs cesarean section
Regarding maternal and child characteristics, some studies revealed an association between the latest and mode of delivery. For instance, Li et al. observed that the mothers of children born by elective CS were older, had a higher education level and higher IQ [6]. The findings of Smithers et al. were in accordance, adding that these mothers were more likely to have a private obstetrician, more antenatal visits, be living in more advantaged areas and less likely to smoke during pregnancy [2]. Additionally, both studies stated that children born by elective cesarean were less likely to suffer from intrapartum fetal distress, having higher five-minute Apgar scores [2,6]. Contradicting these results, a study executed in an Australian cohort found that mothers who underwent CS were more likely to have a low socioeconomic position and the children born by cesarean delivery were more commonly preterm, low birth weight and more likely to require post-delivery intensive care [8]. Concerning vaginal birth, a study by Ahlberg et al. showed that women whose children were delivered by vacuum extraction were more likely to be older, have a higher education and a higher household income than those who gave birth without instruments [36].
Comparing neurocognitive development/learning abilities of children born by VD (spontaneous or instrumental) or CS, at term, after uncomplicated pregnancies, both Khadem et al. and Li et al. reported that in the crude analysis, children born by elective cesarean had a higher IQ than those born by vaginal delivery. However, when adjusted for confounding factors, particularly parental education, the difference became statistically insignificant [5,6]. Furthermore, Polidano et al. stated that child cognitive outcomes are positively associated with mothers that are college educated, are older when giving birth, have a partner, have private health insurance, are employed and have fewer previous births but no relation was found between cesarean birth and several cognitive outcomes measured from ages 4 to 9 in an Australian cohort, after adjusting for the socioeconomic advantage associated with cesarean birth in Australia and perinatal risk factors [37]. Ahlberg et al. assessed school performance in adolescents aged 15-16 years using 2 outcome variables: Mean grade point average and mean score on national mathematics tests. In both cases, after the adjustment for covariables, children born by noninstrumental delivery had higher scores compared to all other modes of delivery, particularly vacuum extraction delivery and nonplanned CS, which had the lowest scores [36].
A study performed by Bahl et al. focused simply on the neurodevelopmental outcomes of children whose mothers had term singleton cephalic pregnancies and required operative delivery at full dilation. The cohort was subdivided into 3 groups: Completed instrumental VD, failed instrumental VD followed by cesarean and immediate cesarean delivery. Children outcomes were evaluated through the caregiver completion of adapted questionnaires and there were no significant differences in reported neurodevelopmental concerns among the 3 groups at 5 years of age [15].
Considering obstetrical history, a child’s neurological outcome may differ according to their mother’s previous mode of delivery (CS or VD). Regarding learning disabilities, Smithers et al. and Black et al. found no significant differences when comparing planned repeat CS and spontaneous vaginal birth after CS, after adjusting for confounding variables [2,38]. However, learning disability was found to be more common when the child was born by unscheduled repeat CS, in comparison to spontaneous vaginal birth after CS [38].
Impact of breech presentation
A study conducted by Molkenboer et al. aimed to analyse whether the planned mode of delivery in breech presentation had an impact on neurodevelopmental outcomes [39]. To this effect, child development was assessed based on Ages and Stages Questionnaire (ASQ), containing 5 domains and in the group of children with 1 or more abnormal domains, the difference in percentage of children born by planned CS and planned VD was statistically insignificant when their birth weight was under 3500 g [40]. However, in children with birth weights greater than 3500 g, the risk of having 1 or more abnormal domains was higher in the planned VD group [39].
To the same end, Eide et al. executed a study, which revealed that when comparing breech births with cephalic births the rate of CS and birth defects is higher in the first group, as is the percentage of preterm and small for gestational age infants. Despite these findings, when assessing intellectual performance, no difference was observed between males delivered in breech compared to cephalic presentation. On the contrary, when considering only breech presentation, intellectual performance among males delivered by CS was slightly lower in comparison to VD [21].
Regarding short and long-term outcomes of breech presentation, Mackay et al. analysed Apgar score, record of additional support needs (ASN) and level of education attainment in the following groups: Vaginal breech delivery, planned CS for breech presentation and vaginal cephalic delivery. Concerning the Apgar score, children born by vaginal breech delivery had lower Apgar scores than those born by cephalic vaginal delivery or planned CS for breech presentation. On the contrary, children delivery by planned CS for breech presentation had better Apgar scores than either group of VD. In terms of ASN, these were more common among children born by breech VD and these children were also more likely to achieve lower examination results. After adjusting for confounding variables, the levels of educational attainment were comparable between children born by planned CS for breech presentation and cephalic VD [22].
Serving the same purpose as the previous study, Macharey et al. assessed arterial pH, Apgar score and neurodevelopment at 4 years of age in children with breech presentation delivered by planned CS or vaginally after a trial of labour. Regarding short-term outcomes, the prevalence of an arterial pH below 7 and a 5 min Apgar below 7 was significantly increased in children delivered vaginally in comparison to those born by planned CS. Concerning neurological development at the age of 4 years, no significant difference was found between these two groups [23].
Influence of premature delivery
To assess the effect of mode of delivery in neurodevelopmental outcomes of preterm infants, Običan et al. conducted a study including children born between 23 4/7 and 25 6/7 weeks delivered by CS or VD in which the primary outcome was Bayley II scores at 2 years of age [41]. On both unadjusted and adjusted analyses there was no significant difference in Bayley scores between the group delivered by CS or VD [42]. Kimura et al. came to the same findings when studying a group of neonates born under 26 weeks, observing that after adjustment for potential confounding factors CS did not have a significant positive effect on neurodevelopment in comparison to VD. However, a subgroup analysis limited to breech presentation showed that CS was associated with improvement in neurodevelopmental outcomes [43].
Bentley et al. resorted to the AEDC instrument to evaluate development in school aged children, born at 32 or more weeks of gestation, which assessed 5 main domains and children were classified as Developmentally High Risk (DHR) if they were found to be developmentally vulnerable on ≥ 2 of those domains [44]. Contrarily to the previously mentioned studies, this last study revealed that children who were DHR were more likely to be male, small for gestational age or born to younger mothers with less income or who smoked during pregnancy, but, even after adjusting for these confounders, all modes of delivery that involved obstetric interventions were associated with a higher risk of being DHR when compared to VD after spontaneous labour, particularly CS after labour induction. Furthermore, they observed that the adjusted risk of being DHR decreased with increasing gestational age [45].
Regarding extremely low birth weight infants, the study of Minguez-Milio et al. involved neonates whose birth weight was under 1000 g and neurodevelopmental outcome was assessed using the McCarthy test, made up of six scales [46]. Their results showed that all the indices of the six scales were lower than normal reference values and when accounting for mode of delivery, children born by CS had higher values [47]. In opposition, Zhu et al. found no difference in neurodevelopmental outcomes at 2 years of age according to mode of delivery in infants whose birth weight was 1500 g or less [48].
Effects of drug administration during delivery
Aiming to analyse long-term effects of administration of exogenous oxytocin during labour in infant’s neurodevelopment, González-Valenzuela et al. conducted a study in children at the age of 5 years where they assessed the presence of developmental delay based on the total score in the Battelle Developmental Inventory [49]. They observed that the effect of oxytocin was mainly modified by maternal age and mode of delivery, being more noticeable in children born by non-instrumental VD to mothers under 28 or over 35 years, while the risk of developmental disorders decreased in infants born by noneutocic birth (instrumental VD or CS) to mothers whose age ranged between 28 and 35 years. Furthermore, this last group included women with higher risk pregnancies [30].
Regarding analgesia and anaesthesia, a search group of the Mayo Clinic performed two studies to assess a potential influence of anaesthesia for CS and neuraxial labour analgesia for VD on childhood learning disabilities [34,35]. The first study conducted by Sprung et al. revealed that children delivered by CS under general anaesthesia had lower birth weight, gestational age and Apgar scores, their mothers were more likely to have complications during pregnancy and delivery and the CS was more commonly emergent. However, children exposed to general or regional anaesthesia for CS were not more likely to develop learning disabilities than those born by VD. In fact, an adjusted analysis showed that the risk of learning disabilities was lower in children born by CS under regional anaesthesia when compared to VD [34]. The posterior study conducted by Flick et al. observed that mothers who received neuraxial analgesia were older, more likely to have had complications during pregnancy and delivery and had a higher rate of forceps or vacuum assisted deliveries. The unadjusted analysis revealed that the risk for learning disabilities was higher in children born by VD with neuraxial analgesia than those born by VD without neuraxial analgesia. However, after adjusting for confounding factors, there was no significant difference between the two groups [35].
Discussion
Vaginal delivery vs cesarean section
The association established in some studies of a higher rate of elective CS among older women with higher education level and income is possibly related to the fact that these women have more access to information and a more closely watched pregnancy, which translates to less complications during pregnancy and delivery and consequently better childhood health outcomes [2,6]. The contradiction presented in a study of an Australian cohort is likely due to the fact that in this study not only elective CS were considered but also non-scheduled CS, which are usually associated with a higher risk of complications and therefore worse outcomes [8].
Regarding neurocognitive outcomes, the fact that many studies revealed an insignificant difference between CS and vaginal birth, after the adjustment for confounding variables, suggests that a child’s neurodevelopment might be more influenced by other factors, such as maternal age, parental education and income, rather than mode of delivery itself [5,6,37]. Nevertheless, it should be considered that most of these studies were conducted with women who had uncomplicated pregnancies and deliveries, in order for the characteristics of the CS and VD groups to be comparable. Therefore, the findings of these studies may not be generalized to children whose mothers had a complicated pregnancy or needed to be submitted to an emergency CS for complications during delivery, such as breech presentation [5,6].
The similarities observed by Ahlberg et al. in school performance of children born by vacuum extraction and nonplanned CS suggest that both modes of delivery are equivalent alternatives for terminating deliveries regarding cognitive outcomes. However, it should be noted that this study was conducted in a country where birth by vacuum extraction is performed at a higher rate in comparison to other countries and therefore most professionals have a high level of experience. Consequently, these results cannot be generalized to situations in which vacuum extraction is rarely performed [36]. In spite of this limitation, the results of the study performed by Bahl et al. in a different context support the evidences of the previous study [15]. Furthermore, the small difference in school performance observed between instrumental delivery and non-scheduled CS and other modes of delivery reflect that the impact of the latest in these children’s lives will likely be minimal [36]. This difference may in turn be explained by the association between instrumental VD and emergency CS with an increased risk of low Apgar scores, fetal acidosis and moderate to severe neonatal encephalopathy [50,51].
Assessing obstetrical history of previous CS, the observed higher probability of developing learning disabilities in children born by unscheduled repeat CS compared to those born vaginally after CS may reflect the risk of scar rupture when attempting vaginal birth after CS, leading to unscheduled CS and potential hypoxic brain injury or death of the child [38,52].
Impact of breech presentation
Mackay et al. and Macharey et al. agreed that short-term outcomes in breech presentation were worse in children born by VD, confirmed by lower arterial pH and Apgar Scores in this group [22,23]. These findings are probably explained by the common occurrence of umbilical cord compression during the delivery of the fetal head. Therefore, it is important to select women eligible for vaginal labour, since breech presentation itself might constitute an indicator of obstetric risk factors and consequent adverse neurodevelopmental outcome [18,23].
Concerning long-term neurological development and intellectual performance, the studies analysed revealed different results. Molkenboer et al. found no difference in neurodevelopment in breech presentation according to mode of delivery, but only in children whose birth weight was under 3500 g. Therefore, birth weight should be considered when assessing long-term outcomes of mode of delivery in breech infants [39].
Similarly, the study conducted by Macharey et al. revealed no significant difference concerning neurological development at the age of 4 years between children with breech presentation according to mode of delivery. Furthermore, this study is strengthened by the fact that they were able to exclude other risk factors for adverse neurodevelopment outcome to evaluate the pure risk of vaginal breech delivery itself [23].
In disagreement with these findings, Eide et al. and Mackay et al. observed differences in intellectual performance according to mode of delivery in breech presentation. The first study noted that males delivered by CS performed at a lower intellectual level while the second observed that the lower education attainment was more common among children born by VD [21,22]. These contradictory findings may be explained by population selection bias, since the first study only refers to males, or the influence of covariables that weren’t accounted for. Furthermore, the study performed by Mackay et al. excluded multiple pregnancies, preterm deliveries and very low birth weight infants and therefore their results should not be generalized to these groups [22].
Influence of premature delivery
Običan et al. and Kimura et al. observed that in preterm infants, mode of delivery did not impact neurodevelopment [42,43]. Furthermore, Kimura et al. performed several sensitivity analyses to account for potential biases, such as missing data and found no changes in the results, which strengthens their findings. Regarding their analyses of preterm infants with breech presentation, the improvement in neurological outcomes associated to CS may be explained by the fact that occasionally labour in gestations <26 weeks progresses rapidly, leading to VD without the precautions required for a breech presentation and consequently worse outcomes [43].
In opposition to the findings of the previous studies, Bentley et al. observed that delivery by CS after labour induction was associated with higher risk of adverse neurodevelopmental outcomes. This study however focused on infants born at 32 or more weeks of gestation, while the previous assessed neurodevelopment in extremely preterm neonates (<26 weeks), which might contribute to their different results. Moreover, the age at which children were evaluated also differed among the studies, as the first two concerned children at 2-3 years of age while the latest focused on school aged children. This consideration is of great relevance since many neurological deficits may not be manifested until school age, therefore the absence of neurological impairment at a younger age does not assure that these children won’t have adverse neurological outcomes in the future [42,43,45]. Additionally, to overcome potential confounders, Bentley et al executed a subgroup analyses in women with low-risk pregnancies that supported their previous findings. Furthermore, their observation that adverse neurological outcomes decreased with increasing gestational age supports clinical guidelines that recommend that labour induction or preterm CS without medical indication should not be performed before 39 to 40 weeks of gestation [45].
Regarding extremely low birth weight infants, the studies of Minguez-Milio et al. and Zhu et al. presented contradictory results, however the studies once again differed in the age of which children were evaluated for neurological outcomes. The first had a longer followup period and revealed that children born by CS had better results while the second assessed children at 2 years of age and found no difference in outcomes according to mode of delivery, which correlates with the findings discussed above [47,48].
Effects of drug administration during delivery
The results of the study conducted by González-Valenzuela et al. can be grouped by maternal age: In women aged 28-35 years the use of oxytocin had a protective effect in dystocic delivery (higher risk pregnancies), while in women under 28 or over 35 years of age this effect was not observed, on the contrary it increased the risk of low scores in eutocic delivery. This contradiction in results may be explained by the fact that the first group is at higher risk for a complicated labour and so promoting the shortening of the first and second stages of labour with the use of oxytocin will accelerate the end of labour and reduce the risk for adverse outcomes [53]. Additionally, in these cases the fetal exposure to exogenous oxytocin is less prolonged. Contrarily, this exposure in the second group is longer, which might support the increased risk for developmental disorders in noncomplicated eutocic deliveries. On this note, an important factor that could help explain the contradictory findings would be the dose of oxytocin used in each case, however this variable was not accounted for, which should be considered as a limitation to this study [30].
The two studies performed by search groups of the Mayo Clinic were conducted with the purpose of being complementary [34,35]. The unexpected result of the study conducted by Sprung et al. that risk of learning disabilities was lower in children born by CS under regional anaesthesia could be explained by the organism’s stress response to labour and delivery [34]. Labour and VD are associated with a significant increase in the levels of stress hormones, which in the neonatal period may produce important changes in the developing brain and play a key role in neurodevelopmental outcomes [54,55]. Epidural anaesthesia for CS decreases stress hormone levels in both mother and fetus compared to VD and significantly decreases these levels compared to CS performed under general anaesthesia [55-57]. Therefore, the proposed hypothesis was that regional anaesthesia for CS would have a strong enough effect on the inhibition of the stress response to influence long-term neurodevelopmental outcomes [34]. With the intent to provide support for this hypothesis, Flick et al. focused on the effects of neuraxial analgesia in VD and found that the latest had no effect on the incidence of learning disabilities [35]. Regarding the stress response hypothesis, these finds do not offer reinforcement. However, even though neuraxial analgesia can decrease some levels of maternal stress response, its effects on neonatal stress response aren’t so clear [55,58]. Additionally, neuraxial analgesia does not prevent psychological stress associated with delivery, which might contribute to increase stress hormones despite pain control [59]. Furthermore, mothers who received neuraxial analgesia had higher rates of instrumental deliveries which may increase fetal stress and overcome the potential analgesic benefits in stress response. Lastly, it’s possible that neonatal stress has no influence in neurodevelopmental outcomes and therefore the stress response hypothesis cannot support the previous findings concerning regional anaesthesia and CS. Nevertheless, the possibility of confounding factors that weren’t accounted for having affected the results cannot be excluded. Moreover, another limitation to both studies is that the inhalation agents used in general anaesthesia for CS and the techniques used to provide neuraxial analgesia in the study period are not in accordance with current practices [34,35].
Review’s Key Points
Vaginal delivery vs cesarean section
• Regarding uncomplicated pregnancies and deliveries, most studies analysed couldn’t support an association between mode of delivery and children’s neurocognitive outcomes [5,6,37].
• Concerning operative delivery, the tendency for lower scores when assessing school performance in children born by instrumental delivery and non-scheduled CS will probably have a minimal influence in future neurodevelopment [15,36].
Impact of breech presentation
• Short-term outcomes in children born by breech VD were consistently poorer when compared to those born by planned CS [22,23].
• The results concerning long-term neurological outcomes in breech infants were contradictory [21-23,39].
Influence of premature delivery
• Adverse neurological outcomes were in general more common in preterm infants [47].
• Neurological outcomes improve with increasing gestational age [45].
• In preterm infants, neurocognitive outcomes varied according to the age at which children were assessed. The studies where children were evaluated at 2-3 years of age revealed no difference between mode of delivery and neurodevelopment in opposition to those where children were evaluated later in life [42,43,45,47,48].
• The results vary according to the characteristics of some subgroups, such as extremely premature infants, premature infants with breech presentation and extremely low birth weight infants [43,47,48].
Effects of drug administration during delivery
• Oxytocin is an undeniably important agent in situations where labour acceleration is necessary to improve maternal and neonatal outcomes [30].
• The long-term neurological effects of children exposed to exogenous oxytocin are still unclear [30].
• Transitory neonatal exposure to anaesthetic drugs during delivery probably won’t harmfully influence long-term neurodevelopment [34,35].
• The proposed hypothesis that regional anaesthesia for CS reduces the fetal stress response to VD and consequently has significant effects on later neurodevelopment was not supported by a posterior study [34,35].
Limitations
• Most studies focused on selected population cohorts, therefore some of the results cannot be generalized, constituting a selection bias.
• Neurodevelopment is influenced by a vast number of genetic and environmental variables, becoming impracticable to account for all factors that may affect neurocognitive development.
Recommendations
Future investigation is necessary to enlighten if neurodevelopment is in fact associated with mode of delivery or if underlying causes are the real influencers.
Conclusions
1. As observed in previous studies, the findings in this review regarding uncomplicated pregnancies and deliveries cannot support an association between vaginal or cesarean delivery and neurodevelopmental outcomes, apart from nonplanned cesarean section which usually correlates to worse outcomes, since it’s normally associated with emergent situations.
2. Focusing on operative deliveries, a small difference was observed in school performance of children born by instrumental vaginal delivery and nonplanned cesarean section in comparison to those born by noninstrumental vaginal delivery or planned cesarean, nonetheless this should have a minimal impact in a child’s future neurodevelopment.
3. Concerning deliveries in breech presentation, short-term outcomes in children born by vaginal delivery were consistently poorer when compared to those born by planned cesarean, however long-term neurological outcomes of these neonates according to mode of delivery were contradictory and therefore further studies are needed to assess optimal mode of delivery in this group.
4. In general, preterm infants were more commonly associated with adverse neurological outcomes regardless of mode of delivery and it was observed that the latest decreased with increasing gestational age, thus delivery should be postponed as much as possible, in the absence of risk circumstances that endanger both mother and child, to ensure the best developmental outcomes. Moreover, in this group of infants, neurocognitive outcomes undoubtedly varied according to the age at which children were evaluated, which enforces the need for studies with longer follow-up time to truly assess the effects of premature delivery in neurodevelopment. Furthermore, the results regarding premature birth and mode of delivery must be cautiously considered given the fact that they vary considerably according to the characteristics of some subgroups, such as extremely premature infants, premature infants with breech presentation and extremely low birth weight infants.
5. Considering the most commonly used drugs in the obstetric setting and their possible effects in neurodevelopment, this review showed that, for instance, the long-term neurological effects of children exposed to exogenous oxytocin are still unclear and so its use should be limited in terms of length of exposure and dose (lowest effective dose).
6. The findings also suggest that a transitory neonatal exposure to anaesthetic drugs during delivery probably won’t harmfully influence long-term neurodevelopment. Additionally, one study proposed the hypothesis that regional anaesthesia for cesarean delivery might reduce the fetal stress response to vaginal delivery and consequently have significant positive effects on later neurodevelopment. This fact was not supported by a posterior study, nevertheless, more research should be conducted to further assess the feasibility of this hypothesis.
7. Effectively, neurodevelopment is influenced by a vast number of genetic and environmental variables and this fact constitutes the most important limitation to this review, because even though the analysed studies proceeded with adjustments for possible confounding covariables, it’s impracticable to account for all factors that may affect neurocognitive development. Thus, all findings should always be cautiously interpreted.
8. Lastly, given the conflicting findings in this review, future investigation is necessary to enlighten if neurodevelopment is in fact associated with mode of delivery or if eventually the latest is dictated by unidentified underlying causes which would consequently be the real influencers in neurodevelopmental outcomes.
9. In sum, the core message of this review is that when considering mode of delivery, every obstetrical case should be individually analysed. Medical practitioners should evaluate the maternal and neonatal risks and benefits of the different modes of delivery in each specific situation (uncomplicated delivery, breech delivery, preterm delivery), educate the mothers and try to demystify certain beliefs to help them make an informed decision and promote their children’s healthy development.
References
- Souza JP, Betran AP, Dumont A, Mucio B, Pickens GCM, et al. (2016) A global reference for caesarean section rates (C-Model): A multicountry cross-sectional study. BJOG 123: 427-436.
- Smithers LG, Mol BW, Wilkinson C, Lynch JW (2016) Implications of caesarean section for children's school achievement: A population-based study. ANZJOG 56: 374-380.
- Habiba M, Kaminski M, Da Fre M, Marsal K, Bleker O, et al. (2006) Caesarean section on request: A comparison of obstetricians’ attitudes in eight European countries. BJOG 113: 647-656.
- Khadem N, Khadivzadeh T (2010) The intelligence quotient of school aged children delivered by cesarean section and vaginal delivery. Iran J Nurs Midwifery Res 15: 135-140.
- Li HT, Ye RW, Pei LJ, Ren AG, Zheng XY, et al. (2011) Cesarean delivery on maternal request and childhood intelligence: A cohort study. Chin Med J 124: 3982-3987.
- Gibbons L, Belizán JM, Lauer JA, Betrán AP, Merialdi M, et al. (2010) The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: Overuse as a barrier to universal coverage. World Health Report 30: 1-31.
- Robson SJ, Vally H, Abdel-Latif ME, Yu M, Westrupp E (2015) Childhood health and developmental outcomes after cesarean birth in an Australian cohort. Pediatrics 136: e1285-e1292.
- Liu S, Heaman M, Joseph KS, Liston RM, Huang L, et al. (2005) Risk of maternal postpartum readmission associated with mode of delivery. Obstet Gynecol 105: 836-842.
- Cardwell CR, Stene LC, Joner G, Cinek O, Svensson J, et al. (2008) Caesarean section is associated with an increased risk of childhood-onset type 1 diabetes mellitus: A meta-analysis of observational studies. Diabetologia 51: 726-735.
- Cho CE, Norman M (2013) Cesarean section and development of the immune system in the off- spring. Am J Obstet Gynecol 208: 249-254.
- Thavagnanam S, Fleming J, Bromley A, Shields M, Cardwell C (2008) A meta-analysis of the association between caesarean section and childhood asthma. Clin Exp Allergy 38: 629-633.
- Li HT, Zhou YB, Liu JM (2013) The impact of cesarean section on offspring overweight and obesity: A systematic review and meta-analysis. Int J Obes 37: 893-899.
- Towner D, Castro MA, Eby-Wilkens E, Gilbert WM (1999) Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med 341: 1709-1714.
- Bahl R, Patel, RR, Swingler R, Ellis M, Murphy DJ (2007) Neurodevelopmental outcome at 5 years after operative delivery in the second stage of labor: A cohort study. Am J Obstet Gynecol 197(2):147.
- Albrechtsen S, Rasmussen S, Dalaker K, Irgens LM (1998) Perinatal mortality in breech presentation sibships. Obstet Gynecol 92: 775-780.
- Lyons J, Pressey T, Bartholomew S, Liu S, Liston RM, et al. (2015) Delivery of breech presentation at term gestation in Canada, 2003-2011. Obstet Gynecol 125: 1153-1161.
- Macharey G, Gissler M, Rahkonen L, Ulander VM, Väisänen-Tommiska M, et al. (2017) Breech presentation at term and associated obstetric risks factors-a nationwide population based cohort study. Arch Gynecol Obstet 295: 833-838.
- Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, et al. (2000) Planned caesarean section versus planned vaginal birth for breech presentation at term: A randomised multicentre trial. Lancet 356: 1375-1383.
- Whyte H, Hannah ME, Saigal S, Hannah WJ, Hewson S, et al. (2004) Outcomes of children at 2 years after planned cesarean vs planned vaginal delivery for breech presentation at term: The international randomized Term Breech Trial. Am J Obstet Gynecol 191: 864-871.
- Eide MG, Øyen N, Skjærven R, Irgens LM, Bjerkedal T, et al. (2005) Breech delivery and intelligence: A population-based study of 8,738 breech infants. Obstet Gynecol 105: 4-11.
- Mackay DF, Wood R, King A, Clark DN, Cooper SA, et al. (2015) Educational outcomes following breech delivery: A record-linkage study of 456947 children. Int J Epidemiol 44: 209-217.
- Macharey G, Väisänen-Tommiska M, Gissler M, Ulander VM, Rahkonen L, et al. (2018) Neurodevelopmental outcome at the age of 4 years according to the planned mode of delivery in term breech presentation: A nationwide, population-based record linkage study. J Perinat Med 46: 323-331.
- Davis EP, Buss C, Muftuler T, Head K, Hasso A, et al. (2011) Children's brain development benefits from longer gestation. Front psychol 2: 1.
- Kim DJ, Davis EP, Sandman CA, Sporns O, O'donnell BF, et al. (2014) Longer gestation is associated with more efficient brain networks in preadolescent children. Neuroimage 100: 619-627.
- Alfirevic Z, Milan SJ, Livio S (2012) Caesarean section versus vaginal delivery for preterm birth in singletons. Cochrane Database Syst Rev 9: CD000078.
- Ment LR, Oh W, Philip AG, Ehrenkranz RA, Duncan CC, et al. (1992) Risk factors for early intraventricular hemorrhage in low birth weight infants. J Pediatrics 121: 776-783.
- Rice D, Barone S (2000) Critical periods of vulnerability for the developing nervous system: Evidence from humans and animal models. Environ Health Perspect 108: 511-533.
- Middaugh LD, Dow-Edwards D, Li AA, Sandler JD, Seed J, et al. (2003) Neurobehavioral assessment: A survey of use and value in safety assessment studies. Toxicol Sci 76: 250-261.
- González-Valenzuela MJ, GarcÃa-Fortea P, Delgado-RÃos M, Cazorla-Granados O, Blasco-Alonso M, et al. (2014) Effects of oxytocin used during delivery on development: A retrospective cohort study. J Clin Exp Neuropsychol 36: 680-690.
- WHO (2011) WHO recommendations for induction of labour. Geneva: World Health Organization.
- Malek A, Blann E, Mattison DR (1996) Human placental transport of oxytocin. J Matern Fetal Med 5: 245-255.
- Gressens P, Mesples B, Sahir N, Marret S, Sola A (2001) Environmental factors and disturbances of brain development. Semin Neonatol 6: 185-194.
- Sprung J, Flick RP, Wilder RT, Katusic SK, Pike TL, et al. (2009) Anesthesia for cesarean delivery and learning disabilities in a population-based birth cohort. Anesthesiology 111: 302-310.
- Flick RP, Lee K, Hofer RE, Beinborn CW, Hambel EM, et al. (2011) Neuraxial labor analgesia for vaginal delivery and its effects on childhood learning disabilities. Anesth Analg 112: 1424-1431.
- Ahlberg M, Ekéus C, Hjern A (2014) Birth by vacuum extraction delivery and school performance at 16 years of age. Am J Obstet Gynecol 210: 361.e1-8.
- Polidano C, Zhu A, Bornstein JC (2017) The relation between cesarean birth and child cognitive development. Sci Rep 7: 11483.
- Black M, Bhattacharya S, Philip S, Norman JE, McLernon DJ (2016) Planned repeat cesarean section at term and adverse childhood health outcomes: A record-linkage study. PLoS Med 13: e1001973.
- Molkenboer JFM, Roumen FJME, Smits LJM, Nijhuis JG (2006) Birth weight and neurodevelopmental outcome of children at 2 years of age after planned vaginal delivery for breech presentation at term. Am J Obstet Gynecol 194: 624-629.
- Squires J, Potter L, Bricker D (1995) The ASQ user's guide for the ages & stages questionnaires: A parent-completed, child-monitoring system. Paul H Brookes Publishing.
- Lowe JR, Erickson SJ, Schrader R, Duncan AF (2012) Comparison of the Bayley II Mental Developmental Index and the Bayley III Cognitive Scale: Are we measuring the same thing? Acta paediatr 101: e55-58.
- Obican SG, Small A, Smith D, Levin H, Drassinower D, et al. (2015) Mode of delivery at periviability and early childhood neurodevelopment. Am J Obstet Gynecol 213: 578.e1-4.
- Kimura T, Takeuchi M, Imai T, Tanaka S, Kawakami K, et al. (2017) Neurodevelopment at 3 years in neonates born by vaginal delivery versus cesarean section at <26 weeks of gestation: Retrospective analysis of a nationwide registry in Japan. Neonatology 112: 258-266.
- Brinkman SA, Gregory TA, Goldfeld S, Lynch JW, Hardy M (2014) Data resource profile: The Australian early development index (AEDI). Int J Epidemiol 43: 1089-1096.
- Bentley JP, Roberts CL, Bowen, JR, Martin AJ, Morris JM, et al. (2016) Planned birth before 39 weeks and child development: A population-based study. Pediatrics 138: e20162002.
- McCarthy D (1972) Manual for the McCarthy scales of children’s abilities. New York: The psychological corporation.
- Minguez-Milio JA, Alcázar JL, Aubá M, Ruiz-Zambrana Ã, Minguez J (2011) Perinatal outcome and long-term follow-up of extremely low birth weight infants depending on the mode of delivery. J Matern Fetal Neonatal Med 24: 1235-1238.
- Zhu JJ, Bao YY, Zhang GL, Ma LX, Wu MY (2014) No relationship between mode of delivery and neonatal mortality and neurodevelopment in very low birth weight infants aged two years. World J Pediatr 10: 227-231.
- Dela-Cruz, MV, González M (2009) Inventario de desarrollo Battelle [Battelle development inventory]. Madrid: Tea Ediciones SA.
- Ladfors L, Thiringer K, Niklasson A, Odeback A, Thornberg E (2002) Influence of maternal, obstetric and fetal risk factors on the prevalence of birth asphyxia at term in a Swedish urban population. Acta obstetr Gynecol Scand 81: 909-917.
- Kjellmer I, Beijer E, Carlsonn G, Hrbek A, Viggedal G (2002) Follow-up into young adulthood after cardiopulmonary resuscitation in term and near term newborn infants. I. Educational achievements and social adjustments. Acta Paediatr 91: 1212-1217.
- Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, et al. (2004) Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med 351: 2581-2589.
- Patka JH, Lodolce AE, Johnston AK (2005) High-versus low-dose oxytocin for augmentation or induction of labor. Ann Pharmacother 39: 95-101.
- Charmandari E, Kino T, Souvatzoglou E, Chrousos GP (2003) Pediatric stress: Hormonal mediators and human development. Horm Res 59: 161-179.
- Vogl SE, Worda C, Egarter C, Bieglmayer C, Szekeres T, et al. (2006) Mode of delivery is associated with maternal and fetal endocrine stress response. BJOG 113: 441-445.
- Taylor A, Fisk NM, Glover V (2000) Mode of delivery and subsequent stress response. Lancet 355: 120.
- Loughran PG, Moore J, Dundee JW (1986) Maternal stress response associated with caesarean delivery under general and epidural anaesthesia. BJOG 93: 943-949.
- Abboud TK, Sarkis F, Hung TT, Khoo SS, Varakian L, et al. (1983) Effects of epidural anesthesia during labor on maternal plasma beta-endorphin levels. Anesthesiology 59: 1-5.
- Kramer MS, Lydon J, Séguin L, Goulet L, Kahn SR, et al. (2009) Stress pathways to spontaneous preterm birth: The role of stressors, psychological distress and stress hormones. Am J Epidemiol 169: 1319-1326.
Citation: Meireles JP, Machado HS (2018) The Influence of Mode of Delivery on the Neurodevelopment of Children and Adolescents. J Preg Child Health 5: 378. DOI: 10.4172/2376-127X.1000378
Copyright: © 2018 Meireles JP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6802
- [From(publication date): 0-2018 - Apr 21, 2025]
- Breakdown by view type
- HTML page views: 5798
- PDF downloads: 1004