The Importance of Ocular Prosthetic in Sudan
Received: 27-Oct-2018 / Accepted Date: 26-Nov-2018 / Published Date: 03-Dec-2018 DOI: 10.4172/2476-2075.1000128
Abstract
Introduction: The eye removal surgery is undertaken only when all other eye treatments are ineffective, inappropriate or undesirable. An ocular prosthesis or artificial eye (a type of craniofacial prosthesis) replaces an absent natural eye following an enucleation, evisceration, or orbital exenteration. The prosthesis fits over an orbital implant and under the eyelids.
Objectives: This study aimed to improve the patient aesthetics, point out the need for prosthesis department and to highlight the need for a trained ocularist.
Methods: A descriptive hospital based study was carried out on 12 subjects who underwent enucleation, evisceration and ocular prosthesis fitting recruited from Makkah Eye Complex (MEC), part of Al Basar International Foundation, Al Rayad, Khartoum Sudan. Data was collected, cleaned and analyzed using SPSS version 25.0.
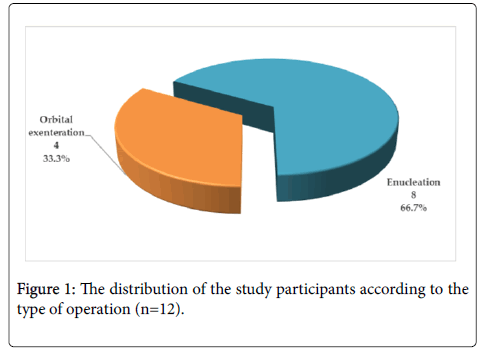
Results: This study includes 12 participants. All of the study participants had an eye removed because of injury. Only one third (33.3%) had orbital evisceration and the remaining (66.7%) had eye enucleation. According to this study; 58.3% of the participants stated that there was no matching of the artificial eye color with the natural eye color, 16.7% of them noticed buildup of deposits on the prosthetic eye, 41.7% had problems in depth perception, so they faced difficulty in pouring water in a jug or tea in the cup, while 16.7% of them had stopped using the artificial eye within less than one year.
Conclusion and recommendations: Health authority in Sudan should take into account the need for establishment of a prosthetic eye department in Sudan that will provide artificial eye services, a manufacturing and fitting service for the supply of ocular prostheses to all patients throughout the country, in addition to the need for trained ocularists.
Keywords: Orbital exenteration; Eye enucleation; Ocular prosthesis; Artificial eye; Sudan
Introduction
Loss of an eye due to tumor or trauma, or end-stage ocular disease is devastating to a person of any age. Not only is there a loss of binocular vision with reduced peripheral visual field and loss of depth perception, but also a sense of facial disfigurement, one’s self-image, due to which self-confidence may be affected. The disfigurement associated with the loss of an eye can cause significant physical and emotional problem [1].
The rehabilitation of a patient who has suffered the psychological trauma of an ocular loss requires a prosthesis that will provide the optimum cosmetic and functional result. Ocular prosthetics made from cryolite glass or perspex can be manufactured and fitted 5-8 weeks after removal of the eye. During this period, a conformer is placed within the conjunctival sac in order to prevent scar formation and shrinking of the socket [2]. Ocular prosthetics act as replacement for the natural eye. Although the replacement cannot provide sight, it fills the cavity of the eye socket as a cosmetic enhancement. It also enhances the psychological well-being and social interaction [3]. Someone with an ocular prosthesis is totally blind on the affected side and has monocular (one sided) vision which affects depth perception. An ocular prosthesis or artificial eye (a type of Craniofacial prosthesis) replaces an absent natural eye following an enucleation (removal of the whole eye ball after severing the muscle, nerve and vascular attachment), evisceration (removal of the eye ball content) or orbital exenteration (surgical removal of the globe in addition to orbital content, muscles, lids and fat) [4]. The prosthesis fits over an orbital implant or empty orbit and under the eyelid. Often referred to as a glass eye, the ocular prosthesis roughly takes the shape of a convex shell and is made of medical grade plastic acrylic. A few ocular prostheses today are made of cryolite glass. There is also a variant of ocular prosthesis with a very thin hard shell known as scleral shell that can be worn over a damaged eye and makers of such ocular prosthetics are known as ocularists [5].
According to the annual report of operations in Makkah Eye Complex in Khartoum, Sudan, nearly 73 to 160 people lose an eye every year. The question that arises here is, is there a need for ocular prosthetic department in the Sudan? The main aim of this study is to improve the patient’s aesthetics, point out the need for ocular prosthesis department and to highlight the need for trained ocularists.
Materials and Methods
Study design
A descriptive hospital based study was carried out on subjects who have normal vision in their surviving eye and had undergone enucleation, evisceration and readymade artificial eye fitted in their other eye. A survey to evaluate their needs and problems that they faced was completed. The subjects were recruited from Makkah Eye Complex (MEC) as part of Al Basar International Foundation, Al Rayad, Khartoum, Sudan [6].
Study population
A descriptive hospital based study was carried out on 12 subjects who underwent enucleation, evisceration and had ocular prosthesis fitting. A 35 question survey was completed to evaluate their needs and the problems that they faced. Only participants with normal vision in the remaining eye were included.
Materials used
Plastic stock eyes from ZABBYS, India; Snellen Vision Testing Chart; Trial set and Trail frame; Pen-light-lamp, type: lens end lamp 2.2V; Data form; Hand held plastic ruler; Sony digital camera (12.1 mega pixels).
Sampling
The appropriate 12 sample were selected from Makkah Eye Complex. For ethical consideration, written approval for conducting this research was obtained from Al-Neelain University. Verbal consent was obtained from all participants enrolled in the study. Study data/ information was used for research purpose only. The privacy issues have been taken into consideration.
Tools of data collection
Comprehensive closed-ended data collection form for patients was used.
Data management
Data was collected, cleaned and analyzed using SPSS version 25.0. Data presentation was in the form of tables and figures including variable table and time trend curves.
Results & Discussion
Patient survey
Considering the patients’ survey findings, the study found out that two thirds of the study participants were more than 40 years in age, two thirds of them were males from wide range of jobs. To some extent, these findings are similar with a Turkish study, which revealed that the average age was ranged 3-80 years. The number of male in the patient group was 74.8% and female was 25.2%. Patients who underwent evisceration were 77.2%, whereas 22.8% of them had undergone enucleation [7].
The study has found out that all of the 12 study participants had undergone eye removal because of injuries as shown in Figure 1.
On a study by Koylu et al. in Turkey, the findings were different. They stated that the leading indications for eye amputations were trauma (50.4%), malignancy (16.3%), painful blind eye and absolute glaucoma (16.3%) [7]. Another study from Iceland showed that the most common causative diagnosis for enucleation was traumatic lesion (39%) [8].
The study found out that only one third i.e. 4 (33.3%) had eye evisceration and the remaining 8 (67.7%) had eye enucleation. Half of them had the operation in right eye while the half had operated the left eye, and only 2 (16.7%) of them had operated the dominant eye as detailed in Table 1.
| Operation characteristics | Frequency | Percent | |
|---|---|---|---|
| Cause of enucleation | Injury | 12 | 100.0 |
| Type of operation | Orbital evisceration | 4 | 33.3 |
| Enucleation | 8 | 66.7 | |
| The Enucleated eye | Right eye | 6 | 50.0 |
| Left Eye | 6 | 50.0 | |
| Was it the dominant eye | Yes | 2 | 16.7 |
| No | 10 | 83.3 | |
Table 1: The distribution of the study participants according to their operation characteristics (n=12).
Other studies explained that evisceration surgery is usually preferred in extremely severe trauma cases, while enucleation is used in advanced cases of intraocular malignancy [7]. The study found out that all patients depend on themselves for movement. Moreover, only 16.7% of them stated that they used suitable artificial eye size. 25% of them with small size and 41.7% had large size. The study showed that 58.3% of them stated that there was no matching of the artificial eye color with the original eye color. Also, 16.7% of them noticed deposits build up on prosthetic eye. Less than half of the study participants (41.7%) wearing protective glasses, and only 16.7% had received training to adapt with eye loss as shown in Table 2.
| General findings | Frequency | Percent | |
|---|---|---|---|
| Patient depend on him/herself in movement | Yes | 12 | 100.0 |
| No | 0 | 0.0 | |
| Small | 3 | 25.0 | |
| Large | 5 | 41.7 | |
| Size of artificial eye used | Suitable | 2 | 16.7 |
| Do not use | 1 | 8.3 | |
| Stopped to use | 1 | 8.3 | |
| Matching of the artificial eye color with the original eye color | Suitable | 5 | 41.7 |
| Not suitable | 7 | 58.3 | |
| Noticed deposits build up on prosthetic eye | Present | 4 | 33.3 |
| Absent | 8 | 66.7 | |
| Noticed change in artificial eye color | Present | 2 | 16.7 |
| Absent | 10 | 83.3 | |
| Wearing protective glasses | Yes | 5 | 41.7 |
| No | 7 | 58.3 | |
| Received training to adapt with eye loss | Yes | 2 | 16.7 |
| No | 10 | 83.3 | |
Table 2: The distribution of the study participants according to their general findings n=12).
Another study from Japan went further in the impact of eye removal on the patient. They stated that the removal of an eye can result in depression, difficulties in driving, perceived problems with physical appearance and coping difficulties [9].
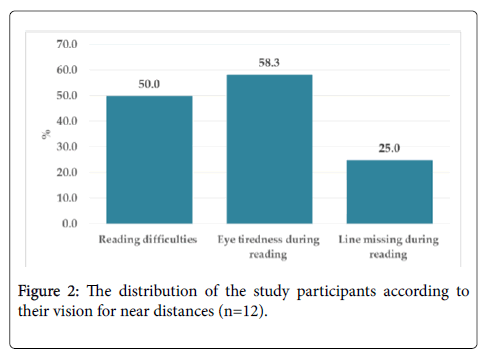
Considering the patients’ vision for near distances, the study points out that half of the study participants had reading difficulties. 58.3% had tiredness in the eye during reading and 25% of them had at least one line missing during reading as in Figure 2.
Other study agreed with this study that the patients may had eye fatigue during reading as an associated complications which are mandatory for a durable functional, esthetic and psychosomatic rehabilitation after ocular extirpation [7].
This study also found out that 41.7% had problems in depth perception, so they face difficulty in pouring the water in jug or the tea in the cup.
Similarly, another study reveals that loss of depth perception and reduced visual range was equally concerning [8]. The study found out that one third of the study participants (33.3%) do not remove the artificial eye and wash it before sleep, 41.7% don’t clean the eye cavity, 58.3% visit the doctor regularly.
Furthermore, the study found that 41.7% do not keep the artificial eye in special box, 83.3% do not use a special solution for artificial eye wash and 8.3% do not wash their hand before touching and wearing the artificial eye. Studies claimed that eyes are very sensitive to irritation. Any irregularity in eye prosthesis would lead to discomfort and can affect the patient compliance for cleaning and reservation and care [9].
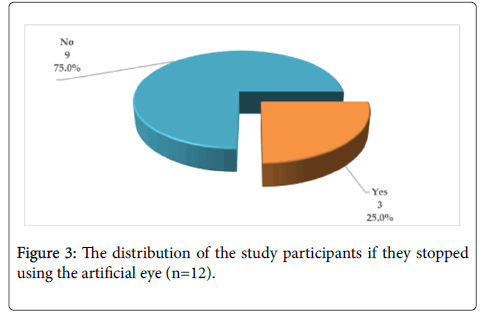
The study found that most of the study participants (91.7%) noticed presence of dirt in the artificial eye. The study realized that one quarter of the study participants had stopped using the artificial eye. 16.7% of them stopped using the artificial eye within less than one year as shown in Figure 3.
The causes to stop using artificial eye were pain (33.3%), change of the artificial eye (33.3%) and inappropriate size of the artificial eye (big in size). All these difficulties highlights the need for training ocularists, in addition to detailed medical history that includes the condition that led to the excision and enucleation in order to alert the possibility of recurrence [7].
Conclusion
This study covered 12 study participants who were recruited from a single eye hospital (Makkah Eye Complex). The study finds that 12 of the study participants had eye removal because of injuries out of which only one third had orbital evisceration and the remaining had eye enucleation.
Limitations of the study, relatively limited number of study participant (12) from one study area may affect negatively in the probability finding. Another limitation is follow up. Some outcomes such as long term outcome or the presence of complication may need to be followed overtime for longer period.
Health authority in Sudan should take into account the need for establishment of an artificial eye department in Sudan that provides updated artificial eye services including manufacturing and fitting services for the supply of ocular prostheses to all patients throughout the country in addition to the need of trained ocularists.
It is required to verify all the details of the private clinic in order to gain the confidence of the patient and a detailed medical history that includes the condition that led to the excision and enucleation in order to alert the possibility of recurrence.
Conflict of Interest
The authors declare that there is no conflict of interest.
Authors' Contributions
All authors have contributed in reviewing the manuscript. The corresponding author has the right on behalf of all authors on a worldwide basis to grant permit of this paper.
References
- Lubkin V, Sloan S (1990) Enucleation and psychic trauma. Adv Ophthalmic Plast Reconstr Surg. 8:259-262.
- Koch KR, Trester W, Müller-Uri N, Trester M, Cursiefen C et al. (2016) Ocular prosthetic. Fitting, daily use and complication. Ophthalmologe 113: 133-142.
- Hatamleh MM, Alnazzawi AA, Abbariki M, Alqudah N, Cook AE (2017) Survey of ocular prosthetics rehabilitation in the united Kingdom, Part 2:Anophtalmic patient satisfaction and Acceptance. J Craniofac Surg 28: 1297-1301.
- Micheal O. Hughes. Anatomy of the anterior eye for ocularists (2004) Journal of Ophthalmic Prosthetics.
- Annual Report of Operations, Makkah Eye Complex, Khartoum, Sudan, 2011-2012.
- Koylu MT, Gokce G, Uysal Y, Ceylan OM, Akıncıoglu D, et al. (2015) Indications for eye removal surgeries. A 15-year experience at a tertiary military hospital. Saudi Med J 36: 1205-1209.
- Geirsdottir A, Agnarsson BA, Helgadottir G, Sigurdsson H. (2014) Enucleation in Iceland 1992-2004: Study in a defined population. Acta Ophthalmol 92: 121-125.
- Kondo T, Tillman WT, Schwartz TL, Linberg JV, Odom JV. (2014) Health Related Quality of Life after Surgical Removal of An Eye. Ophthal Plast Reconstr Surg 29:51-56.
Citation: Ahmed Aldow MO, Ali El-Awad ME (2018) The Importance of Ocular Prosthetic in Sudan. Optom Open Access 3: 127. DOI: 10.4172/2476-2075.1000128
Copyright: © 2018 Ahmed Aldow MO, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4472
- [From(publication date): 0-2018 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 3633
- PDF downloads: 839