The Importance of a Preventive Oral Hygiene in Chemotherapy and Radiotherapy: A Case Report
Received: 30-Jun-2022 / Manuscript No. JOHH-22-68944 / Editor assigned: 02-Jul-2022 / PreQC No. JOHH-22-68944(PQ) / Reviewed: 16-Jul-2022 / QC No. JOHH-22-68944 / Revised: 21-Jul-2022 / Manuscript No. JOHH-22-68944(R) / Accepted Date: 25-Jul-2022 / Published Date: 28-Jul-2022 DOI: 10.4172/2332-0702.1000325
Abstract
Chemotherapy and radiotherapy are treatments that can cause serious short and long-term side effects, by affecting different body areas, the oral cavity included. There are immediate or late-term side effects on the oral cavity. The side effects of cervical-cephalic radiotherapy are borne by the treated area and depend on the treatment volumes and dose of radiation and drugs administered. Other factors: the age of the patient, associated therapies, psychological attitude of the patient to the disease, as well as individual sensitivity to radiation, also affect the extent of these effects.
Dietary and oral hygiene changes, oesophageal reflux disease can cause tooth tissue demineralisation with enamel erosion and increase the risk of tooth decay if appropriate preventive interventions are not planned.
Keywords: Oral Health; Chemotherapy; Radiotherapy
Keywords
Oral Health; Chemotherapy; Radiotherapy
Introduction
The clinical case concerns a patient of 60 years old, female, which come to my attention in a compromised state of general and oral health, due to breast cancer is performing radiotherapy and chemotherapy (Figure 1).
The clinical examination and the history have shown a lack of knowledge of the importance of oral hygiene before and during chemo and radiotherapy. As a professional in the health of oral hygiene I set myself the goal of transmitting this concept, to show the patient the critical issues in her oral cavity and motivate her to improve the situation and with it the health of both hard and soft tissues [1].
Case Report
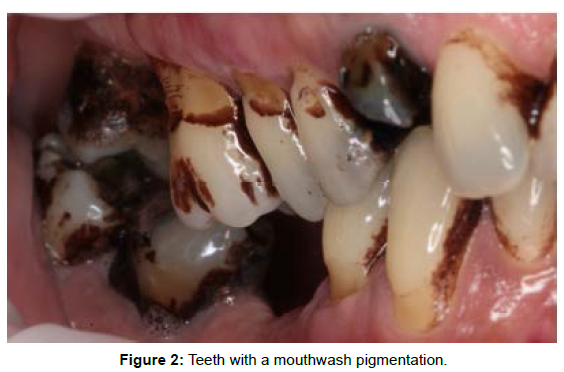
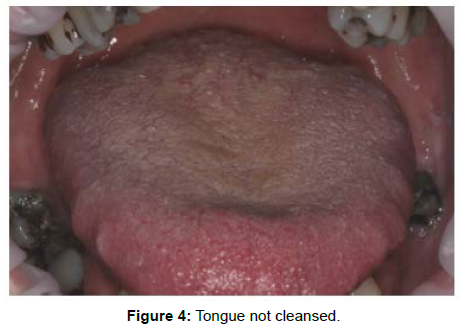
The patient is submitted to the documentation of the case through intra-oral photos, both without and with the use of the plaque-detector (useful to provide the patient with visual evidence of the presence of both plaque and tartar, which the naked eye could not identify) [2]. With the mirror and the picture of the teeth i start my session of motivation and instruction (Figure 2).
I proceed with the use of the electric toothbrush, to show the patient that an “Electric” device with the suitable head can facilitate the cleaning of the teeth (Figure 3).
Professional treatment
She received a professional periodontal treatment. Periodontal therapy consisted of plaque control with a tri-tone-plaque-detector, showed that she was very careful to scrupulously perform the oral hygiene protocols at home customized for her [4].
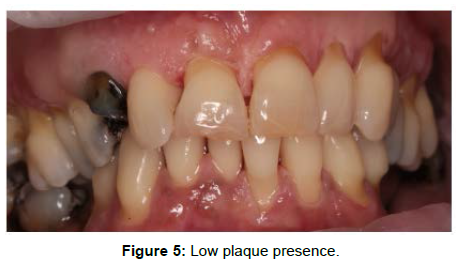
The use of technologies such as photography and plaque detector, allowed me to motivate the patient and show the effects of plaque and tartar in hard and soft tissues; -Airflow, ultrasound with modulating power allowed me to work on the patient without her experiencing pain; -Professional products have allowed me to restore integrity to dental enamel and reduce post-hygiene bleeding (Figure 5).
If the management of the patient in radio and chemotherapy is not immediate and preventive we can have long-term side effects. Long-term side effects:
• Hyposcialia (dryness);
• Carious processes;
• Telangiectasia (dilation of blood vessels); Mucosal
• Fragility; Infections;
• Trismus (jaw muscles contractures); Muscle fibrosis;
• Decrease in vascularisation;
• Soft tissue necrosis;
• Osteoradionecrosis;
• Dental and facial malformations.
• Mucositis and stomatitis manifest themselves with erosions and ulcerations with possible over- infection by microorganisms (mycosis); they cause pain and difficulty in chewing.
The intensity of this effect is variable and individual and may be greater when radiation therapy is associated with chemotherapy. Thorough oral hygiene after meals and dental remediation before the start of radiotherapy reduces the extent of such side effects [5].
Dryness of the oral cavity: it is caused by the reduction of the salivary production caused by the irradiation of the salivary glands; this effect can last for some months after the end of the radiotherapy and in some cases it can become permanent [6].
Conclusion
Oral Hygiene procedures before, during and after chemo and radiograph are necessary and safe: every patient should be assessed for dental hygiene habits and oral problems. Good oral hygiene, brush twice a day and floss once a day, good nutrition ,regular visits to the dental hygienist can prevent immediate effects. The maintenance of optimal conditions of the oral cavity is crucial to avoid further problems in the patient with a psychological and health state already compromised by the therapies. The dental hygienist and dentist support can prevent or reduce mouth disease.
Conflict of Interest
I declare that I not have conflict of interest.
References
- McGuire DB, Fulton JS, Park J, Brown CG, Correa MEP, et al. (2013) Systematic review of basic oral care for the management of oral mucositis in cancer patients. Support Care Cancer 21: 3165-3177.
- Valdez JA, Brennan MT (2018) Impact of Oral Cancer on Quality of Life. Dent Clin North Am 62: 143-154.
- Levi LE, Lalla RV (2018) Dental Treatment Planning for the Patient with Oral Cancer. Dent Clin North Am 62: 121-130.
- Georgakopoulou E, Stebbing J, Scully C (2018) Targeted cancer therapies: Oral health care implications. J Am Dent Assoc 149: 100-111.
- Yuwanati M, Gondivkar S, Sarode SC, Gadbail A, Desai A, et al. (2021) Oral health-related quality of life in oral cancer patients: systematic review and meta-analysis. Future Oncol 17: 979-990.
- Epstein JB, Miaskowski C (2019) Oral Pain in the Cancer Patient. J Natl Cancer Inst Monogr 53.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Morittu S (2022) The Importance of a Preventive Oral Hygiene in Chemotherapy and Radiotherapy: A Case Report. J Oral Hyg Health 10: 325. DOI: 10.4172/2332-0702.1000325
Copyright: © 2022 Morittu S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2163
- [From(publication date): 0-2022 - Mar 14, 2025]
- Breakdown by view type
- HTML page views: 1850
- PDF downloads: 313