Research Article Open Access
The Impact of Treatment for Juveniles with Sexual Behavior Problems in Reducing Anxiety, Depression, and Cognitive Distortions
Aryssa Washington1, Lee A. Underwood1*, Mark Yarhouse1, Yolanda Crump2, Frances L.L. Dailey11Regent University, School of Psychology and Counseling, Virginia, USA
2Louisiana Office of Juvenile Justice, Los Angeles, USA
- Corresponding Author:
- Lee A. Underwood
Regent University, School of Psychology and Counseling, Virginia, USA
E-mail: leeunde@regent.edu
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
This study offers empirical evidence for the efficacy of the therapeutic treatment of juveniles with sexual behavior problems in secure-care facilities using the Louisiana Sex Offender Treatment Program (LSOTP), an integrated cognitive behavioral theory (CBT) approach. A quasiexperimental pre-test, post-test research design was implemented to examine the impact of LSOTP services among 33 adjudicated, male juveniles with sexual behavior problems in two secure-care facilities. All participants received LSOTP services and were measured for changes in depression, anxiety, and cognitive distortions (rape and molest) from Time 1 to Time 2. Results indicated that participants experienced (1) statistically significant reductions in anxiety level, and (2) measurably greater reductions in rape-related cognitive distortions. The LSOTP model of treatment used across Louisiana is related to psychosocial benefits. Recommendations are provided.
Keywords
Juveniles with sexual behavior problems, Secure-care facilities, Cognitive distortions, Anxiety, Depression, Hostility
Introduction
Juveniles with sexual behavior problems (JSBP’s) who commit sexual acts against another constitute a significant threat to public safety and welfare (Karakosta, 2015; Rehfuss et al., 2013). Juveniles adjudicated for sex offenses are often mandated to participate in treatment programming specifically addressing sexual behavior problems (Karakosta, 2015; Underwood & Knight, 2006). Juveniles with sexual behavior problems represent a special public concern for treatment providers in the community and juvenile justice administrators. Interventions for JSBPs tend to be based upon the goals of public safety and victim protection (Crump et al., 2013). In essence, the aim of treatment is often to reduce recidivism rates, or rates at which juveniles re-offend.
According to the Federal Bureau of Investigation, 14.3 percent of forcible rapes and 17 percent of other inappropriate sexual behavior perpetrated by youths under the age of 18 (Crump et al., 2013). It was estimated that 20 percent of sexual assaults and 30 to 50 percent of child molestations are committed by juveniles under the age of 18, according to a report in 2000 (Crump et al., 2013). Additionally, many adjudicated juveniles with sexual behavior problems admit to committing their first offense at approximately 12 to 15 years of age (Crump et al., 2013). Research has revealed that half of convicted adults with sexual behavior problems reported the initiation of their sexually abusive behaviors in adolescence (Underwood, Robinson, Mosholder, & Warren, 2008).
While much research is focused on the important goal of reducing recidivism rates of juvenile sex offending, Rehfuss et al. (2013) contends that few studies have measured the effectiveness of juvenile treatment programs in addressing the psychosocial needs relevant to characteristics consistent with juvenile with sexual behavior problems. Not only is the goal of treatment and rehabilitation to protect the community, it is also important to increase the quality of life and social skills of adjudicated juveniles with sexual behavior problems. Karakosta (2015) expressed that a failure to adequately examine treatment programs that address sexual behavior problems, as well as increase positive psychosocial changes, undervalues the juvenile justice system’s goal of rehabilitation. As such, prevention and intervention for JSBPs will benefit from validation of treatment protocols that measure psychosocial benefits among juveniles adjudicated for sexual behavior problems.
This is important because reoffending for sexual offenses tends to occur less often than nonsexual recidivism (Efta-Breitbach & Freeman, 2004). In fact, current research suggests that while most juveniles with sexual behavior problems will not repeat their sexual offenses, they may go on to commit other nonsexual criminal offenses (Efta-Breitbach & Freeman, 2004). The Indiana Department of Corrections conducted a three-year study of recidivism of juveniles with sexual behavior problems in 2010 (Schelle, 2010). Similar to previous data, the researchers found that juveniles with sexual behavior problems recidivated less often than other offenders. About three percent of juveniles with sexual behavior problems released in 2007 re-offended a sex offense. Further corroborating the literature, the study noted that 56% of the juveniles with sexual behavior problems attained new charges of nonsexual nature (Schelle, 2010). Therefore, evidence suggests that treatment for juveniles with sexual behavior problems should also aim to address overarching behavioral, cognitive, and emotional needs not necessarily related to the sexual crime. In order to attend to this goal, there are several critical factors that must be considered in serving juveniles with sexual behavior problems (JSBP’s), to include etiology, risk factors, and common characteristics of JSBPs.
Etiology and RiskOne contributing factor to sexual behavior problems is familial pathology (Geradin &Thibaut, 2004). Much of the literature purports that many JSBPs were also victims of or viewers of early physical and/or sexual abuse (Knight, 1990; Underwood et al., 2008). As statistics reveal that not all childhood victims become perpetrators, opinions vary regarding the impact of childhood victimization on adolescent sexual perpetration (Underwood et al., 2008). Hunter (2004) suggests that poor parental support, antisocial male-modeled behavior, and intrasexual and familial violence is somewhat related to the level of inappropriate sexual behavior exhibited by the juvenile with sexual behavior problems. Essentially, inappropriate sexual behavior stems, in part, from developmental and dysfunctional family behaviors (Hunter, 2004). When youth are exposed to male role models exhibiting antisocial behaviors, and sexually or physically violent behaviors towards females, they are more likely to develop inappropriate sexual behavior (Underwood et al., 2008).
Early childhood abuse has been noted as a risk factor for later offending behaviors (Boonmann et al., 2016). Others have similarly found that adverse childhood experiences were associated with increased likelihood of serious, violent, and chronic juvenile offending by approximately 35% (Fox et al., 2015). In their meta-analysis, Seto and Lalumiere (2010) revealed that prevalence for sexual abuse, physical abuse, and emotional abuse/neglect was over 35% for juvenile sex offenders. This occurrence was also evident more often in juveniles who sexually offend versus those who offend non-sexually (Seto & Lalumiere, 2010). DeLisi et al. (2017) examined a sample of 2520 confined, male JSBPs to evaluate the significance of adverse childhood experiences on offense type (homicide, sexual assault, and serious persons/property offending). Researchers found that adverse childhood experiences varied considerably across ethnicities and type of crime, but noted that adverse childhood experiences were strongly and positively associated with sexual offending. These findings suggest that JSBPs are generally more likely to have experienced some form of child abuse or an adverse childhood experience than non-sexual juvenile offenders. Furthermore, the greater the amount of childhood adversity and abuse experienced, the greater the likelihood of the youth to offend later in life, placing JSBPs at a greater risk. In terms of sexual violence, many researchers have discovered that various adverse childhood experiences, particularly childhood sexual abuse, increases the likelihood of committing sexual crimes in adolescence or later (Drury et al., 2017; Levenson et al. Looman, 2016; McCuish et al., 2017).
Not only are adverse experiences and trauma linked to later offending, extant literature has revealed that childhood abuse is also associated with increased mental health problems (Boonmann et al., 2016). Boonmann et al. (2016) examined a sample of 44 JSBPs in two juvenile detention centers in the Netherlands between 2008 and 2014. Youth were examined in order to explore the relationship between a history of childhood abuse and mental health problems in juveniles with sexual behavior problems. These researchers found that in their sample, sexual abuse was related to anger problems, suicidal ideation, and thought disturbance. These correlations were significantly stronger in JSBPs than in non-sexual juvenile offenders (Boonmann et al., 2016). This corroborates earlier claims that JSBPs who have a history of child abuse, may suffer from more salient internalizing and externalizing mental health problems.
Boonmann et al. (2015) expressed that there is a need for more studies regarding the relationship between JSBPs and mental health problems. Using the Massachusetts Youth Screening Instrument-Version 2 (MAYSI-2), Boonmann and colleagues (2015) found that young JSBPs were less likely to report anger-irritability or substance misuse, but convicted and detained young sex offenders expressed higher levels of mental health problems compared to non-sexually offending youth. While Seto and Lalumiere (2010) and Van Wijk and colleagues (2006) noted that JSBPs tended to have more internalizing problems (i.e., anxiety and depression), Boonmann et al. (2015) found that there were no differences in internalizing problems between JSBPs and non-sexually offending juveniles. Doreleijers (as cited in Boonmann et al., 2015) hypothesized that the prevalence of mental health problems in youth increases the further within the juvenile justice system they go, as the prevalence of Distortionsmental health problems appears to differ between juvenile arrestees, juveniles brought to court, juveniles assessed by the court, and incarcerated juveniles. This hypothesis in conjunction with findings on adverse childhood experiences would suggest that juveniles with sexual behavior problems in secure-care settings would exhibit a higher prevalence of mental health problems.
Characteristics of Juveniles with Sexual Behavior ProblemsIt has been found that many young offenders have high levels of mental health problems (Underwood & Washington, 2016), but there have also been some findings that indicate that JSBPs tend to have more internalizing problems, peer relationship problems, and higher rates of childhood sexual abuse (Seto & Lalumiere, 2010; Boonmann et al., 2015). Studies have also corroborated that JSBPs tend to express lower rates of alcohol problems, drug problems, and anti-social involvement (Boonmann et al., 2015). This is in contrast with older male offenders, who expressed more anger/irritability, substance use problems, and traumatic experiences (Cauffman, 2004). There are varying and even contradictory opinions with regards to factors that characterize juveniles with sexual behavior problems.
The pattern of greater mental health problems, behavioral problems, and interpersonal problems characteristic of JSBPs has some links with psychopathy. Psychopathy describes a pattern of deficits in interpersonal, emotional, and adaptive/behavioral functioning that can be directly related to understanding and explaining sex offending (Cale et al., 2015). Features such as deceit, manipulation, lack of empathic understanding, and consistent engagement in antisocial behaviors are all consistent with psychopathic traits and explanations of the coercion and aggression often used by juveniles with sexual behavior problems (Cale et al., 2015). In a sample of JSBPs and juvenile non-sex offenders, Cale and Colleagues (2015) found that JSBPs had significantly higher rates of psychopathy compared to violent, non-violent, and chronic juveniles with non-sexual behavior problems.
Some suggest that JSBPs are “opportunistic, manipulative, and pretentious having an inflated image of their abilities, insight, and knowledge” (Lakey as cited in Underwood et al., 2008, p. 919). Others describe JSBPs as lacking social communication skills and having limited impulse control, antisocial personality features, and having limited knowledge and experiences (Gardin&Thibaut, 2004; Underwood et al., 2008). Familial dysfunction often lends to JSBPs reporting feelings of worthlessness and fears of being rejected, and having underdeveloped social and coping skills compared to peers (Underwood et al., 2008). Extent literature suggests that JSBPs hold maladaptive value systems founded on faulty thought patterns, cognitive distortions, or thinking errors generally learned from interpersonal relationships (Apsche et al., 2004; Berenson & Underwood, 2001; Underwood et al., 2008). With regards to sexuality, JSBPs percepts or beliefs are often misinformed and he/she refuses to consider alternative information. Exposure to parental sexual pathology, sexual interactions of parents/surrogates, and pornography exposure are posited to create a maladaptive concept of appropriate sexual behavior which in turn may lead to exhibitions of offensive behaviors (Gardin&Thibaut, 2004; Underwood et al., 2008).
Additionally, a significant number of JSBPs lack the ability to empathize with their victims (Geradin &Thibaut, 2004; Hunter, 2004). In fact, some JSBPs may even hold the victims responsible for their actions (Underwood et al., 2008). The inappropriate sexual behavior often empowers the youth, making him/her feel as though he/she has dominion or control over the victim (Geradin &Thibaut, 2004). This emotional deficit and maladaptive concept is often indicative of some underlying mental health disorder. Much research has suggested that JSBPs do suffer from a significant range of mental health and substance use disorders (Apsche et al., 2004). In addition, JSBPs who have committed child molestation or rape, have a higher risk of recidivating for both sexual offenses and non-sexual crimes (e.g. vandalism, arson, theft; Harris et al., 2003; Underwood et al., 2008).
Trauma, childhood abuse, and adverse childhood experiences increases the possibility of youth externalizing their symptoms and engaging in various types of antisocial behavior. This possibility is even greater for juveniles with sexual behavior problems. Additionally, JSBPs tend to experience more internalizing problems, related to emotional problems, social deficits, and behavioral/adaptive problems. It may be even more problematic for JSBPs in residential or secure-care facilities. As such, these highlight the need for treatment programming to be able to address some of these underlying psychosocial factors.
Common InterventionsThe general tenets of juvenile justice administrators include rehabilitation, control, and custody. These emphases have led to the need to implement best-practice and evidence-based treatment interventions to juvenile offenders (Underwood and Knight, 2006). Estimates indicate that 50 to 70% of juvenile offenders have diagnosable mental health issues and may need services not merely specific to their offense (Teplin, Abram, & Washburn, 2013; Underwood and Knight, 2006; Underwood and Washington, 2016). In essence, JSBP’s present with other internalizing mental health problems not directly correlated with the sexual offense (i.e., depression or anxiety). Additionally, many incarcerated youth, including JSBPs, may have learning or intellectual disorders, or may have been exposed to adverse childhood experiences or significant traumatic events (Bailey et al., 2007; Boonmann et al., 2015; DeLisi et al., 2017). Finally, the interpersonal and behavioral deficits commonly associated with JSBPs, suggest that treatment must provide some development of prosocial skills.
An intervention program consisting of cognitive-behavioral interventions within a multisystemic (or integrated) approach carried out within an institutional setting, may best allow for justice to maintain its tenets of retribution, deterrence, and rehabilitation. A multisystemic treatment approach may include, individual, group, and or family therapy within various types of settings (residential or community). A mixture of these treatment modalities (to include individual, group, and family therapy) has been deemed an effective approach in addressing the various emotional, social, and behavioral needs of juveniles with sexual behavioral problems (Borduin et al., 2009; Letourneau et al., 2009; Rehfuss et al., 2013; Karakosta, 2015). Literature on the treatment of JSBPs indicates that cognitive behavioral models show the greatest effectiveness for offenders involved in multidimensional programs (Underwood and Knight, 2006). Additionally, a cognitive-behavioral framework allows for therapeutic facilitators to integrate multiple interventions that address various issues related to the juvenile offender’s ability to change (Underwood & Knight, 2006; Efta-Breitbach & Freeman, 2004; Rehfuss et al., 2013; Borduin et al., 2009; Karakosta, 2015).
The Integrated Sex Offender Treatment Program ModelThe Louisiana Office of Juvenile Justice (OJJ) recognized in 2008 that there was no standard level of care or collaboration on the best-practice treatment of JSBPs within the legal system (Crump et al., 2013). The Louisiana OJJ found that JSBPs received inconsistent or confusing care, and that youth may have spent much time in secure-care when a less restrictive setting would have been optimal (Crump et al., 2013). Additionally, due to community care limitations, the continuity of care for JSBPs was often inadequate (Crump et al., 2013). In efforts to carry out the mission of effective care and limited harm, the OJJ has reserved secure-care for youth with a greater risk of reoffending, and community-care for youth who pose a lesser risk (Crump et al., 2013). In 2008, the Louisiana OJJ received a grant award to address concerns related to assessment, placement, and treatment of adjudicates JSBPs (Crump et al., 2013).
As a result, a modified comprehensive integrated treatment Program—Louisiana Sex Offender Treatment Program (LSOTP)—for juveniles adjudicated for sexual offenses in Louisiana was developed. Juveniles in secure-care receive comprehensive psychosexual assessments, and those with lower risk levels receive treatment in a clinic-based format (i.e., they are placed in general population dorms with juveniles adjudicated for non-sexual offenses). Individual and group therapy is provided to JSBPs one to two times weekly and family therapy is provided monthly (Crump et al., 2013). Higher risks JSBPs receive individual, group and family therapy with more intensity, frequency, and duration. Group therapy is conducted in three phases of 12 to 16 weeks each. The Louisiana Sex Offender Treatment Program (LSOTP) consists of four stages of care that address, social skills, impulse control, healthy sexuality/relationships, masculinity, anger management, empathic understanding, relapse prevention, and aftercare.
This program is a multi-faceted treatment process that takes the youth through an initial phase of screening and assessment, through behavioral health treatment interventions, leading to admission for successful discharge from the program. Behavioral health treatment interventions utilized within the program include (1) individual counseling and case management, (2) family interventions, and (3) crisis intervention services. Individual counseling targets individual behavioral deficits, distortions, and developmental needs and fosters the skills required by individual residents to manage and cope with different persons, places, and situations. Individual case management helps map out individual responses in crisis situations, reinforces the use of behavioral management skills and addresses other needs that are not appropriate for group skills training. Family interventions are designed to engage family members or legal guardians in the treatment process. Mental health providers inform the resident’s family about placement in the program and encourage participation in the treatment process in person or via telephonic conference. Crisis intervention services are also available on a continuous basis to any youth who is experiencing acute distress. The program was designed to enhance recognition of appropriate sexual boundaries and bolster emotional stability and self-control, addressing the various problem areas relevant to juveniles with sexual behavior problems.
Purpose of the StudyThis study examined whether juveniles with sexual behavior problems receiving LSOTP services at two secure-care facilities experienced positive changes in psychosocial factors over time. This study is the initial portion of a larger longitudinal study and the purpose of this study is to determine if there are significant positive changes in juvenile’s reported levels of anxiety, depression, and cognitive distortions after receiving 13 weeks of LSOTP services. This was done in order to track the longitudinal impact of receiving LSOTP services and provide guidance for future studies with the Louisiana Sex Offender Treatment Program. Specifically, it was hypothesized that juveniles with sexual behavior problems involved in LSOT programming would: (1) Experience a decrease in reported depression symptoms from Time 1 to Time 2, (2) Experience a decrease in reported anxiety symptoms from Time 1 to Time 2, and (3) Experience decreased cognitive distortions related to rape and molestation.
Methodology
The research method used is a quasi-experimental time series design (pretest/ posttest design without a baseline) and employed Dependent-Samples T-tests to examine differences in means scores from a group of juveniles with sexual behavior problems in LSOT programming at two southeastern states in the United States.
Participants
The sample in the study was provided by Louisiana’s Office of Juvenile Justice (OJJ) treatment program for JSBPs at two satellite secure-care facilities. The rationale for this research design is based on the nature of the data and the setting. Several years ago, Louisiana Office of Juvenile Justices moved that all treatment programs utilize this same integrated treatment program. As such, it was not possible to have a manipulated treatment group. Additionally, all adjudicated JSBPs receive services in secure-care settings, unless the youth refuses to participate, services were deemed unnecessary, or the youth was removed from treatment (i.e., termed the “refusal” group). At the time of this study, the refusal group was small (n=1). The current study represents the initial part of a longitudinal study examining psychosocial changes in JSBP’s spanning October 2014 to February of 2016.
Participants in this study were recruited from a convenience sample of 55 adjudicated male JSBPs between the ages of 12 and 19 years of age residing at two secure care facilities in southeastern USA. Prior to the initial site visit, guardian consent for each youth to participate in the study was obtained by the facility. Upon the initial site visit, the purpose of the study, activities involved in participation, and the voluntariness of participation was described to all adjudicated youth at both sites in groups of 5 to 10 youth. At that time youth gave assent to participate in writing, but were reminded that they could discontinue participating in the study at any time. For inclusion in this study, the participant must have signed consent and assent forms, must have been 19 years old or younger, mandated to participate in treatment, be adjudicated for a sexual offense, and complete assessment measures for both Time 1 and Time 2.
The sample was initially comprised of 52 adolescent males, as 3 chose not to participate. An additional 19 youth were removed from analysis as they did not participate in testing at Time 2. As such, the participant sample in this study consisted of 33 adolescent males, 8 (24%) receiving treatment for sexual behavior problems in a rural, northern Louisiana secure-care facility and 25 (75%) receiving treatment for sexual behavior problems in a southeastern Louisiana. While the sample size is considered small, it is reflective of other quasi-experimental designs with juvenile sex offenders. Karakosta (2015), Boonmann et al. (2016), Borduin, Schaffer, and Heiblum (2009), Borduin et al. (1990) conducted analyses with sample sizes of less than 50 juveniles with sexual behavior problems.
Adolescents in this study self-identified as, European American (33%), African American (42%), Multi-ethnic (9%), Hispanic American (6%), Native American (6%), and Other (3%). Ages of youth in the sample ranged from 13 years old to 19 years old, with most between the ages of 15 and 18 years (87%). Grade level ranged from 6th to 12th grade. Approximately 17 (51%) had not been treated before for a sex offense, while 15 (46%) had received some form of sex offender treatment. For 90% of the sample, this is the first time they have been adjudicated for a sex crime, however, 45% reported having been treated for sexual behavior problems in the past. At the time of assessment, four distinct groups of youth emerged based on the amount of time they have spent in the treatment program. Approximately 9 (27%) of the youth have been in LSOTP for 0-3 months, 6 (18%) have been in treatment for 4-6 months, 5 (15%) have been receiving treatment for 7-9 months, and 13 (39%) have been receiving LSOTP services for 9+ months.
Data Collection
A Human Services Review Committee was reviewed and approved this study, ensuring for safeguards and human protection factors. Prior to the initial site visit, the Louisiana OJJ sought and provided consent for youth to participate in the current study should he choose to do so. Upon the initial site visit, the researchers provided adjudicated JSBPs at both sites with an introduction to the research purpose and activities related to involvement. Participants were informed that regardless of their involvement, they would continue to receive LSOTP services. Youth were also assured that they were not required to participate in the study, that participation was strictly voluntary, and that they were able to discontinue participation at any time throughout the study. Participants were informed that each individual would be assessed via several self-report measures at 12 to 13 week intervals. Youth were also assured that strict confidentiality would be maintained throughout the study by use of a numerical coding system. After asking and answering any follow up questions, written assent was obtained from those volunteering to participate in the study.
Before the initial site visit, the researchers reviewed the demographic questionnaire (pre-test only), Children’s Depression Inventory-2 (CDI-2), Revised Children’s Manifest Anxiety Scale-2 (RCMAS-2), Bumby Cognitive Distortions Rape Scale (BCDR), and the Bumby Cognitive Distortions Moles Scale (BCDM) with test administrators (graduate level research students) to discuss any questions that may arise and demonstrate the order in which assessments were to be administered. All team members were instructed on how to describe informed assent, and they were instructed to collect all assent forms from all participants before proceeding with assessment. Juveniles with significant learning, cognitive, or attention deficits were identified by group case workers, and they were provided a separate space for more one-to-one help with a research team member. Assessment administrations occurred within one day per site. Post-test administration took place approximately 13 weeks later, following the same protocol. Each youth was assigned a number code to use instead of identifying information (a master list of names and associated codes was maintained by the principle investigator). After the assessment period, each site was provided with money to provide youth with pizza and soda as a participation incentive.
Instruments
The measures employed in this study include a demographic questionnaire administered to participants at the facility from whom consent has been obtained voluntarily from both the participant and their parent/legal guardian and four inventories that are the dependent variables in this study. The measures were handed out in hard-copy form and participants were asked to respond to all items on the testing instruments to ensure validity of the comparative results. These measures are described briefly:
Demographic Questionnaire
Participants were asked to fill out a demographic questionnaire upon agreeing to participate in the program. Items on this measure were generated by the research team. Questions regarding age, race/ethnicity, level of education completed, and history of confinement. See Appendix A for a sample of the demographic questionnaire administered.
Children’s Depression Inventory 2 (CDI-2)
The CDI 2 is a revised version of the Children’s Depression Inventory. The revisions include additional assessment tools that focus on core features of childhood depression and normative data representative of U.S. populations. The Children’s Depression Inventory 2 (CDI 2) assesses depressive symptoms in 7- to 17-year-old children and adolescents. Evolving from the original CDI and formally published in 1992, the CDI 2 was designed for youth to respond to the scales with three choices per item and items written at a low reading level. This, as with all other inventories was administered and scored in a paper and pencil format.
Historically, all CDI 2 forms showed high or acceptable levels of internal consistency with the Cronbach’s alpha values from 0.67 to 0.91 for total and all subscales for all age and sex groups. Also, since the CDI 2 purports to estimate temporary attributes (i.e., state) rather than stable attributes (i.e., trait; Hong & O’Neil, 2001), test-retest reliability of the self-report forms was tested for 79 children (53.2% male, mean age=12.06 years, SD=2.92 years) within a 2- to 4-week interval (M=16.1 days). The results revealed excellent short-term stability with nearly no change during the time interval. The construct validity of CDI 2: SR was analyzed through a hierarchical third order 1 CFA model—the model fit was very good with the CFA indexes: NFI=.95, NNFI=.94, CFI=.96 and RMSEA=.07.
The Revised Children’s Manifest Anxiety Scale (RCMAS-2)
The Revised Children’s Manifest Anxiety Scale (RCMAS) is a self-reporting instrument designed to gather and rate the nature of anxiety experienced by respondents (Reynolds & Richmond, 1985). Designed for children, questions are dichotomous “yes/no” items. A “yes” response indicates that the item in question describes the respondents feeling and actions. A “no” response indicates that the item is generally not descriptive of the respondent’s feelings and actions. A total anxiety score is calculated from the 28 items divided into three subscales measuring (1) physiological anxiety (such as sleep difficulties, fatigue, and nausea), (2) worry and over-sensitivity (such as obsessive concerns about having one’s feelings hurt or feeling emotionally isolated), and (3) social concerns related to interpersonal relations and levels of concentration.
Internal consistency reliability for the RCMAS-2 indicates the scale has alpha estimates that are adequate. Coefficient alpha estimates ranged from 0.92 (Total Anxiety) to 0.75 (Physiological Anxiety) for the full reference sample (N=3,086). Similar coefficient alpha reliabilities were found across different gender, age, and ethnic groups. The test authors reported adequate alpha estimates ranging from 0.92 (Total Anxiety) to 0.70 (Physiological Anxiety) in a clinical sample of children with one of the following disorders: attention deficit disorder (n=57), autism spectrum disorders (n=36), anxiety disorders (n=32), depression (n=101), oppositional defiant disorder (n=42), conduct disorder (n=73). Evidence of test-retest reliability of the scales was obtained from a sample of 100 school children, who completed the RCMAS-2 on two occasions with a one-week delay. The highest test-retest correlation was for the Total Anxiety scale (.76) and the lowest test-retest correlation was for the Short Form Total Anxiety scale (.54; Reynolds & Richmond, 1978; 1985).
Bumby Cognitive Distortions Scale (BCDS)
The use of a cognitive distortions scale reflects the realization that cognitive and perceptual distortions are critical elements in the assessment and treatment of sexual offenders. Several scales have been created to identify and measure cognitive distortions, specifically the MOLEST and RAPE Scale of the Bumby Cognitive Distortions Scale. The basic premise that underlies the use of these types of scales is that perpetrators often have distorted perceptions regarding themselves, their sexuality, their relationships to others (especially regarding their relationships as men toward women), and the nature and severity of sexual aggression and sexual contact.
The Bumby RAPE Scale, a self-report instrument wherein respondents rate their agreement to 36 statements reflecting attitudes toward women. Overall, the Bumby RAPE Scale scores have demonstrated good reliability and validity with adult populations. Each item of the Bumby RAPE Scale had an item-to-total correlation greater than 0.30 with a mean score of 0.65. Cronbach’s alpha was 0.96 in Bumby’s (1996) evaluation and was 0.95 in the Robinson, Shaver, &Wrightsman (1991) study. In addition, Bumby (1996) found that the test-retest correlation was good (r=0.86) across a 2-week interval. Validity was assessed by correlating the Bumby RAPE Scale with the Cognitive Distortions/Immaturity (r=.33, p<0.05) and Justification (r=0.34, p<0.05) scales of the Multiphasic Sex Inventory (Robinson et al., 1991). The correlations were low to moderate, providing some evidence of convergent validity. Furthermore, the Bumby RAPE Scale was not significantly related to measures of socially desirable responding in Bumby’s study (r= –0.02, p>0.05) or the 1991 study (r=0.04, p>0.05), suggesting that socially desirable responding is not an issue. Moreover, the application of a cognitive distortions scale among juveniles with sexual behavior problems may be less prone to misleading or deceptive responses since juveniles may be less keenly aware of what kinds of responses would be socially desirable, thus making the use of self-reporting instruments such as these scales among juveniles acceptably valid measures.
Using some items derived from the ABCS, Bumby (1996) set about developing a questionnaire measurement of Child molesters' cognitive distortions more robust to socially desirability bias. The resultant MOLEST scale contained 38 items rated using a 4-point Likert scale, had improved psychometric properties in comparison to the ABCS (α=0.97; test–retest reliability over two weeks=0.84), and was not significantly correlated with socially desirable responding (measured using the Marlow–Crowne Social Desirability Scale; Crowne & Marlowe, 1960). Increased MOLEST scale endorsements were significantly correlated with number of victims in offenders' offense histories. In terms of discriminative ability, Bumby (1996) reported that Child molester made significantly higher endorsements of cognitive distortions on the MOLEST scale. The Bumby scales were normed on adult sex offenders, but research has indicated its use with adolescents in treatment or clinical settings (Bumby, 1996; Beech et al., 2003). As there is limited research regarding the Bumby scales utility in measuring adolescent cognitive distortions, the current study hopes to add statistical information regarding its use with adolescent sex offenders.
Research Design and Statistical Analysis
The current study utilized a quantitative, quasi-experimental time series (pre-test/post-test design without a baseline) design. The independent factor in this study is Time (Time 1 and Time 2). Dependent variables included scores on depression, anxiety, rape-related cognitive distortions, and molestation-related cognitive distortions. The method of statistical analysis conducted was a dependent-samples t-test for each dependent variable. Dependent-samples t-tests were used to examine the differences in mean scores on dependent measures at Time 1 compared to mean scores on dependent measures 13 weeks later at Time 2.
Results
A Dependent-Samples T-test was conducted to compare the difference in mean scores on psychosocial measures of anxiety, depression, and cognitive distortions after participants had received 13 weeks of LSOTP services. Table 1 provides a summary of Dependent-Samples t-test results.
| Variables | Time 1 | Time 2 | 95% CI for Mean Difference | r | t | df | |||
|---|---|---|---|---|---|---|---|---|---|
| Outcome | M | SD | M | SD | n | ||||
| Depression | 53.03 | 10.9 | 52.2 | 11.28 | 33 | -1.96, 3.60 | 0.75 | 0.6 | 32 |
| Anxiety | 48.63 | 10.8 | 45.8 | 10.71 | 32 | 0.124, 5.37 | 0.77 | 2.14* | 31 |
| Molest | 62.13 | 14.1 | 57.3 | 15.89 | 33 | -1.0, 10.60 | 0.41 | 0.1 | 32 |
| Rape | 65.75 | 14.5 | 58.5 | 14 | 33 | 1.67, 12.77 | 0.4 | 2.65* | 32 |
| *p<0.05 | |||||||||
Table 1: Descriptive statistics and t-test results for depression, anxiety, and cognitive distortions
Data Screening/Diagnostics
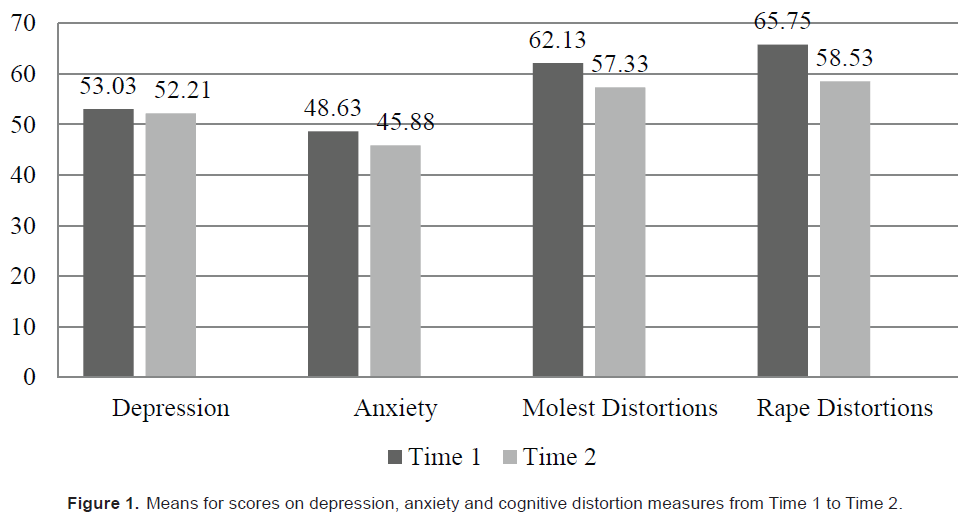
Originally, the study consisted of 52 participants; however, 19 cases were removed from analysis due to non-completion of post-test assessments. The remaining 33 cases were assessed for missing value patterns using Little’s Missing Completely at Random (MCAR) test. The Little’s MCAR test obtained for this study’s data resulted in a chi-square=.000 (df= 2663; p<1.0), which indicates that the data is indeed missing at random (i.e., no patterns to missing values). Using the Multiple Imputation Analyze Pattern function in SPSS, complete versus incomplete data were analyzed for variables and amount missing. Overall, 19 variables (9.86%) were missing 1-3 values each, resulting in 27 total missing values. Additionally, approximately 48% (n=16) of individuals were missing at least one item-response on a measure. As no individual exhibited a pattern to their missing values, missing values were replaced by calculating scale scores using the case-wise mean. Replacing the values, as opposed to deletion was preferred due to the small sample size and the intention of conducting inferential statistics. Using case-wise mean values to derive total scale scores was preferred to multiple imputation, estimation maximization, or series means, as most individuals were only missing 1 to 3 values randomly. In this case, an assessment of how the individual was responding to items was used to estimate the mean for those missing less than 3 item responses. Calculated scale scores for each individual on the three dependent variables for pre-and post-measures were utilized in the analyses of this data. Figure 1 depicts differences in mean scores from Time 1 to Time 2 for each dependent variable (see Appendix A).
Dependent-Samples t-tests indicated that there was no significant difference in depression scores from Time 1(M =53.03, SD=10.91) to Time 2 (M=52.21, SD=11.28); t(32)=.599, p=0.554, d =0.105. Thus, Hypothesis one was not supported. Essentially, participants did not report experiencing a measurably significant reduction in depression symptoms after receiving LSOTP services for 13 weeks.
There was a significant difference in anxiety scores from Time 1(M=48.63, SD=10.89) to Time 2 (M=45.88, SD=10.71), t(31)=2.136, p<0.05. Effect size was corrected for dependence between means using Morris and Deshon’s (2002) equation 8, and the magnitude of the difference is considered small (d=.378). This result indicates that participants reported experiencing less anxiety after receiving 13 weeks of LSOTP services. Thus, Hypothesis two was supported.
Participants mean scores on molestation-related cognitive distortions were not significantly different Time 1 (M=62.13, SD=14.16) to Time 2 (M=57.33, SD=15.89), t(32)=1.684, p =.102, d=0.294. Effect size was corrected for dependence between means using Morris and Deshon’s (2002) equation 8. Participants cognitive distortions about molestation did not seem to differ after 13 weeks of being in the LSOT program. As such, part of Hypothesis three was not supported.
In contrast, participants mean cognitive distortions regarding rape were significantly lower from Time 1 (M=65.75, SD=14.59) to Time 2 (M=58.53, SD=14.00), t(32)=2.653, p<0.05. Effect size was corrected for dependence between means using Morris and Deshon’s (2002) equation 8, and the magnitude of the difference is considered small to medium (d =0.462). After receiving 13 weeks of LSOTP services, participant’s rape-related cognitive distortions appeared to decrease. Thus, Hypothesis three was partially supported.
Discussion
This study examined the changes in psychosocial factors over time for JSBPs receiving LSOTP services at two secure-care facilities. As the initial portion of a larger longitudinal study, the purpose of this study was to determine whether JSBP’s in the LSOTP program experienced measurable changes in their reported levels of anxiety, depression, and cognitive distortions related to rape and molestation after 13 weeks of treatment. This was done to also provide insight on the impact of the integrated treatment program on psychosocial factors. Specifically, it was hypothesized that participants would experience a decrease in reported depression, anxiety and cognitive distortions from Time 1 to Time 2.
Prior research indicates that JSBPs often exhibit greater internalizing problems and non-serious mental illnesses such as anxiety and depression. The current study predicted that after 13 weeks in LSOT programming, JSBPs would experience measurable symptom relief related to depression and anxiety. While juveniles did not appear to experience significant changes in depression, their anxiety levels did decrease after 13 weeks of receiving LSOTP services. Boonmann et al. (2015) noted that the prevalence of mental health problems among juvenile offenders often differs depending on the youth’s phase within the judicial process. It may be that depressive symptoms were less relevant to this sample than were symptoms related to anxiety. The finding does support that JSBPs likely do experience some internalizing mental health problems, and that this integrated approach can potentially address anxiety related issues. Evaluating the same treatment program in a different state, with JSBPs in a residential setting, Karakosta (2015) did not observe statistically significant reductions in depression or anxiety, while the current study did observe significant reductions in anxiety among JSBPs in secure-care facilities. The difference in findings may reflect fundamental differences in JSBPs receiving integrated treatment within different secure-care facilities. As such, future exploration of said differences would add information to the field and treatment needs of juveniles with sexual behavior problems.
The third hypotheses predicted that JSBPs receiving LSOTP services would experience decreases in cognitive distortions after 13 weeks of treatment. The cognitive-behavioral framework of integrated treatment programs is often helpful in addressing distorted or faulty thinking. The findings in this study partially corroborate this notion, as youth experienced significant decreases in rape-related distortions, but not distortions related to molestation. Karakosta (2015) also observed statistically significant reductions in rape-related cognitive distortions. These findings partially confer with the findings of Karakosta (2015) and Rehfuss et al. (2013) who reported that an integrated treatment approach, such as LSOTP services, significantly increased JSBPs abilities to analyze cognitive distortions. In contrast with the current study, Karakosta (2015) also found that molestation-related cognitive distortions were significantly reduced.
In general, JSBPs receiving LSOTP services at the two secure-care facilities, did experience partial positive changes in psychosocial factors. This provides some evidence that youth in secure-care receiving LSOTP services are experiencing some psychosocial benefits relevant to juveniles. The significant reductions in rape-related cognitive distortions and anxiety symptoms lend support to the utility of LSOTP with JSBPs in secure-care facilities. These positive findings are reflective of treatment models such as the Good Life Model, the Good Enough Lives Model, and the Risk-Need Responsivity Model (Boer, 2013; Looman &Abracen, 2013). These program models, much like LSOTP, promote a multi-systemic treatment approach created to reduce recidivism, prevent sexually aggressive behaviors, while also increasing the psycho-social wellbeing of individuals with sexually maladaptive behaviors (Boer, 2013; Karakosta, 2015). The results of the study reinforced the theoretical underpinnings promoting an integrated design to therapeutic treatment in that there were significant reductions in cognitive distortions as well as improvements in anxiety levels over time in the treatment program.
Limitations and Future Research
A limitation of the study is the lack of a non-treatment or comparison group, which would enable the generalizability of the present results. However, the partial findings in the current study are similar to the partial findings in Karakosta’s study (2015) of the same integrated model. The findings do suggest that individuals participating in the LSOT program at the secure-care facilities in Louisiana do appear to be experiencing some psychosocial benefits.
The nature of the dependent-samples design used in this study raise concerns about internal validity related to history effects and a non-randomized sample. An issue relevant to history effects at one site was a change in program director and delayed incentive. Youth reactions and responding at Time 2 was likely impacted by changes to programming staff and to the fact that they did not receive their participation incentive for Time 1 until after Time 2.
Another threat to internal validity is the fact that the sample was more of convenience than randomized, and there was no comparison group since JSBPs within governed secure-care facilities must be provided treatment. There are some individuals who refused to complete programming or are removed/not allowed to participate in LSOTP services, which may make for a helpful comparison group for future research. At the time of initial assessment, however, there was only 1 individual who was identified as “refusal.” Future studies should include a comparison group of participants who do not receive treatment or who receive a different type of treatment. This would allow for changes in outcomes to be indicative of the treatment modality the participants are exposed to. Again, this would increase the generalizability of the research findings. It would be more informative to track changes in a more longitudinal format that also assessed for patterns to changes on outcome measures based on the length of time in treatment. It would be valuable to evaluate at what point in time in the treatment program are which psychological factors more prone to change. Another recommended study would be to evaluate the differences in LSOTP services provided to JSBPs in secure-care facilities, versus those receiving services in residential treatment facilities and community settings.
Due to the size of the sample and limits to the strength of Power, a less ideal statistical analysis of comparing means was chosen—a paired-samples t-test. This analyses was, however, appropriate, and all testing assumptions were met, lending to the strength of the study’s design and analysis. Additionally, the size of the current study’s sample is reflective of the sample size of similar studies (Boonmann et al., 2016; Karkosta, 2015). Due to the fact that participants had received varying amounts of treatment (0-9months), and Boonmann and colleague’s notion that stage in the system relates to degree of internalizing problems, future studies would benefit from examining associated group patterns.
Although the sample in the current study is considered small, it was diverse in age and ethnicity. Most previous studies comparing mental health problems between young JSBPs and other offenders may have been confounded because they did not allow for demographic differences related to status in the juvenile justice system, age, and ethnicity (Boonmann et al., 2015), which represents somewhat of a strength for the current study. Cuellar et al. (2006) suggests that an updated study that controls for phase in the judicial system, would contribute to our understanding of mental health problems among JSBPs and the intervention needs present. Future studies that examine the anxiety, depression, and cognitive distortions of JSBPs at different phases within the judicial process would also provide information to the field on juvenile sex offending.
Another recommendation for future research is to further evaluate the validity and reliability of the use of Bumby Cognitive Distortion Scales with youth in secure-care facilities. This study achieved demonstrable success using the Bumby Rape Scale even though it was designed specifically for adults and is commonly used in clinical treatment settings with youth offenders. The limited success with the Bumby Rape Scale, along with observed comprehension and attentional difficulties, indicate that some attention to the applicability with this population should be explored in future studies.
As a complement to the quantitative analyses being conducted on the impact of LSOTP services in secure-care facilities, a more qualitative study design is recommended. Aphenomenological-qualitative design would provide an opportunity to explore meaningful experiential information that focuses on participants’ experiences and their interpretation of their experiences while receiving LSOTP services. A study as such, would explore the relationship between noted experiences and family, medical, personal, and criminal histories. Thus, the obtained information would provide meaningful interpretation of the individuals receiving LSOTP services in a secure-care setting.
Implications
Given the variety of theoretical approaches to treatment interventions for JSBPs and the various treatment options available to practitioners, the need for empirical evidence supporting the efficacy of such treatments is apparent. This study offers some empirical evidence for the efficacy of LSOTP services across time in the state of Louisiana, specifically in the management of anxiety and rape-related cognitive distortions relevant to youth with sexual behavior problems. As such, the first implication of this study for treatment providers is to support the validity of LSOTP services as a relevant treatment approach for anxiety and rape-related cognitive distortions in Louisiana secure-care facilities.
There is a wide spectrum of sexual offense charges, from Lewd and Lascivious Conduct, to more serious charges of Rape. Additionally, for JSBPs in secure-care, their criminal charges may consist of a clear sexual assault or be accompanied by crimes in other areas. Awareness of the nature of charges when providing treatment with JSBPs would be helpful. The nature of the charges likely suggests some differences in psychological profile, risk factors, and demographic influences. It is also important to note that the exhibited sexual behaviors may differ from the charges the youth was adjudicated for. Some juveniles may have committed more heinous crimes, than reflected by the actual charges due to the plea-bargaining process. Additionally, secure-care facilities are the most restrictive environment and often a last choice, thus providers may want to account for historical sexual behaviors that may exist with youth. As mentioned by Karakosta (2015), treatment providers need to be aware that youth conduct may be divergent from actual legal charges.
Of grave importance, is the need for providers to understand the difference between maladaptive sexual and criminal behaviors that are sexually problematic in nature. Essentially, treatment providers should be able to differentiate between sexual behaviors that are merely maladaptive and deviate from social norms, versus those that are violations of the law. This consideration is implicative for treatment planning and issues related to governing ethics.
A final implication of this study is that factors such as depression and anxiety have been linked to JSBPs and those who commit sex crimes. These psychological factors may not be causally connected, or may only be partially related. For example, this study found anxiety was relevant to this sample of JSBPs, but depression may not have been. Additionally, the secure-care setting can often be anxiety-provoking and depending on length of time in the environment or exposure to restrictive environments as such juveniles in secure facilities may in general exhibit heightened levels of anxiety. Regardless of treatment training, providers should be able to identify symptoms of anxiety and depression so appropriate and timely services can be provided. Essentially, individuals providing treatment to JSBPs in secure-care facilities should have adequate training to accurately diagnose mental health conditions or accurately identify problematic psychological factors underlying the juvenile’s condition.
Conclusion
The results of the study provide reasonable support for the integrated approach offered through the LSOTP in the treatment of juvenile sex offenders with anxiety and rape-related cogntive distortions. This study demonstrates that sexually maladaptive behaviors based on rape-related cognitive distortions are amenable to improvements and accompanying heightened anxiety is amenable to reduction for juvenile sex offenders within the LSOT program. The observations made via this research study contributes to the growing body of empirical evidence supporting the use of integrated, multisystemic treatment approach to address some of the psychosocial needs of juveniles with sexual behavior problems. The measures used in the study indicate, with a small to medium effect size, that juvenile sex offenders receiving LSOTP services in secure-care facilities experience improvements in anxiety level and cognitive distortions related to rape. This research supports the use of LSOTP services with juvenile sex offenders in secure-care facilities to bring about significant improvements in intrapersonal and interpersonal factors consisted with maladaptive sexual behaviors, to include perceptual misconceptions and anxiety.
References
- Apsche, J.A., Evile, M.M., & Murphy, C. (2004). The thought change system an empirically based cognitive behavioral therapy for male adolescent sex offenders. The Behavior Analyst Today, 5(1), 101-107
- Bailey, S., Whittle, N., Farnworth, P. &Smedley, K. (2007), A developmental approach to violence, hostile attributions, and paranoid thinking in adolescence.Behavioral Science &The Law, 25: 913–929
- Berenson, D. & Underwood, L.A. (2001). A resource guide: Sex offender programming in youth correction and detention centers. Council For Juvenile Correctional Administrators (CJCA) & The Federal Office of Juvenile Justice Delinquency Prevention (OJJDP):Washington, D.C
- Boer, D.P. (2013). Some essential environmental ingredients for sex offender reintegration.International Journal of Behavioral Consultation and Therapy, 8(3), 8-11
- Boonmann, C., Nelson, R., Dicataldo, F., Jansen, L., Doreleijers, T., Vermeiren, R. et al. (2015). Mental health problems in young male offenders with and without sex offences: a comparison based on the MAYSI-2.Criminal Behaviour and Mental Health
- Boonmann, C., Grisso, T., Guy, L.S., Colins, O.F., Mulder, E.A., Vahl, P., et al. (2016). Childhood traumatic experiences and mental health problems in sexually offending and non-sexually offending juveniles.Child and Adolescent Psychiatry and Mental Health, 10, 45
- Borduin, C.M., Schaeffer, C.M., &Heiblum, N. (2009). A randomized clinical trial of multi-systemic therapy with juvenile sexual offenders: Effects on youth social ecology and criminal activity.Journal of Consulting and Clinical Psychology, 77, 26–37
- Bumby, K.M. (1996). Assessing the cognitive distortions of child molesters and rapists: Development and validation of the molest and rape scales. Sexual Abuse: A Journal of Research and Treatment, 8, 37-54
- Cale, J., Lussier, P., McCuish, E., &Corrado, R. (2015). The prevalence of psychopathic personality disturbances among incarcerated youth: Comparing serious, chronic, violent and sex offenders. Journal of Criminal Justice, 43, 337–344
- Cauffman, E. (2004).A statewide screening of mental health symptoms among juvenile offenders in detention.Journal of the American Academy of Child and Adolescent Psychiatry, 43, 430-439
- Crump, Y., Underwood, L.A., & Dailey, F.L. (2013). Louisiana office of juvenile justice’s comprehensive statewide approach to treating juveniles with sexual behavior problems.Corrections Today (September/October), 60-84
- Cuellar A.E., McReynolds, L.S., Wasserman, G.A. (2006). A cure for crime: Can mental health treatment diversion reduce crime among youth? Journal of Policy Analysis and Management, 25, 197-214
- DeLisi, M., Alcala, J., Kusow, A., Hochstetler, A., Heirigs, M., Caudill, J., et al. (2017). Adverse childhood experiences, commitment offense, and race/ethnicity: Are the effects crime-,race-, and ethnicity-specific? International Journal of Environmental Research and Public Health, 14, 331-342
- DeLisi, M., Kosloski, A.E., Vaughn, M.G., Caudill, J.W., &Trulson, C.R. (2014). Does childhood sexual abuse victimization translate into juvenile sexual offending? New Evidence. Violence and Victims, 29, 620–635
- Drury, A.J., Heinrichs, T., Elbert, M.J., Tahja, K.N., De-Lisi, M., &Caropreso, D.E. (2017). Adverse childhood experiences, paraphilias, and serious criminal violence among federal sex offenders. Journal of Criminal Psychology
- Efta-Breitbach, J., &Freeman, K.A. (2004) Recidivism and resilience in juvenile sexual offenders: An analysis of the literature. Journal of Child Sexual Abuse, 13, 257–279
- Fox, B.H., Perez, N., Cass, E., Baglivio, M.T., & Epps, N. (2015). Trauma changes everything: Examining the relationship between adverse childhood experiences and serious, violent, and chronic juvenile offenders. Child Abuse & Neglect, 46, 163–173
- Geradin, P. &Thibaut, F. (2004).Epidemiology and treatment of juvenile sexual offending.Pediatric Drugs Journal, 6(2), 79-91
- Harris, G.T., Rice, M.E., Quinsey, V.L., Lalumiere, M.L., Boer, D., & Lang, C. (2003). A multisite comparison of actuarial risk instruments for sex offenders. Psychological Assessment, 15(3), 413−425
- Hunter, J.A. (2004). Developmental pathways in youth sexual aggression and delinquency: risk factors and mediators. Journal of Family Violence, 19(4), 233−242
- Karakosta, O. (2015). The effectiveness of the ISOTP with juvenile sex offenders in residential care.Available from Dissertations & Theses @ Regent University; ProQuest Dissertations & Theses Global
- Knight, C. (1990).Use of support groups with adult female survivors of child sexual abuse.Social Work, 35(3), 202−206
- Letourneau, E.J., Henggeler, S.W., Borduin, C.M., Schewe, P.A., McCart, M.R., Chapman, J.E., et al. (2009). Multisystemic Therapy for Juvenile Sexual Offenders: 1-Year Results from a Randomized Effectiveness Trial. Journal of Family Psychology : JFP : Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 23(1), 89–102
- Levenson, J.S., Willis, G.M. & Prescott, D.S. (2016). Adverse childhood experiences in the lives of male sex offenders: Implications for trauma-informed care. Sexual Abuse,28, 340–359
- Looman, J. &Abracen, J. (2013). The Static-99R: Are there really differencesbetween normative groups? International Journal of Offender Therapy andComparative Criminology, 57 (7)
- McCuish, E., Lussier, P., &Corrado, R. (2016). Criminal careers of juvenile sex and nonsex offenders: Evidence from a prospective longitudinal study. Youth Violence and Juvenile Justice, 14, 199–224
- Morris, S. &DeShon, R. (2002). Combining effect size estimates in meta analysis with repeated measures and independent-groups design. Psychological Methods, 7, 105-125
- Rehfuss, M.C., Underwood, L.A., Enright, M., Hill, S., Marshall, R., Tipton, P., et al. (2013). Treatment impact of an integrated sex offender program as measured by J-SOAP-II.Journal of Correctional Health Care, 19(2), 113-123
- Reynolds, C. (1987). Reynolds Adolescent Depression Scale (RADS): Professional manual. Odessa, FL: Psychological Assessment Resources
- Reynolds, C., &Kamphaus, R. (1998). The behavioral assessment scales for children, second edition: professional manual. Odessa, FL: Psychological Assessment Resources
- Reynolds, C.R., & Richmond, B.O. (1978). What I Think and Feel: A revised measure of children's manifest anxiety. Journal of Abnormal Child Psychology, 6, 271-280
- Reynolds, C.R., & Richmond, B.O. (1985). Revised Children's Manifest Anxiety Scale (RCMAS). Los Angeles: Western Psychological Services
- Seto, M.C., and Lalumiere, M.L. (2010). What is so special about male adolescent sexual offending? A review and test of explanations through meta-analyis.Psychological Bulletin, 136, 526-575
- Schelle, S. (2010).Juvenile recidivism. Indianapolis: Indiana Department of Correction
- Underwood, L.A., & Washington, A. (2016).Mental illness and juvenile offenders.International Journal of Environmental Research and Public Health, 13, 228 – 241
- Van Wijk, A., Vermeiren, R., Loeber, R., Hart-Kerkhoffs, L., Doreleijers, T. &Bullens, R. (2006). Juvenile sex offenders compared to non-sex offenders: A review of the literature 1995-2005. Trauma, Violence, & Abuse, 7: 227-243.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 6338
- [From(publication date):
June-2017 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 5475
- PDF downloads : 863