The Impact of Obstructive Sleep Apnea and Daytime Sleepiness on Work Performance: An Observational Cross-Sectional Study in a North African Population
Received: 15-Jan-2018 / Accepted Date: 22-Jan-2018 / Published Date: 05-Feb-2018 DOI: 10.4172/2329-6879.1000270
Abstract
Background: Obstructive sleep apnea hypopnea syndrome (OSAHS) has been shown to be associated with many serious health conditions. The impact on occupational health is still unclear as it was scarcely studied.
Purpose: The aim of this study was to assess the association of work performance with OSAHS and daytime sleepiness.
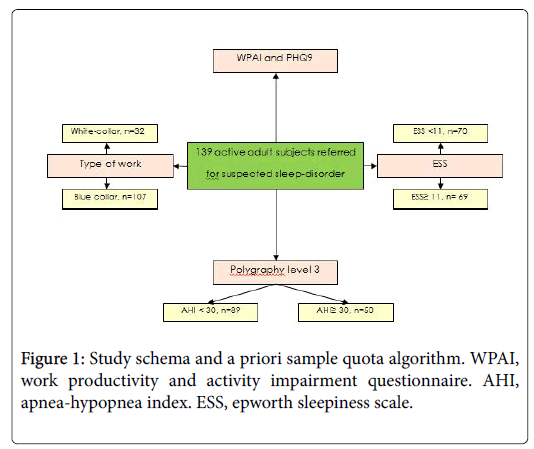
Methods: A cross-transversal study was conducted including Tunisian active adult subjects referred for suspected sleep disordered breathing. All subjects completed the Epworth Sleepiness Scale (ESS), the Work Productivity and Activity Impairment Questionnaire (WPAI), and the Patient Health Questionnaire 9 (PHQ9). They all underwent polygraph testing level 3.
Result: One hundred thirty-nine subjects completed the survey, including 107 (77%) blue-collar workers, and 32 (23%) white-collar workers. Participants were classified as following: 50 patients with apnea hypopnea index (AHI) ≥ 30 and 89 with AHI <30. Among the four outcomes of the WPAI scale, only presenteeism was associated with AHI (p=0.012). A significant association has been found between daytime sleepiness and three outcomes of WPAI. Sleepy patients with ESS ≥ 11 had lower work performance in terms of presenteeism (42.46 ± 28.40 vs. 24.71 ± 24.77 p=0.0001), absenteeism (12.26 ± 25.51 vs. 6.05 ± 18.32, p=0.101), overall work productivity loss (47.43 ± 31.65 vs. 26.58 ± 28.47, p= 0.0001), and decline in activity (46.67 ± 30.75 vs. 32.14 ± 27.02, p=0.004) in comparison with non-sleepy participants. A strong correlation of presenteeism and overall work productivity loss scores with ESS was demonstrated among white-collar workers (r=0.624, p=0.0001; r=0.602, p=0.0001 respectively). PHQ9 score was significantly higher in sleepy subjects (p=0.0001). Near miss accidents in the workplace and work related accidents were significantly more frequent in those with ESS ≥ 11 (p=0.012, p=0.026; respectively).
Conclusion: The most relevant finding of this study was the involvement of daytime sleepiness in performance impairment, while the impact of AHI was less clear.
Keywords: Sleep apnea syndromes; Work performance; Depression
Introduction
Obstructive sleep apnea hyponea syndrome (OSAHS) is a common disease with reported rates of 3-7% in middle age population [1]. It’s characterized by repetitive partial or complete collapse of the airway during sleep, resulting in apnea or hypopnea. These episodes cause intermittent hypoxia, repetitive arousal from sleep, which leads to increased sympathetic activity, increased respiratory effort, and sleep fragmentation. Untreated OSAHS is incriminated in increased risk of several co-morbidities including cardiovascular diseases, and metabolic syndrome. Disrupted sleep can also result in tiredness, lack of energy, and a feeling of weakness during the day. Severe forms of the disease are often associated with excessive daytime sleepiness and micro-sleep episodes. Furthermore, persons with OSAHS may experience decreased quality of life, significant cognitive limitations and mood disorders such as anxiety, irritability, and depression.
Because of these adverse mood changes and neurocogintive dysfunction, it has been suggested that OSAHS may be detrimental to work performance, and associated with greater risk of workplace accidents. However, this hypothesis has been little explored, and even less so among North African population and no solid conclusion could be drawn due to disputed results.
Considering the above findings and rationale, we designed an observational cross-sectional study in order to gain a greater understanding in how OSAHS and daytime sleepiness affect work productivity and workplace accidents in a sample of subjects referred for suspected sleep-disorders.
Material And Methods
Participants
The study was performed during the period of July 2015 to April 2017 on a subset of participants referred to the department of respiratory and sleeps medicine of Hedi Chaker University Hospital in Sfax, Tunisia for suspected sleep-disorders. Only subjects between the age of 18 and 60 years, and actively employed for at least 6 months were included in the study. The exclusion criteria were: another sleep disorder, previous treatment for sleep apnea, medications that could affect sleep and/or vigilance, serious medical conditions, overt psychiatric disorders including alcohol or other drug addiction, and pregnancy. The study was approved by the institutional Human research ethics committee, and consent was obtained from all participants.
Instruments
Self-administrated questionnaires: Consenting participants were given extensive questionnaire regarding their socio-demographics, habits, medical history, and working conditions such as work schedule, shift work, number of worked hours and the kind of work they had over the last 24 months. The following groupings were classified as white-collar workers: clerks, technicians and associate professionals, highly skilled professionals, directors and managers. Otherwise, unskilled workers, production-line/machine workers and drivers, skilled manual workers, farm/horticulture workers, service workers and retailers were classified as blue-collar workers [2]. The survey also included questions aimed at evaluating the number of work-related accidents, the number of sick leave more than 30 days over the last year, as well as somatic symptoms of stress such as epigastralgia, chest tightness, dyspnea and muscle tension.
Elsewhere, participants completed the Work Productivity and Activity Impairment (WPAI) questionnaire, in order measure impairments in work and activities. Daytime sleepiness was assessed by Epworth Sleepiness Scale (ESS), while Patient Health Questionnaire (PHQ9) was used to screen for the presence and severity of depression according to DSM-IV criteria.
Work productivity and activity impairment (WPAI) questionnaire: The WPAI [3] is a validated instrument that consists of six questions: Q1=currently employed; Q2=hours missed due to health problems; Q3=hours missed due to other reasons; Q4=hours actually worked; Q5=degree health affected productivity while working; and Q6=degree health affected regular activities. According to the questionnaire responses, scores are generated for four main outcomes including absenteeism (work time missed), presenteeism (impaired productivity at work), and overall work productivity loss (absenteeism +presenteeism) in the past 7 days. Impairment in performing daily (non-work) activities, such as work around the house, shopping, child care, exercising, etc. is also assessed.
The different outcomes are expressed as percentage score, with higher scores indicating greater impairment. They are generated as the following:
1. Absenteeism = Q2/(Q2+Q4) for those who were currently employed;
2. Presenteeism = Q5/10;
3. Percent overall work loss due to health= Q2/(Q2+Q4)+[(1-Q2/ (Q2+Q4)) × Q5/10] for those who were currently employed;
4. Percent activity impairment due to health= Q6/10 for all respondents. For those who missed work and did not actually work in the past seven days, the percent overall work impairment due to health is equal to the percent work time missed due to health.
Patient health questionnaire (PHQ9): The PHQ-9 is a validated selfadministered tool used in primary care to screen patients for depression and to estimate symptoms severity. By assessing patient’s mood over the last 2 weeks, the questionnaire allows scoring each of the 9 DSM-IV criteria for Major Depressive Disorder as ‘0’ (not at all) to ‘3’ (nearly every day). As a severity measure, the PHQ-9 score can range from 0 to 27. PHQ-9 scores of 5, 10, 15, and 20 represented mild, moderate, moderately severe, and severe depression, respectively [4].
Epworth sleepiness scale (ESS): Daytime sleepiness was estimated using the Arabic version of the ESS (AESS) [5]. It’s an eight selfcompleted questionnaire assessing the probability of falling asleep in various daytime situations, for a total score ranging from 0 to 24. Depending on their ESS score (ESS<11, ESS ≥ 11), subjects were divided into two groups of subjective sleepiness severity. Those with an ESS score ≥ 11 were considered to have significant daytime sleepiness.
The AESS was created according to the recommendations of the ISPOR Task Force for Translation and Cultural Adaptation with bilingual individuals (Table 1). It had shown a high internal consistency (Cronbach’s alpha 0.76, intra-class correlation coefficient of 0.85 (IC95%: 0.76–0.92), thus it’s considered valid instrument for the evaluation of daytime sleepiness in Arabic speaking populations [5].
| Groups | |||||||
|---|---|---|---|---|---|---|---|
| Type of work | AHI | ESS | Total | ||||
| Blue collar | White collar | <30 | ≥ 30 | <11 | ≥ 11 | n=139 | |
| (n=107) | (n=32) | (n=89) | (n=50) | (n=70) | (n=69) | ||
| Age, years | 48.4 ± 10.2 | 45.19 ± 10,7 | 47.43 ± 11.003 | 48.1 ± 9.2 | 47.8 ± 10.6 | 47.5 ± 10.2 | 47.6± 10.4 |
| Sex-ratio | 2.57* | 0.88* | 1.28** | 5.25** | 2.33 | 1.65 | 1.96 |
| BMI (Kg/m2) | 33 ± 5.83 | 35.23 ± 6.97 | 32.41 ± 6.44** | 35.46 ± 5.1** | 32.05±4.99** | 34.99 ± 6.87** | 33.51 ± 6.16 |
| Education, n (%) | |||||||
| No studies | 7(6.5) | 0(0) | 6(6.7) | 1(2) | 4(5.4) | 3(4.3) | 7(5) |
| Primary | 48(44.9)*** | 1(3.1)*** | 34(38.2) | 24(34.3) | 24(34.3) | 25(36.2) | 49(35.3) |
| Secondary | 39(36.4) | 10(31.3) | 29(32.6) | 20(40) | 23(32.9) | 26(37.7) | 49(35.3) |
| Technical training | 0(0)*** | 16 (50)*** | 9(10.1) | 7(14) | 13(18.6) | 3(4.3) | 16(11.5) |
| University studies | 13(12.1) | 5(15.6) | 11(12.4) | 7(14) | 6(8.6) | 12(17.4) | 18(12.9) |
| Working schedule, n (%) | |||||||
| Full time | 79(73.8) | 29(90.6) | 72(80.9) | 36(72) | 56(80) | 52(75.4) | 108(77.7) |
| Nocturnal work | 7(6.5) | 1(3.1) | 4(4.5) | 4(8) | 3(4.3) | 5(7.2) | 8(5.8) |
| Shift work | 21(19.6) | 2(6.3) | 13(14.6) | 10(20) | 11(15.7) | 12(17.4) | 23(16.5) |
| Habits, n (%) | |||||||
| Smoking | 36(81.8) | 8(18.2) | 26(59.1) | 18(40.9) | 25(56.8) | 19(43.2) | 44(31.7) |
| Alcoholism | 36(91.3) | 1(7.7) | 5(38.5) | 8(61.5) | 7(53.8) | 6(46.2) | 13(9.4) |
| Comobidities | |||||||
| Hypertension | 37(72.5) | 14(27.5) | 29(56.9) | 22(43.1) | 25(49) | 26(51) | 51(36.7) |
| Diabeties | 23(85.2) | 4(14.8) | 19(70.4) | 8(29.6) | 13(48.1) | 14(51.9) | 27(19.4) |
| Dyslipidemia | 26(70.3) | 11(29.7) | 23(62.2) | 14(37.8) | 21(56.8) | 16(43.2) | 37(26.6) |
| Cardiovascular disease | 25(86.2) | 4(13.8) | 20(69) | 20(31) | 16(55.2) | 13(44.8) | 29(20.9) |
| Lung disease | 33(84.6) | 6(15.4) | 27(69.2) | 12(30.8) | 15(38.5) | 24(61.5) | 39(28.1) |
| Endocrine disease | 6(46.2)* | 7(53.8)* | 9(69.2) | 4(30.8) | 5(38.5) | 8(61.5) | 13(9.4) |
| Neurological disease | 5 (71.4) | 2 (28.6) | 6 (85.7) | 1 (14.3) | 4 (57.1) | 3 (42.9) | 7 (5) |
| ESS | 11.34 ± 6.25 | 9.59 ± 5.76 | 10.57 ± 5.90 | 11.58 ± 6.61 | <11 | ≥ 11 | 10.94 ± 6.16 |
| Polygraphy | |||||||
| AHI (events/hour) | 24.86 ± 24.98 | 26.16 ± 25.46 | <30 | ≥ 30 | 21.68 ± 18.53 | 28.67 ± 29.93 | 25.15 ± 25.01 |
| ODI (events/hour) | 23.29 ± 24.68 | 21.68 ± 24.71 | 9.17 ± 8.51*** | 47.38 ± 24.93*** | 18.24 ± 15.73* | 27.66 ± 30.53* | 22.92 ± 24.61 |
| Mean SpO2 (%) | 93.08 ± 2.96 | 92.98 ± 5.67 | 94.02 ± 2.19*** | 91.33 ± 5.10*** | 93.82 ± 2.23* | 92.28 ± 4.70* | 93.05 ± 3.74 |
| T90% (%) | 11.26 ± 19.74 | 10.29 ± 23.62 | 5.51 ± 14.18*** | 20.88 ± 26.1*** | 8.59 ± 17.34 | 13.51 ± 23.34 | 11.03 ± 20.61 |
| AHI: Apnea-hypopnea index. ESS: Epworth sleepiness scale. BMI: Body mass index. ODI: Oxygen desaturation index. SpO2: Arterial oxygen saturation. T90%: Total sleep time with arterial oxygen saturation lower than 90%. * 0.01 ≤ p | |||||||
Table 1: Socio-demographic and clinical characteristics of study participants.
Nocturnal polygraph recording: Nocturnal polygraph recording was performed for all patients using type III polysomnography (PSG) (EmblaTM N7000, ResMed Corp., San Diego, CA, United States) according to standard techniques. Airflow was monitored by an oronasal air pressure transducer (EmblaTM N7000, ResMed Corp., San Diego, CA, United States), thoracic and abdominal respiratory effort and body position by uncalibrated impedance plethysmography belts (EmblaTM N7000, ResMed Corp., San Diego, CA, United States), and arterial oxygen saturation (SpO2) by digital pulse oximetry. Snoring was recorded by a microphone (EmblaTM N7000, ResMed Corp., San Diego, CA, United States) placed on the anterior neck. Prior to sleep study, patients were recommended to ovoid caffeinated drinks and foods, alcohol, and drugs that could interfere with sleep architecture.
Scoring respiratory events was performed manually by one doctor according to the standard criteria of the American Academy of Sleep Medicine (AASM) published in 2012 [6]. Obstructive apnea was defined as a 90% decrease in airflow relative to the basal amplitude persisting for at least 10 seconds in the presence of thoracic and abdominal movements. Hypopnea was defined as a 30% decrease in the airflow amplitude relative to the baseline persisting for at least 10 seconds, with an associated 3% oxygen desaturation. Patients having an apnea hypopnea index (AHI) <5/hour without any evocative symptoms apart from snoring were classified as controls, while patients with an AHI of 5 or greater and clinical symptoms were considered positive for OSAHS [7].
According to the AHI, subjects were classified into groups. One group included subjects with severe OAHS (AHI ≥ 30), while a second included subjects without OAHS (
Depression rates: Considering the total sample, PHQ9 score was significantly higher in subjects with daytime sleepiness compared with those with normal ESS (p=0.0001). The observed difference between the two groups was significant whatever the AHI was Table 2). In contrast, no significant difference was found in PHQ9 score according to AHI, T90%, and IDO.
| Variables | Groups | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| IAH | ≥ 30(n=50)Total (n=139) | ||||||||
| ESS | <11 | ≥ 11 | p | <11 | ≥ 11 | p | <11 | ≥ 11 | p |
| PHQ9 | 6.56 ± 5.85 | 11.72 ± 4.69 | 3-Oct | 6.46 ± 4.04 | 12.38 ± 5.52 | 3-Oct | 6.46 ± 4.4 | 12.38 ± 5.52 | 3-Oct |
| PHQ9: Patient health questionnaire. ESS: Epworth sleepiness scale AHI: Apnea-hypopnea index. | |||||||||
Table 2: Assessment of depression severity with patient health questionnaire according to Epworth sleepiness scale.
Somatic symptom of stress, and work related accidents: Somatic symptom of stress, near miss accidents in the workplace, and work related accidents were not associated with any sleep polygraphic parameters including AHI, ODI, and T90% (Figure 1). However, near miss accidents in the workplace and work related accidents were significantly more frequent in sleepy subjects (ESS ≥ 11), as compared with ESS
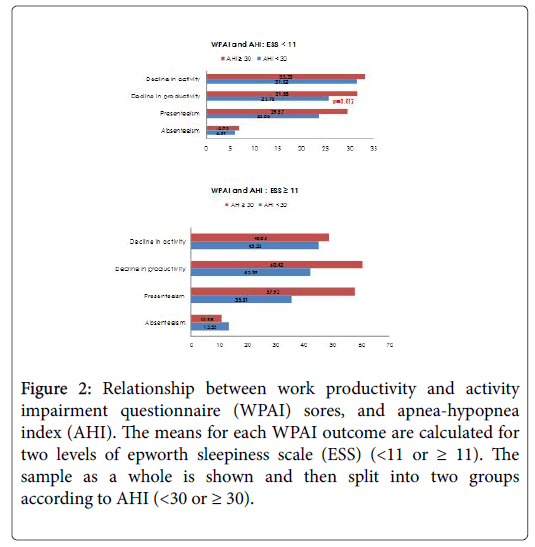
Work productivity: Among the four outcomes of the WPAI scale, only presenteeism was associated with AHI. Actually, patients with AHI ≥ 30 had a significantly higher score of presenteeism in comparison with those with AHI Figure 2).
Elsewhere, when most hypoxemic subjects (T90% ≥ 30%) were compared with the least hypoxemic subjects (T90% <30%), significant higher presenteeism was observed (46.67 ± 28.08 vs. 31.57 ± 27.57; p=0.032).
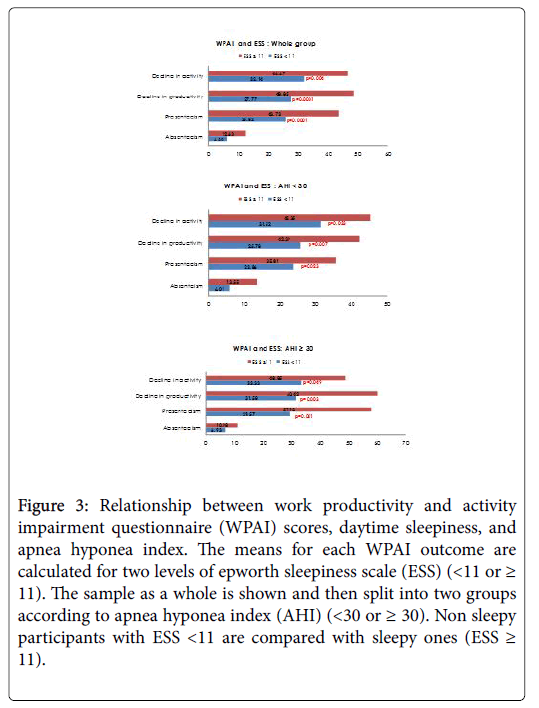
Considering subjective sleepiness, presenteeism, impairment in performing daily activities and overall work productivity loss scores were significantly higher in sleepy subjects when compared with nonsleepy ones. Absenteeism was similar in both groups. These results were observed in the sample as a whole as well as among the two AHI groups (Figure 3).
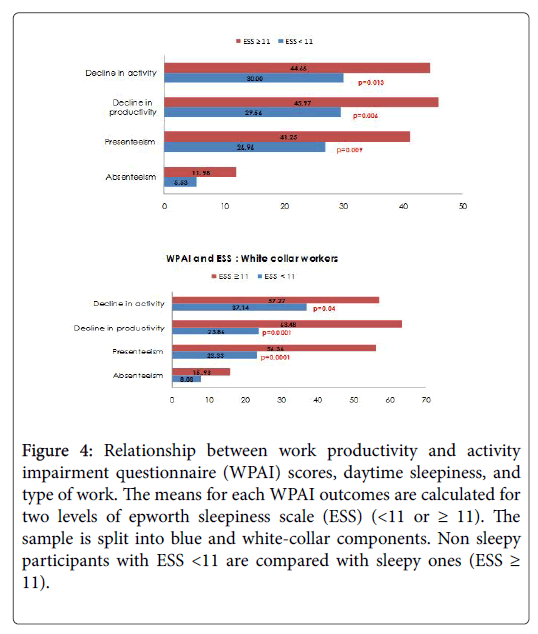
A similar pattern was observed when subjects were divided into blue and white-collar workers with significant higher scores in sleepy subjects for presenteeism, impairment in performing daily activities and overall work productivity loss, but not for absenteeism. It is interesting to observe, however, that the impact of daytime sleepiness was more marked among white-collar workers (Figure 4).
In the total sample, a weak correlation was found between presenteeism and both AHI (r=0.212, p=0.012) and T90% (r=0.222, p=0.009) (Table 3). In addition, the four outcomes of the WPAI scale were weakly correlated with PHQ9 score. Weak correlations were also detected between both presenteeism and overall work productivity loss scores and ESS. This correlation was stronger among white-collar workers (r=0.624, p=0.0001; r=0.602, p=0.0001 respectively). In the same group, presenteeism and overall work productivity loss scores were moderately correlated with AHI (r=0.395, p=0.025; r=0,382, p=0.031 respectively).
| Variables | Groups | |||||
| Whole sample (n=139) | Blue collar (n=107) | White collar (n=32) | ||||
| r | p | r | p | r | p | |
| With AHI | ||||||
| Presenteeism | 0.212 | 0.012 | 0.165 | 0.09 | 0.395 | 0.025 |
| Absenteeism | -0.027 | 0.754 | -0.047 | 0.627 | 0.031 | 0.866 |
| Decline in productivity | 0.153 | 0.071 | 0.085 | 0.383 | 0.382 | 0.031 |
| Decline in activity | -0.015 | 0.862 | -0.025 | 0.795 | 0.016 | 0.93 |
| With T90% | ||||||
| Presenteeism | 0.222 | 0.009 | 0.186 | 0.055 | 0.352 | 0.048 |
| Absenteeism | 0.043 | 0.613 | 0.111 | 0.254 | -0.127 | 0.489 |
| Decline in productivity | 0.161 | 0.058 | 0.131 | 0.178 | 0.251 | 0.165 |
| Decline in activity | -0.007 | 0.935 | -0.036 | 0.711 | 0.096 | 0.601 |
| With PHQ9 | ||||||
| Presenteeism | 0.447 | 0.0001 | 0.404 | 0.0001 | 0.61 | 0.0001 |
| Absenteeism | 0.233 | 0.006 | 0.287 | 0.003 | 0.089 | 0.628 |
| Decline in productivity | 0.432 | 0.0001 | 0.436 | 0.0001 | 0.423 | 0.016 |
| Decline in activity | 0.347 | 0.0001 | 0.284 | 0.003 | 0.574 | 0.001 |
| With ESS | ||||||
| Presenteeism | 0.296 | 0.0001 | 0.226 | 0.019 | 0.624 | 0.0001 |
| Absenteeism | 0.096 | 0.263 | 0.083 | 0.395 | 0.163 | 0.373 |
| Decline in productivity | 0.299 | 0.0001 | 0.222 | 0.022 | 0.602 | 0.0001 |
| Decline in activity | 0.189 | 0.026 | 0.15 | 0.124 | 0.421 | 0.016 |
| AHI: Apnea-hypopnea index. T90%: Total sleep time with arterial oxygen saturation lower than 90%. PHQ9: Patient health questionnaire. ESS: Epworth sleepiness scale | ||||||
Table 3: Correlations of work productivity and activity impairment scores with apnea hypopnea index, patient health questionnaire and epworth sleepiness scale.
Discussion
In this study, a decreased work performance (as assessed by a validated scale) was observed in patients with severe OSAHS, but also and most importantly in those with daytime sleepiness. This impact has been found to be more marked in white-color workers as compared with blue-color workers.
Despite the impact of OSAHS on occupational health has been suspected since a long time, only few studies have been performed to evaluate this relationship, showing divergent results. Jurado-Gimez B et al. [8] studied a sample of 259 Spanish individuals referred to the sleep disorders clinic for suspected OAHS. Participants were classified to OAHS group or a non-OAHS according to polysomnography results. Both groups had similar rates of work-related accidents. However, OAHS was significantly associated with higher rate of absenteeism. Psychological distress and OAHS were associated with significantly poorer work productivity as assessed on the Spanish IMPALA (impact of disease on work productivity) index. A diagnostic of OAHS was the variable with the most importance impact on the working lives of patients, while excessive daytime sleepiness and subjective quality of sleep (as assessed using Pittsburg Sleep Quality index) was not associated with any influence.
For his part, Muglgrew et al. [9] studied a sample of 428 Canadian adults that had undergone overnight polysomnography for sleepdisordered breathing. OAHS severity defined by AHI was not associated with any dimension of work limitation questionnaire (WLQ). In contrast, subjective sleepiness as assessed by ESS was strongly associated with three of the four scales of WLQ.
Similarly in our study, work performance as assessed by WPAI was significantly affected in sleepy patients with ESS ≥ 11, when compared with non-sleepy patients, while the impact of OAHS severity defined by AHI was less clear. The same conclusion was reached by Bean [10] when comparing a group including 1759 subjects with OAHS, depression, narcolepsy, multiple sclerosis, with 1977 subjects without these conditions. In both, group, excessive sleepiness was associated with highly significant impairment in work productivity for all measures, except for absenteeism.
Many other studies had also reached the same conclusion about the negative impact of daytime sleepiness on work performance [11-13] however some of these have limitations. Actually, surveys were almost always focused on subjects referred for suspected-disordered breathing rather a community-based sample as was the case for Muglgrew et al. [9]. No objective evaluation was performed to better assess the impact of daytime sleepiness on work performance. Some authors did not perform an objective sleep study [11,13] while others used only polygraph as their sleep study [14].
Yet, despite the above limitations, we could still deduce that daytime sleepiness as a common feature of OAHS could cause greater impairment than AHI on work performance. These findings would support the current controversy about the value of AHI as an indicator of OAHS severity. Actually, several recent studies have suggested that AHI would not be enough to predict adverse safety and health consequences of OAHS, particularly daytime fatigue and sleepiness [15]. This is consists with the results of our study that showed no association between ESS and AHI. Therefore, patients with mild to moderate disease (5 ≤ AHI <30) may be more tired and sleepy, and consequently have lower work performance than patients with severe disease (AHI ≥ 30). This means that AHI would not be appropriate to objectively assess the impact of OAHS on work performance. Thus, a novel parameter such as the recently suggested AHI adjusted should be used to improve the recognition of OAHS patients, as well as accuracy and reliability of disease severity estimates [16].
In our study, depression score was not associated with any polygraphic parameter, but was significantly higher in patients with ESS ≥ 11. This fact may contribute to impair work performance in sleepy patients. Elsewhere, Mulgrew et al. found that the impact of subjective daytime sleepiness as assessed by ESS on work performance was equal between white-color and blue-color workers [17]. As opposed to these findings, white-color workers appeared to be more marked affected in our study. This difference may be explained by the sedentarily nature of white-color work that makes sleepiness harder to fight off.
Some studies have suggested an increased risk of work-related accidents due to OAHS symptoms. However, only very few studies have assessed this relationship in patients with definitive diagnosis of OAHS. Besides, studies did not consistently find that daytime sleepiness and the severity of OAHS were correlated with crash risk [8,17]. Our results showed that Work-related accidents were associated with ESS, but not with AHI. In line with this study, Lindberg et al. [18] showed a 2-fold increase in the risk of work-related accidents in snorer and sleepy subjects when compared with subjects without those symptoms. Jurado-Gimez B et al. [8] reported that the OAHS group and the control group had similar rates of workplace accidents.
Our study has limitations. First, the sample would not be representative of our target population as it was small in size, and was selected among subjects referred for suspected sleep disordered breathing. This may have introduced a selection bias making our results not representative enough to be extrapolated beyond our referral group. A second limitation may be related to using polygraphy, and not polysomnography, for diagnosing OAHS which may lead to an underestimation of the prevalence and the severity of the disease. Third, work performance was assessed by WPAI scale which has been validated into many languages, but neither in Arabic nor in Tunisian dialect. In addition, despite many confounders were considered when including subjects, it remains still difficult to conclude about the association of work performance with OAHS and daytime sleepiness. The contribution of other unrecognized confounders in this association could not be excluded given the cross-sectional nature of our study. Finally, there was no follow up-analysis of patients posttreatment which would be helpful to have more information about the association in question.
Conclusion
To our knowledge, this is the first comprehensive study of the burden of OSAHS and daytime sleepiness on occupational health in a Nord African population. Our study demonstrated that daytime sleepiness may lead to low work performance in a population referred for suspected sleep-disordered breathing. This impact was more marked in white-color workers as compared with blue-color workers. In contrast, the relationship between OAHS (as defined by AHI) and work performance was less clear. These results suggest that screening for excessive daytime sleepiness should be considered as a part of occupational health assessment. It would be also interesting to define new instruments other than conventional AHI to more accurately evaluate the impact on the working lives.
References
- Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5: 136-143.
- Reilly MC, Zbrozek AS, Dukes EM (1993) The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics 4: 353–365.
- Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 16: 606–613.
- Riachy M, Juvelikian G, Sleilaty G, Bazarbachi T, Khayat G, et al. (2012) Validation of the Arabic version of the epworth sleepiness scale: Multicentre study. Rev Mal Respir 29: 697–704.
- Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, et al. (2012) Rules for scoring respiratory events in sleep: Update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American academy of sleep medicine. J Clin Sleep Med 15: 597-619.
- Ito E, Inoue Y (2015 ) The international classification of sleep disorders, American academy of sleep medicine. Includes bibliographies and index. Nihon rinsho 73: 916-923.
- Jurado-Gámez B, Guglielmi O, Gude F, Buela-Casal G (2015) Workplace accidents, absenteeism and productivity in patients with sleep apnea. Arch Bronconeumol 51: 213-218.
- Mulgrew AT, Ryan CF, Fleetham JA, Cheema R, Fox N, et al. (2007) The impact of obstructive sleep apnea and daytime sleepiness on work limitation. Sleep Med 9: 42-53.
- Dean B, Aguilar D, Shapiro C, Orr WC, Isserman JA, et al. (2010) Impaired health status, daily functioning, and work productivity in adults with excessive sleepiness. J Occup Environ Med 52: 144-149.
- Sivertsen B, Overland S, Glozier N, Bjorvatn B, Maeland JG, et al. (2008) The effect of OSAS on sick leave and work disability. Eur Respir J 32: 1497–1503.
- Swanson LM, Arnedt JT, Rosekind MR, Bolenky G, Balkin TJ, et al. (2011) Sleep disorders and work performance: Findings from the 2008 National Sleep Foundation Sleep in America poll. J Sleep Res 20: 487–494.
- Sivertsen B, Björnsdottir E, Overland S, Bjorvatn B, Salo P (2013) The joint contribution of insomnia and obstructive sleep apnoea on sickness absence. J Sleep Res 22: 223–230.
- Accattoli MP, Muzi G, dell’Omo M, Mazzoli M, Genovese V, et al. (2008) Occupational accidents, work performance and obstructive sleep apnea syndrome (OSAS). G Ital Med Lav Ergon 30: 297–303.
- David WH (2016 ) Sleep apnea severity classification—revisited. Sleep 39: 1165-1166.
- Muraja-Murro A, Kulkas A, Hiltunen M, Kupari S, Hukkanen T, et al. (2014) Adjustment of apnea-hypopnea index with severity of obstruction events enhances detection of sleep apnea patients with the highest risk of severe health consequences. Sleep Breath 18: 641-647.
- Ellen RL, Marshall SC, Palayew M, Molnar FJ, Wilson KG, et al. (2006) Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med 2: 193-200.
- Lindberg EV, Carter NE, Gislason T, Janson C (2001) Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med 164: 2031-2035.
Citation: Msaad S, Kammoun N, Hajjaji M, Kalle N, Bahloul N, et al. (2018) The Impact of Obstructive Sleep Apnea and Daytime Sleepiness on Work Performance: An Observational Cross-Sectional Study in a North African Population. Occup Med Health Aff 6: 270. DOI: 10.4172/2329-6879.1000270
Copyright: © 2018 Msaad S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6464
- [From(publication date): 0-2018 - Nov 13, 2025]
- Breakdown by view type
- HTML page views: 5414
- PDF downloads: 1050