The Impact of Digital Education Material in Improving Clinical and Behavioural Outcomes in Home-Based Cardiac Rehabilitation Participants: A Pilot Study
Received: 14-Jan-2022 / Manuscript No. jcpr-22-51674 / Editor assigned: 16-Jan-2022 / PreQC No. jcpr-22-51674 (PQ) / Reviewed: 30-Jan-2022 / QC No. jcpr-22- 51674 / Revised: 04-Feb-2022 / Manuscript No. jcpr-22-51674 (R) / Published Date: 11-Feb-2022 DOI: 10.4172/jcpr.1000153
Abstract
Background: Home-based cardiac rehab (HBCR) program is a potential solution to overcome CR barriers, however its setting in Malaysia is still in its infancy. Reduced physical interaction with CR providers among HBCR participants may also mean reduced cardiovascular knowledge-sharing opportunities. We hypothesized by delivering an education material using a commonly used internet-based instant messaging app to HBCR participants may compensate for this limitation and improve outcome and subsequently improve HBCR delivery.
Aims: To assess the feasibility and impact of a digital education material in improving clinical and behavioural outcomes in home-based CR phase 2 (CRP2) participants.
Methods and Results: A prospective, multiple assessment study was conducted involving home-based CR patients in a single center. Research participants were given digital educational material via an internet-based instant messaging app at the beginning of CRP2 and followed up for 12 weeks. The frequency of monthly faceto- face follow-up with CR providers remained unchanged. The uptake rate was 91.3%, with an 80% adherence rate. 92.9% who completed the intervention complied with the CRP2 program. The majority of participants reported positive feedback and high acceptability for this intervention. In a pre/post comparison to intervention completers, improvement was noted in the ABCD-risk score, smoking cessation, medication adherence, compliance to weekly exercise, and treadmill exercise stress test endurance parameters.
Conclusion: A digital education material shared via an internet-based instant messaging app is a feasible intervention to HBCR participants and has a positive impact on behavioural and clinical outcomes.
Keywords
Cardiac rehabilitation; Secondary prevention; Patient education handout; Patient compliance
Introduction
Background
Ischaemic heart disease is a global disease burden and remains as the highest cause of death and disability among developing countries such as Malaysia for the past decade [1-3]. National statistics estimated among adult Malaysians, 17.5% are living with diabetes, 30.3% with hypertension, 47.7% with hypercholesterolemia and 17.7% with obesity, and these non-communicable diseases (NCDs) contributed to an estimated USD 3.09 billion of economic loss due to reduced labour productivity and burden of disease cost [4]. With the recent COVID-19 pandemic, the need for public health measures intended to curb its spread may promote a sedentary lifestyle [5, 6], posing a threat to further increasing the incidence and prevalence of cardiovascular disease in the nation.
Cardiac rehabilitation (CR) is a cost-effective, Class IA recommendation for cardiovascular (CV) secondary prevention [7-10] and has shown to improve control of cardiovascular risk factors, exercise capacity, quality of life, hospital readmission rates and mortality rates [11, 12]. However, despite its proven benefits, enrolment and adherence to CR is still low, with an overall uptake rate ranging between 30-50% [13-15], due to various patient or service-related barriers. One strategy to overcome these barriers and improve CR uptake is a home-based CR program. Home-based CR (HBCR) program is proven to have similar outcomes compared to centre-based program (CBCR) in improving cardiovascular risk factors, psychological status, and exercise capacity [16], better adherence to CR [17], and a better-improved quality of life [18].
However, the setting of HBCR in the Western countries where promising outcomes were seen including frequent nurse-led phone call follow-ups, scheduled home visits by trained allied health staff, and having equipped exercise facilities in the community, has yet to be made available in a middle-income country like Malaysia. Like many developing countries, CR spots per IHD patient is relatively low [19], and the service is only available at tertiary hospitals with in-house rehabilitation medicine services, mostly in capital cities. A single-centre observational study highlighted logistical barriers, work/time conflicts, and healthcare barriers as the main CR barriers perceived by Malaysians [20]. In addition to the low CR density, Malaysians in suburban and rural areas face multiple geographical and socioeconomic barriers, adding to the low CR uptake; hence any work to improve HBCR delivery should be made a priority. With the recent experience of the COVID-19 pandemic where non-emergency hospital visitations were discouraged and non-essential medical services including CR needed to be reduced, HBCR became the sole option for CR survivors.
Educational interventions tailored to patients with coronary artery disease (CAD) are proven to improve disease-related knowledge, self-management behaviours [21], and health-related quality of life [22], and event recurrences. Unfortunately, although patient education is considered a core component of CR, no educational program has been standardized globally and locally. In addition, most available patient education materials are developed in Western countries which some recommendations such as dietary advice and practical lifestyle modification tips may not be culturally adaptable. As opposed to CBCR, HBCR participants have lesser face-to-face interaction with CR providers, which may lead to lesser opportunities for this heart-healthy education to be delivered efficiently thus, jeopardizing the effort to promote secondary prevention in CR.
We aim to improve the delivery of HBCR in Malaysia by formulating culturally adapted comprehensive education material to HBCR patients that is shared using a commonly used internet-based instant messaging mobile app (IBIMMA) to compensate for the reduced physical interaction with CR providers. Before proceeding to a larger scale, controlled study to define its effectiveness in improving behavioural and clinical outcomes in HBCR participants, a pilot study to assess its feasibility and apparent impact is deemed necessary. The objectives of this study are to determine the feasibility of providing a structured patient education material (SPEM) to HBCR participants, and to assess the impact of SPEM on their behavioural and clinical outcomes, cardiovascular (CV) risk knowledge, perceived CV risks, and perceived benefits and intention to a heart-healthy lifestyle.
Method
Study design
This study employs a prospective multiple assessment baseline design to assess the impact of SPEM by comparing multiple outcome measurements obtained in different phases, throughout the second phase of CR (CRP2), which is the intensive phase of outpatient CR.
Study Setting and Participants
This study took place at an outpatient cardiac rehabilitation clinic in a tertiary university hospital in Kuala Lumpur. The standard practice in this centre for HBCR participants is a 4-weekly appointment with CR physiotherapists and occupational therapists, while their CBCR counterparts are seen once weekly for 12 weeks. At the end of the 12 week program, home-based participants will only have 3 face-to-face sessions with CR providers, as opposed to 12 sessions for centre-based participants.
All eligible CRP2 participants who opted or were assigned to a home-based CRP2 were offered to join this study. Verbal and written consent was obtained from each participant. The inclusion criteria were as follows: adults aged 20-70 years, stratified as low to moderate risk for CR program as per the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) Standards, able to participate in a treadmill exercise stress test, and cognitively able to give consent and use a smartphone. Participants who are risk-stratified as high risk as per the AACVPR standards are excluded from the study.
Ethical Approval
This study complies with the Declaration of Helsinki ethical standards and is approved by UMMC Medical Ethics (MREC ID: 20201010-9146). It is registered at the ClinicalTrials.gov web-based registry (ID: NCT05045118).
Procedure
Standard care involves individualized consultation and rehabilitation prescription to CR participants including supervised exercise prescription, activities of daily living assessment and retraining, activity modification with energy conservation, and stress management, without a standardized educational material. SPEM provides a general, structured written education material that is shared digitally via IBIMMA as a supplement to standard care to all study participants.
Development and content of SPEM
SPEM is a locally produced, comprehensive education material that adapts the principles of cardiac rehabilitation endorsed by the American Heart Association (AHA) and the American Association of Cardiovascular Heart and Pulmonary Rehabilitation (2013) Including (1) understanding and managing the disease process; (2) beginning an exercise program; (3) helping the patient modify risk factors; (4) providing vocational guidance to help the patient to return to work; (5) supplying information on physical limitations; and (6) providing emotional support [23]. The main themes of SPEM focus on addressing the 5 main target health behaviours in CR which are increasing physical activity, improving dietary habits, medication adherence, smoking cessation, and achieving optimal psychosocial wellbeing, thereby reducing their risk of future cardiovascular events [17]. Clinical health recommendations including the targeted values of blood pressure, lipid profile, HbA1C, and dietary suggestions are obtained from the latest published Clinical Practical Guidelines by the Ministry of Health Malaysia [24-27] to ensure its relevance and applicability to our local context. Content providers for SPEM were rehabilitation medicine physicians and residents, cardiac rehabilitation physiotherapists, and occupational therapists.
A group of 8 expert panels including Rehabilitation Physicians, physiotherapists, occupational therapists, a dietician, and a rehabilitation nurse practitioner from various health institutes was invited to evaluate the education material and review its appropriateness. Suggestions obtained were then incorporated into SPEM and subsequently shared back to the expert panel for a final endorsement. SPEM was then shared with a group of CR patients for lay review. The SPEM that was used for this study was the finalized version that has received expert and lay reviews to ensure its accuracy and appropriateness.
Delivery of SPEM
The digital version of SPEM was shared in an online booklet format, via IBIMMA to study participants. The online booklet format provides a smooth page-flip experience to participants as they browse through the pages once they click on the link provided. The content was divided into 5 different chapters and was shared consecutively. The link to the subsequent chapters was only provided once participants self-report completion of reading the earlier chapters. The subjects were encouraged to complete all chapters within 4-6 weeks. The frequency of outpatient appointments with CR providers which is once in 4 weeks, remained unchanged.
Outcomes
Feasibility
Feasibility was assessed by the uptake rate, adherence rate, compliance to CR, and participants’ feedback. Uptake rate is the proportion of eligible participants that agreed to participate in this intervention. Adherence rate is the proportion of participants that completed reading all pages of SPEM within the stipulated duration by self-reporting. CR compliance was assessed by the number of attended monthly scheduled face-to-face follow up, and data were compared between participants that completed SPEM and those that did not. Participants’ feedback was gathered from a close-ended questionnaire mainly to assess their acceptability of the intervention, and open-ended questions to gather their general feedback.
Impact of SPEM
Behavioural and Clinical Outcomes
Smoking status and medication adherence were asked at baseline and monthly until CRP2 completion. Participants were asked to report the likelihood of not taking daily medication as either “never”, “at least once a week”, or “at least once a month”. Compliance to exercise is recorded by an electronic fitness tracker that was provided during enrolment.
Compliance to exercise is assessed by the hours of aerobic exercise per week as recorded by an electronic fitness tracker. The recording of exercise duration starts only when the participant selects the “exercise” button on their tracker and finishes recording when they double select the same button. The data will then be synchronized to their mobile phones using a mobile app that had been pre-installed at the beginning of the program. The action to consciously record their exercise using this feature is significant in highlighting the difference between an exercise and a physical activity, which is often confused.
Cardiorespiratory endurance was measured by a pre/post treadmill exercise stress test (EST), using a modified Bruce protocol. The parameters measured were peak METs values, duration of exercise, and stage completed.
Knowledge and perceived cardiovascular risk, perceived heart-healthy practice benefits and intention
Cardiovascular knowledge and perceived intention to maintain a healthy lifestyle was assessed by using The Attitudes and Beliefs about Cardiovascular Disease (ABCD) Risk Questionnaire developed by Woringer et al. It is a validated questionnaire that combines assessment of cardiovascular risk and prevention knowledge, perceived risk of cardiovascular disease, perceived benefits and intention to change behaviour, and healthy eating intentions, in a single 26-item (2-page) questionnaire [28]. This questionnaire is licensed under Creative Commons Attributions 4.0 International Licence, and written approval for use in this study has been obtained from the author via email. Participants were asked to answer the ABCD Risk questionnaire at the beginning of CRP2, and upon completion at 12 weeks.
Data analysis
Microsoft Excel 365 Version 2110 was used to collate and analyze data. Quantitative data are reported using descriptive statistics, including means (± standard deviations). Due to the small sample size, a statistical analysis comparing the pre-and post- outcome measures was not performed.
Results
Feasibility
Uptake rate, adherence rate, and compliance to CRP2
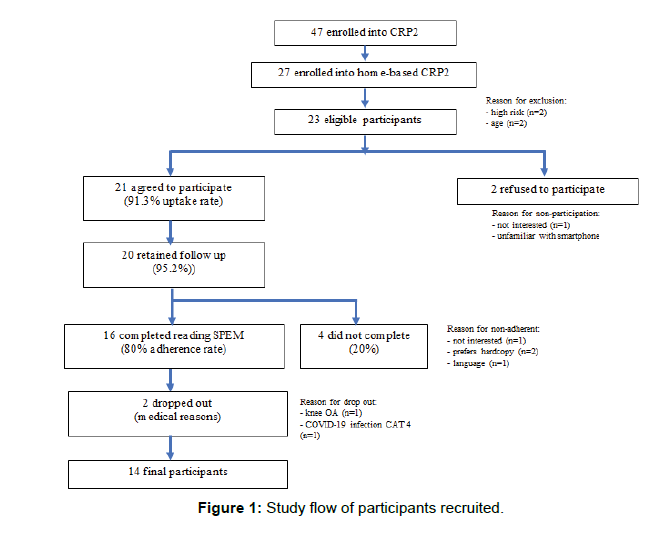
Between March to August 2021, 47 patients were enrolled in the CRP2 program. 27 participants opted for or were assigned to a home-based program; the subject flow is outlined in Figure 1. 4 participants were excluded due to age (n=2) and risk stratified as high risk (n=2). Out of 23 eligible participants, 21 participants agreed to use this intervention and participate in the study (91.3% uptake rate), but 1 was lost to follow-up. All participants that were eligible, offered for this intervention, and participated in this intervention were male.
This study yields an 80% adherence rate whereby 16 out of 20 participants completed reading SPEM by self-reporting. The reasons for non-completing were preference for a hardcopy education material (n=1), work/time conflict (n=1), and 1 participant who is a native Mandarin speaker reported language barrier as the reason for noncompletion. Out of the 16 SPEM completers, 2 dropped out from CRP2 due to medical reasons (n=1 knee osteoarthritis, n=1 active COVID-19 CAT-4 infection). Demographic characteristics of the 14 participants that completed SPEM are outlined in (Table 1).
| Characteristics | n(%) |
|---|---|
| Age (years) | 55.6 (±7.2) |
| Gender | 14 (100) 0 (0) |
| Male Female |
|
| Race | 7 (50) 2 (14.3) 5 (35.7) |
| Malay Chinese Indian |
|
| Working Status | 7 (50) 1 (7.1) 1 (7.1) 1 (7.1) 4 (28.7) |
| Private sector Public sector Self-employed Unemployed Retired |
|
| Education Level | 1 (7.1) 2 (14.3) 11 (78.6) |
| Primary Secondary Tertiary |
|
| Perceived Cardiac Rehab Barrier | 12 (85.7) |
| Concerns regarding COVID-19 | |
| Logistic | 2 (14.3) |
| Co-morbidities | 11 (78.6) 12 (85.7) 13 (92.9) |
| Type II DM Hypertension Dyslipidaemia |
|
| Revascularization procedures | 10 (71.4) 4 (28.6) |
| PCI CABG |
Table 1: Demographic characteristics of participants that completed SPEM (n=14).
With regards to CR compliance, 92.9% of participants that completed the intervention (n=13) completed CRP2, whereas none of the non-SPEM users completed CRP2. None of the participants that completed this intervention reported any major adverse cardiovascular and cerebrovascular events (MACCE) during exercise sessions at home and at the centre.
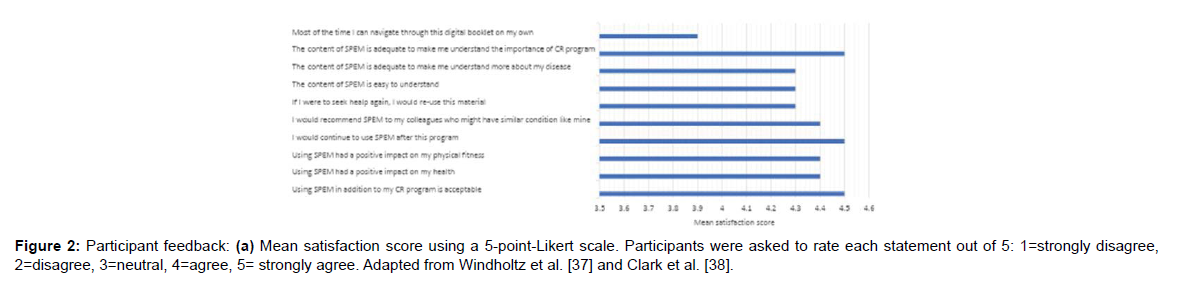
Participants’ Feedback
Most participants agreed that having SPEM delivered via IBIMMA in addition to their CR program is acceptable, brought a positive impact on their health and physical fitness, helped them to better understand their disease and the importance of the CR program, and felt that they would reuse this material and share with others who might have the similar condition (Figure 2a). 3 participants preferred a hardcopy SPEM if they were given the option to choose. General feedback is as outlined in the end of the text.
Impact of Spem
Behavioural and clinical outcomes
Only 2 participants were active cigarette smokers prior to initiation of CRP2, and both reported a significant amount of reduction in the amount of cigarette stick smoked per day at the end of CRP2. 3 other participants abstained from smoking 6 months prior to initiation of CRP2, and all of them remained abstained until the completion of CRP2 (Table 2a).
| Participant | ABCD Risk | No of cigarette smoked per day | Likelihood to miss daily medication | No of exercise hours per week | Number of attended CR sessions (total 3) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Change | Pre | Post | Change | Pre | Post | Pre | Post | ||
| 1 | 64 | 71 | 7 | 30 | 6 | -24 | never | never | 0 | 176.2 | 3/3 |
| 2 | 58 | 61 | 3 | 0 | 0 | 0 | never | never | 0 | 182.5 | 3/3 |
| 3 | 57 | 72 | 15 | 40 | 4 | -36 | Once/ month | never | 0 | 345 | 3/3 |
| 4 | 56 | 57 | 1 | 0 | 0 | 0 | Once/ month | never | 0 | 307.5 | 3/3 |
| 5 | 56 | 62 | 6 | 0 | 0 | 0 | never | never | 0 | 180 | 3/3 |
| 6 | 55 | 62 | 7 | 0 | 0 | 0 | never | never | 0 | 157.5 | 3/3 |
| 7 | 52 | 55 | 3 | 0 | 0 | 0 | Once/ month | never | 0 | 155.25 | 3/3 |
| 8 | 56 | 58 | 2 | 0 | 0 | 0 | never | never | 0 | 105 | 3/3 |
| 9 | 62 | 61 | -1 | 0 | 0 | 0 | never | never | 0 | 145 | 3/3 |
| 10 | 68 | 68 | 0 | 0 | 0 | 0 | never | never | 0 | 197 | 3/3 |
| 11 | 61 | 61 | 0 | 0 | 0 | 0 | never | never | 0 | 97.5 | 3/3 |
| 12 | 55 | 67 | 12 | 0 | 0 | 0 | Once/ month | never | 0 | 77.5 | 3/3 |
| 13 | 59 | 60 | 1 | 0 | 0 | 0 | Once/ week | never | 0 | 117.25 | 3/3 |
| Mean (SD) | 58.4 (4.2) | 62.7 (5.1) | 4.3 (4.7) | - | - | - | - | - | 0 (0) | 163.2 (79.4) | - |
Table 2(a): Summary of outcome assessments: (a) ABCD risk scores and behavioural outcomes (smoking status, medication adherence, weekly hours of exercise) and CR compliance (total attended CR face-to-face sessions).
In relation to medication adherence, 5 participants reported some degree of likelihood to miss their daily medication at the beginning of CRP2 and most of them reported improvement in this behaviour at the end of CRP2. All other participants that reported “never” to miss their daily medication for the past 1 month maintained this behaviour throughout the 12-week follow-up (Table 2a).
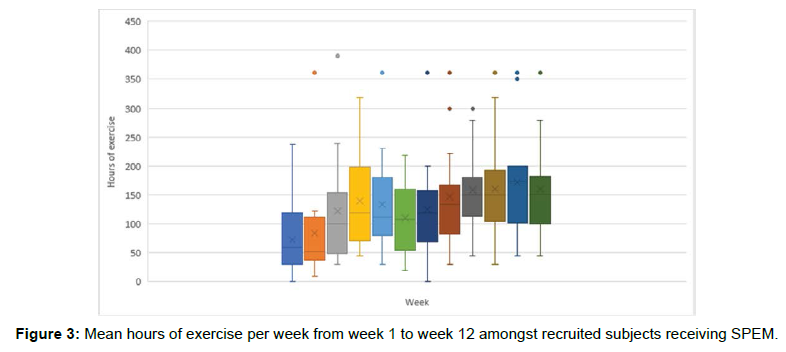
Generally, all participants recorded an improvement in hours of exercise per week throughout the 12-week duration, and 57% (n=8) achieved the recommended exercise duration of a minimum of 150 minutes per week (Table 2a, Figure 3). 1 participant was unable to perform the post-exercise stress test due to logistic reasons, hence excluded for comparison. Overall, there was observed improvement of all cardiorespiratory endurance parameters including peak METs (mean change 1.3 ± 1.4), exercise duration (mean change 94.2 seconds ± 85.5), and stage completed (mean change 0.7 ± 0 .7) as summarised in (Table 2b).
| Participant | No of exercise hours per week | Endurance parameters measured by treadmill exercise stress test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Peak METs value | Exercise duration (sec) | Stage completed | ||||||||||
| Pre | Post | Pre | Post | Change | Pre | Post | Change | Pre | Post | Change | ||
| 1 | 0 | 176.2 | 10.1 | 11.1 | 1 | 901 | 919 | 18 | 5 | 5 | 0 | |
| 2 | 0 | 182.5 | 10.1 | 10.1 | 0 | 901 | 902 | 1 | 5 | 5 | 0 | |
| 3 | 0 | 345 | 10.1 | 10.1 | 0 | 794 | 901 | 107 | 4 | 5 | 1 | |
| 4 | 0 | 307.5 | 7 | 7 | 0 | 643 | 720 | 77 | 3 | 4 | 1 | |
| 5 | 0 | 180 | 10.1 | 10.1 | 0 | 811 | 902 | 91 | 4 | 5 | 1 | |
| 6 | 0 | 157.5 | 10.1 | 10.4 | 0.3 | 804 | 890 | 86 | 4 | 4 | 0 | |
| 7 | 0 | 155.25 | 7 | 10.1 | 3.1 | 710 | 785 | 75 | 3 | 4 | 1 | |
| 8 | 0 | 105 | 7 | 10.1 | 3.1 | 721 | 789 | 68 | 4 | 4 | 0 | |
| 9 | 0 | 145 | 3.5 | 4.8 | 1.3 | 330 | 512 | 182 | 1 | 2 | 1 | |
| 10 | 0 | 197 | 12.8 | 12.4 | -0.4 | 962 | 942 | -20 | 5 | 5 | 0 | |
| 11 | 0 | 97.5 | 7 | 10.4 | 3.4 | 657 | 907 | 250 | 3 | 5 | 2 | |
| 12 | 0 | 77.5 | 7 | 10.4 | 3.4 | 636 | 901 | 265 | 3 | 5 | 2 | |
| 13 | 0 | 117.25 | 10.1 | 11.5 | 1.4 | 901 | 926 | 25 | 5 | 5 | 0 | |
| Mean (SD) | 0 (0) | 163.2 (79.4) | 8.6 (2.3) | 9.9 (1.9) | 1.3 (1.4) | 751.6 (160.2) |
845.8 (115.5) |
94.2 (85.5) |
3.8 (1.1) |
4.5 (0.8) |
0.7 (0.7) |
|
Table 2(b): Summary of outcome assessments: (b) Exercise hours and endurance parameters.
Knowledge and perceived cardiovascular risk, perceived heart-healthy practice benefits and intention
The ABCD-Risk Questionnaire showed a mean total score improvement by 4.3 (±4.7), with the greatest mean change noted in the perceived CV risk section (mean change 3 ± 4.5), followed by CV knowledge (mean change 0.7 ± 0.8). There was no change in the perceived benefits and intention section. 1 participant did not complete the post-test assessment, hence excluded from the summarised result.
Unsurprisingly, participants that had marked improvement in the ABCD-risk score showed positive improvement in the behavioural outcomes. For instance, Participant 3 which scored the highest ABCD-risk score improvement also showed a marked reduction in the number of cigarettes smoked per day, improvement in medication adherence, and the greatest improvement in exercise hours per week (Table 2a).
Discussion
Principal Findings
This study shows that it is feasible and acceptable to deliver education material via IBIMMA to CR participants. 98.7% out of 2400 Malaysian respondents in an online survey in 2020 stated that “Whatsapp” is their favourite instant messaging mobile app [29], and had been reported as an important, and heavily relied-on communication tool by Malaysians during movement restriction orders due to COVID-19 pandemic [30]. A recent cross-sectional study to examine attitudes, perceptions, and behavioural intentions toward remote digital CR revealed that 86% of participants preferred communication channel was through text messaging, followed by e-mail and video clips (40% each), whereby half wanted to receive up to two messages a week, and almost a quarter was interested in daily text messages [31]. Therefore, the utilization of a commonly used internet-based instant messaging app as a medium to deliver information, and to a certain extent as a remote monitoring medium can be further optimized in the delivery of home-based CR programs. In addition, IBIMMA-sharing education material is simple and convenient, and bypasses the need to install a separate mobile application and minimizes the possibilities of users’ technical difficulties. The technical difficulty and the need for user training have been described as potential barriers to utilizing certain telemedicine devices in a previous study [32]. Bypassing the need for user training may be one reason for this study’s high acceptability rate. However, the main limitation of this method is the requirement of a smartphone with a stable cellular network. Utilizing this intervention in remote areas with poor network coverage will be a challenge. The mean age of the study sample is below 60; hence it is difficult to determine its impact in the older age group, which has been described in a previous study as less technology-literate [31]. Some participants preferred to be given the option to choose between a digital SPEM or printed SPEM, hence this should be considered in future studies.
This study also reveals higher adherence to home-based CRP2 among SPEM-completers, compared to non-completers. Although the majority of SPEM-completers rated concerns regarding COVID-19 as their biggest perceived barrier to the CR program (Table 1) that did not lead to non-compliance to scheduled CR follow-ups. In contrast, none of the non-completers successfully graduated from CRP2. Possible contributors to this high adherence are the emphasis of CR compliance and heart-healthy behaviour targets outlined in SPEM, the direct telecommunication during SPEM delivery via IBIMMA, and the incorporation of activity monitoring using a fitness tracker as part of the study. A Cochrane review in 2014 of interventions to improve CR adherence included activity monitoring with daily entries, goal setting, and telephone communication as possible solutions [33]. However, due to these multiple contributing factors, it is difficult to determine which is the strongest contributor, hence a controlled study is needed to determine this.
Overall, there is improvement in all behavioural parameters, with the greatest improvement noted in compliance to home exercise. Interestingly, improved compliance to exercise is also reflected in improved cardiorespiratory endurance parameters, especially in increased EST exercise duration and the stage completed. This suggests that despite the enforcement of public health measures (movement restriction orders, physical and social distancing) compliance to a healthy lifestyle can be maintained by providing education material via a commonly used mobile phone application. Although some of the participants did not meet the recommended exercise duration of 150 minutes/week, all succeeded to maintain a weekly exercise. This is an encouraging achievement considering they had reduced physical interaction with CR providers, and only 1 participant had a pre-existing habit of regularly exercising while the rest was pre-morbidly sedentary. This finding is indeed promising given the cardio metabolic effects of exercise are related to reduced mortality in cardiovascular patients [11]. Engagement with technology-enabled CR intervention in a previous study has shown better adherence to lifestyle behaviours among home-based CR participants which suggests the presence of a greater sense of responsibility for own health [34]. However, the fact that all participants adhered to all scheduled face-to-face follow-ups may also contribute to this positive behaviour outcome hence a controlled study is needed to determine this.
With regards to the pre/post comparison of ABCD-Risk scores, there was a wide range of score changes between participants. The greatest change noted is in the perceived CV risk section, indicating that most participants have increased awareness of their risks of getting a secondary cardiac event. Health-related risk perceptions play a role in motivating health behaviour change [35], hence interventions that can bring change to risk perceptions may subsequently change health behaviour.
Strengths and Limitations
Most studies involving home-based CR participants were carried out in developed countries. This study is the first to be carried out in Malaysia, which is a middle-income country, and findings may be relatable to many other lower to middle-income nations. Most studies involving an education intervention did not include endurance as an outcome. This pilot study included an objective cardiorespiratory endurance measurement, as an initial attempt to capture the correlation between a change in knowledge and good intentions to actual clinical outcomes.
The main limitation of this study is the study design. A further randomized controlled trial is needed to ascertain the effectiveness of SPEM in improving the above outcomes among HBCR participants. Subsequent comparison to CBCR participants not receiving the intervention is needed to assess if this intervention is comparable to the standard care (centre-based CR). Secondly, study participants were mostly well-educated, who attended CR program at a university hospital in an urban setting. The highest educational attainment and socioeconomic background were not controlled in this study; therefore, the results may not be representative of the larger population. In addition, during this study recruitment, no female patient was eligible and recruited, emphasizing the unique issues revolving around female patients in cardiac rehabilitation [36], hence further studies are needed to explore further on referral, enrolment, and participation of cardiac rehabilitation among this specific population.
A longer follow up, preferably 3- and 6-months post completion of CRP2 is needed to ascertain the effectiveness of this intervention to promote long-term behaviour change towards a healthy lifestyle hence CV reduction risks [37-38].
Clinical Implications
This study could be a groundwork for the development of telemedicine in a home-based rehabilitation program for future use and can be readily utilized should a health emergency like the current Covid-19 pandemic arise again. Provision of CR program to all Malaysian economic strata which was previously limited by a geographical barrier, e.g., distance from CRP centres exceedingly more than 20km; demographic barrier, for example, those of lowerincome group defaulted due to time and financial commitment or elderly population depending on others to attend hospital visits, could hopefully be improved. In addition, decentralization of CR services from the hospital overcomes age and gender-specific issues often seen in mix-age or mix-gender therapy sessions.
Conclusion
Providing digital education material via an internet-based instant messaging app is feasible, and yields a positive impact on CR compliance, behavioural and clinical outcomes, cardiovascular risk knowledge, perceived cardiovascular risks, and perceived intention to practice a heart-healthy lifestyle. Future controlled, randomized studies can elucidate to the effectiveness of this intervention and applicability of its effects.
Acknowledgements
The authors would like to express their gratitude to the staff of the Cardiac Rehabilitation Services and the Rehabilitation Medicine Clinic of University Malaya Medical Centre for their assistance in this study. This study received funding from the UMSC C.A.R.E Fund Research Grant (PV019-2020).
Funding
This study was funded by the UMSC C.A.R.E Fund Research Grant (PV019- 2020).
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors Contribution
Conceptualization, A.S. and A.F.N.; methodology, A.S. and L.W.L.; software, K.D.V & E.R.M.F.; validation, A.F.N., L.W.L. and A.S.; formal analysis, A.F.N.; resources, A.S.; data curation, A.F.N. & E.R.M.F.; writing—original draft preparation, A.F.N.; writing—review and editing A.S.; visualization, A.F.N.; supervision, A.S.; project administration, L.W.L.; funding acquisition, A.S. All authors have read and agreed to the published version of the manuscript.
Participant feedback: Participants’ general feedback from an open-ended question.
General feedback from participants
• “This education material helps me to understand about my health condition better”
• “What I like the most about this education material is the ease of understanding the information. The colourful graphic made reading interesting”
• “I like it as I can access the information at anytime and anywhere”
• “This education material that I received helps me to understand the risk of a recurrent attack”
• “I would like to suggest participants given an option to choose from a digital version or a printed version”
• “I feel this education material should be shared to many others; in fact, I have started to share this education material to my friends”
• “I would suggest a downloadable PDF version of this file is also offered to us”
References
- Health Data (2019) Malaysia Institute for Health Metrics and Evaluation 2019. 2013:1–9.
- Mohd Uzir Mahidin (2020) Department of Statistics Malaysia Press Release: Statistics on Causes of Death, Malaysia, 2020. Dep Stat Malaysia 2020: 1–8.
- Abbafati C, Abbas KM, Abbasi-Kangevari M, Michael RM Abrigo, Jaimie DA, et al. (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396: 1204–1222.
- Ministry of Health Malaysia (2015) Ministry of Health Malaysia. Heal Facts2015:1–19.
- Zheng C, Huang WY, Sheridan S, Cindy Hui-Ping S, Xiang-Ke C, et al. (2020) COVID-19 pandemic brings a sedentary lifestyle: a cross-sectional and longitudinal study. Int J Environ Res Public Health.
- Stockwell S, Trott M, Tully M, Shin J, Barnett Y, et al. (2021) Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med 7:1–8.
- O’Gara PT, Kushner FG, Ascheim DD, Chung MK, Ettinger SM, et al. (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American college of cardiology foundation/american heart association task force on practice guidelines. J Am Coll Cardiol 61: 78–140.
- Levine GN, Bates ER, Blankenship JC, Bittl JA, Cercek B, et al. (2011) 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 124: 574–651.
- Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, et al. (2012) 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: Executive summary. J Thorac Cardiovasc Surg 143: 4–34.
- Smith SC, Bonow RO, Hutter AM (2007) AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update. ACC Cardio source Rev J 16: 60–2.
- Heran BS, Chen JM, Ebrahim S, Moxham T, Oldridge N, et al. (2011) Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev.
- Bellmann B, Lin T, Greissinger K, Rottner L, Rillig A, et al. The Beneficial Effects of Cardiac Rehabilitation. Cardiol Ther 9: 35-44.
- Balady GJ, Ades PA, Bittner VA, Franklin BA, Gordon NF, et al. (2011) Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: A presidential advisory from the American Heart association. Circulation 124: 2951–2960.
- NACR (2019) The National Audit of Cardiac Rehabilitation: Annual Statistical Report. Natl Audit Card Rehabil.
- Poh R, Ng HN, Loo G, Yeo TJ, Wong R, et al. (2015) Cardiac Rehabilitation after Percutaneous Coronary Intervention in a Multiethnic Asian Country: Enrollment and Barriers. Arch Phys Med Rehabil 96: 1733–1738.
- K Jolly, R Taylor, GYH Lip, S Greenfield, J Raftery, et al. (2007) Business 11.
- Thomas RJ, Beatty AL, Beckie TM, Brewer LC, Brown TM, et al. (2019) Home-Based Cardiac Rehabilitation: A Scientific Statement From the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 140: e69–e89.
- Imran HM, Baig M, Erqou S, Taveira TH, Shah NR, et al. (2019) Home-Based Cardiac Rehabilitation Alone and Hybrid With Center-Based Cardiac Rehabilitation in Heart Failure: A Systematic Review and Meta-Analysis. J Am Heart Assoc 8: e012779.
- Turk-Adawi K, Supervia M, Lopez-Jimenez F, Pesah E, Ding R, et al. (2019) Cardiac Rehabilitation Availability and Density around the Globe. EClinicalMedicine 13: 31–45.
- Yang CT, Suhaimi A, Wan Mohamad Akbar SH (2018) Perceived Barriers to Cardiac Rehabilitation Participation Amongst Cardiac Patients in A Malaysian Tertiary Care Hospital.
- Ghisi GL de M, Abdallah F, Grace SL, Thomas S, Paul Oh, et al. (2014) A systematic review of patient education in cardiac patients: Do they increase knowledge and promote health behavior change? Patient Educ Couns 95:160–174.
- Anderson L, Brown JPR, Clark AM, Dalal H, Rossau HK, et al. (2017) Patient education in the management of coronary heart disease. Cochrane Database Syst Rev 6.
- Rehabilitation AA of C and P (2013) Guidelines for Cardiac Rehabilitation and Secondary Prevention Programmes.
- Ministry of Health Malaysia (2017) Clinical Practice Guidelines on Primary & Secondary Prevention of Cardiovascular Disease 2017.
- Ministry of Health Malaysia (2019) Clinical Practice Guideline Management of Acute ST Segment Myocardial Infarction (STEMI) 2019. 4thedn.
- Ministry of Health Malaysia (2017) Clinical Practice Guideline Management of Dyslipidaemia 2017. 5thedn.
- Ministry of Health Malaysia (2020) Clinical Practice Guideline Management of Type 2 Diabetes Mellitus 2020 6th Edition. 6thedn.
- Woringer M, Nielsen JJ, Zibarras L, Evason J, Kassianos AP, et al. (2017) Development of a questionnaire to evaluate patients’ awareness of cardiovascular disease risk in England’s National Health Service Health Check preventive cardiovascular programme. BMJ Open 7.
- Malaysia: internet users using communication apps 2020 (2020) Statista.
- Karim MFSA, Bakar MSA (2021) Functions, Influences & Effects of WhatsApp Use During the Movement Control Order (MCO) in Malaysia. Asian Soc Sci 17: 24.
- Nabutovsky I, Nachshon A, Klempfner R, Shapiro Y, Tesler R, et al. (2020) Digital Cardiac Rehabilitation Programs: The Future of Patient-Centered Medicine. Telemed J E Health 26: 34–41.
- Paul DL, Pearlson KE, McDaniel RR (1999) Assessing technological barriers to telemedicine: Technology-management implications. IEEE Trans Eng Manag 46: 279–288.
- Karmali KN, Davies P, Taylor F, Beswick A, Martin N, et al. (2014) Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev.
- Claes J, Filos D, Cornelissen V, Chouvarda I (2019) Prediction of the Adherence to a Home-Based Cardiac Rehabilitation Program. Annu Int Conf IEEE Eng Med Biol Soc2019:2470–2473.
- Sheeran P, Harris PR, Epton T (2014) Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull 140: 511–543.
- Mamataz T, Ghisi GLM, Pakosh M, Grace SL (2021) Nature, availability, and utilization of women-focused cardiac rehabilitation: a systematic review. BMC Cardiovasc Disord 21: 459.
- Windholz T, Swanson T, Vanderbyl BL, Jagoe RT, et al. (2014) The feasibility and acceptability of neuromuscular electrical stimulation to improve exercise performance in patients with advanced cancer: A pilot study. BMC Palliat Care 13:23.
- Clark RA, Fredericks B, Buitendyk NJ, Adams MJ, Dracup KA, et al. (2015) Development and feasibility testing of an education program to improve knowledge and self-care among Aboriginal and Torres Strait Islander patients with heart failure. Rural Remote Health 15: 3231.
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google scholar Crossref
Indexedat Google scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Citation: Suhaimi A, Ngimron AF, Ling LW, Varathan KD, Faizal ERM (2022) The Impact of Digital Education Material in Improving Clinical and Behavioural Outcomes in Home-Based Cardiac Rehabilitation Participants: A Pilot Study. J Card Pulm Rehabi 6: 153. DOI: 10.4172/jcpr.1000153
Copyright: © 2022 Suhaimi A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3039
- [From(publication date): 0-2022 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 2503
- PDF downloads: 536