The Impact of Antithrombotic Medication on Uteroplacental Blood Flow in Patients with Previous Obstetric History of Placental Mediated Disorders
Received: 24-Aug-2018 / Accepted Date: 25-Sep-2018 / Published Date: 02-Oct-2018 DOI: 10.4172/2376-127X.1000391
Keywords: Placental mediated disorders; Antithrombotic medication; Uteroplacental blood flow; Pregnancy
Abbreviations
PMD: Placental Mediated Disorders; PI: Pulsatility Index; UtAs: Uterine Arteries; AM: Antithrombotic Medication; UtADIs: Uterine Artery Doppler Indices; SG: Study Group; CG1: Control Group 1; CG2: Control Group 2; PE: Pre-eclampsia; IUGR: Intrauterine Growth Restriction; PA: Placental Abruption; LDA: Low Dose Aspirin; LMWH: Low Molecular Weight Heparin; UtAPI: Uterine Artery Pulsatility Index; 95c: Ninety-Fifth Centile; TI: Trophoblastic Invasion; DI: Doppler Index; IUFD: Intrauterine Fetal Death; CD: Colour Doppler; G.a:. Gestational age; G.w.: Gestational week.
Introduction
Placenta-Mediated Diseases (PMD) include early-onset Preeclampsia (PE), which develops before 34 gestational weeks (g.w.), Intrauterine Growth Restriction (IUGR), Placental Abruption (PA) and Intrauterine Fetal Death or stillbirth (IUFD). The recurrence rate of PMD in subsequent pregnancies is particularly high [1,2]. It is believed that abnormal Trophoblastic Invasion (TI) of the spiral arteries plays a major role in the pathogenesis of PMD, leading to placental hypoperfusion [1,3]. Abnormal TI is the underlying reason for the elevated Doppler Indices (DI) in the Uterine Arteries (UtAs). Thus, abnormal UtADIs constitute a major indicator of pathologic spiral artery remodelling [4,3]. According to a lot of research abnormal values of uterine artery DIs, especially the Pulsatility Indices (PIs), have good predictive value for the identification and follow-up of pregnancies at high risk for the development of such PMD [1,2,5].
High PIs above the 95th centile (>95c) in one or both UtAs can be detected far before the clinical manifestation of PMD. Thus, DI measurements are nowadays an integral part of the first trimester combined screening for chromosomal defects - 11-14th gestational week (g.w.). The combined assessment of biophysical and biochemical markers allows the identification of pregnant women at high risk for the development of earlyonset PE (before 34 g.w.) and IUGR. Doppler assessment of the uterine arteries in the third trimester of pregnancy, according to some studies, might be helpful in identifying pregnancies at a risk for late PE or IUGR and therefore unfavorable perinatal outcome [6].
A lot of studies were performed during the last two decades on the role of Antithrombotic Medication (AM) either with Low-Dose Aspirin (LDA) alone or with Low-Molecular Weight Heparin (LMWH) or the combination of both for the prevention of PMD. The beneficial effect was mainly attributed to the antithrombotic function of these medications. Later, it was hypothesized that AM may interfere with TI enhancing it and thus preventing the subsequent development of PMD. However, there is still a lot of controversy in this area and opinions of researchers as to the type and dosage of AM vary [1,2,7,8].
The aim of our study was to assess UtAPIs in pregnant women on different types of AM, administered because of a history of previous pregnancy with PMD. Our hypothesis was that AM could enhance TI, thus leading to decreased impedance to flow in the UtAs, resulting in increased proportion of cases with bilaterally normal UtAPIs and decreased proportion of cases with bilaterally abnormal UtAPIs or mean PIs>95c in the study group of patients (SG).
Materials and Methods
Our research was a cohort one including 647 patients, divided in a Study Group (SG) and two Control Groups (CGs). The SG included 169 patients, who received different types of AM because of a past history of PMD. PMD included early-onset PE, IUGR, PA and/or IUFD. The SG was additionally subdivided into three subgroups according to the type of AM applied. The 169 patients from the SG were either on LDA (subgroup 1), on LMWH (subgroup 2) or on combination of LDA and LMWH (subgroup 3). 44/169 (26%) of the patients in the SG received LDA (100 mg/day), 74/169 (44%) received LMWH (nadroparin calcium at a dosage of 0.4/0.6 mL sec/day or enoxaparin sodium x 0.4 mL sec/ day) and 51/169 patients (30%) received both LDA and LMWH.
The first CG (CG1) included 158 patients who like the patients in the SG had a history for previous PMD, but were not on AM. The second CG (CG2) included 320 patients with uncomplicated previous pregnancies and on no AM.
The following three indicators were analyzed in the SG: (1). The proportion of bilaterally normal PIs in the UtAs below the 95th centile, (2). The proportion of cases with bilaterally abnormal PIs in the UtAs above the 95th centile, (3). The proportion of cases with mean PIs in the UtAs above the 95th centile, according to the gestational age (g.a.). They were compared to the corresponding indicators in the CG1 and the CG2. The same parameters were also compared between the three subgroups of the SG.
Pulsatility Indices (PIs) in the uterine arteries were measured trans abdominally. The ultrasound transducer was placed in the lower lateral abdominal area with a slight medial tilt. UtAs were identified using Colour Doppler (CD) at the level of the crossing with the external iliac artery. Doppler Indices (DIs) were measured at a minimal angle of insonnation of the vessel of interest, according to the ISUOG criteria, 2013. The sample volume was adjusted according to the studied vessel diameter. Additional adjustment of the filter and PRF settings was also performed [8]. Samsung-Medison-Accuvix A30 and A35 equipment was used. PI values in the UtAs above the 95th centile for the g.a. were defined as elevated. PI values in the UtAs below the 95th centile were defined as normal for the g.a. [9].
The analysis of the results were performed by the Student’s t-test. Statistical significance was admitted with p<0.05.
Results
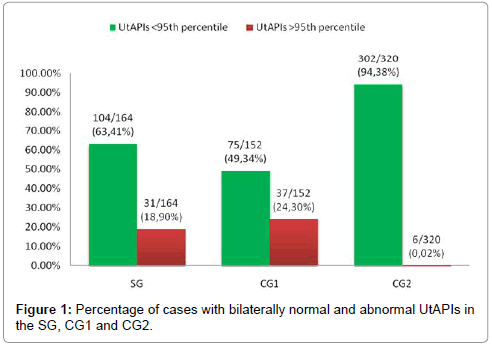
Normal PIs in both UtAs<95c were found in 104/164 (63.41%) of the patients in the SG on AM because of previous PMDs. There was lack of information regarding UtAPIs in 5 out of 169 patients from the SG. Normal DIs were significantly less frequent in the CG1-75/152 (49.34%) of the patients (p<0.05). There was lack of information regarding UtAPIs in 6 out of 158 patients from the CG1. The percentage of cases with bilaterally normal UtAPIs in the SG -104/164 (63.41%) of the patients, was even more significantly lower as compared to the one in the CG2-302/320 (94.38%) of the patients, p<0.0001 (Figure 1).
There was no statistically significant difference between the SG - 31/164 (18.9%) of the patients and the CG1 - 37/152 (24.3%) of the patients, regarding bilaterally abnormal UtAPIs>95c, (p>0.05). The cases with bilaterally abnormal UtAPIs>95c in the SG-31/164 (18.9%) of the patients, were significantly more frequent in comparison to the ones in the CG2 (6/320-0.018%), p<0.0001 (Figure 1).
The results from the present study including 169 patients with previous PMD receiving AM (SG) and 158 patients with the same history but without medication (CG1) showed a statistically significant increase in the percentage of bilaterally normal UtAPIs<95c in the SG as compared to the CG1. Nevertheless, the percentage of cases with bilaterally normal UtAPIs<95c in the SG stayed significantly lower in comparison to that percentage in the CG2 with previous uncomplicated pregnancies and on no AM. The results from the present study showed tendency towards a decrease in the percentage of cases with bilaterally abnormal UtAPIs>95c in the SG as compared to the CG1, but the difference was not statistically significant. Nevertheless, the percentage of cases with bilaterally abnormal UtAPIs>95c stayed significantly higher in the SG in comparison to the CG2.
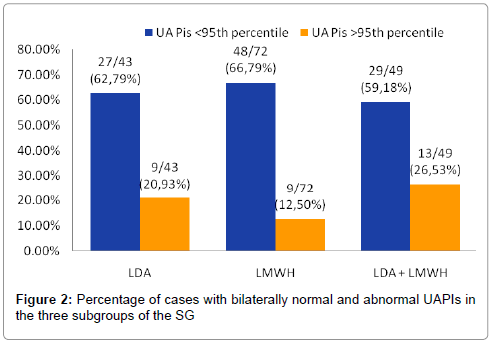
The analysis of the different subgroups in the SG showed that there was no statistically significant difference in the percentage of cases with bilaterally normal UtAPIs<95c (p>0.05). We observed normal DIs in both UtAs in 27/43 (62.79%) of the patients in subgroup 1 on AM only with LDA, in 48/72 (66.79%) of the patients in subgroup 2 on AM only with LMWH and in 29/49 (59.18%) of the patients in subgroup 3 receiving both LDA and LMWH, p>0.05. There was lack of information regarding UtADIs in one case from subgroup 1, in 2 cases from subgroup 2 and in 2 cases from subgroup 3 (Figure 2).
There was no statistically significant difference among the three subgroups of the SG regarding the percentage of cases with bilaterally abnormal UtAPIs. UtAPIs>95c were found in 9/43 (20.93%) of the patients in subgroup 1 on AM only with LDA, 9/72 (12.5%) of the patients in subgroup 2 on AM only with LMWH and 13/49 (26.53%) of the patients in subgroup 3 receiving combined AM with LDA and LMWH, p>0.05 (Figure 2).
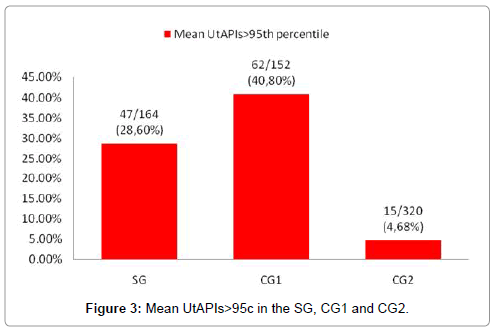
The percentage of cases with mean UtAPIs>95c was significantly lower in the SG-47/164 (28.6%) of the patients, as compared to the CG1-62/152 (40.8%) of the patients, p<0.05. However, the percentage of cases with mean UtAPI>95c in the SG was significantly higher in comparison to the CG2-15/320 (4.68%) of the patients, respectively (Figure 3).
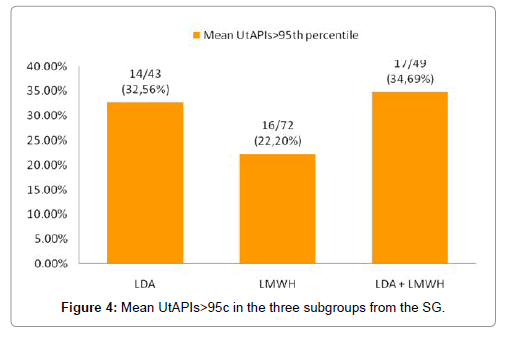
In addition, we found no statistically significant difference in the three subgroups of the SG on different AM regarding the proportion of cases with elevated mean UtAPIs>95c, p>0.05. Mean PIs>95c was observed in 14/43 (32.56%) of the patients in subgroup 1 on AM only with LDA, in 16/72 (22.2%) of the patients in subgroup 2 only on LMWH and in 17/49 (34.69%) of the patients in subgroup 3 on combined therapy with LDA and LMWH (Figure 4).
The percentage of cases with mean UtAPIs>95c in the SG was significantly lower than the one in the CG1. This effect did not seem to depend on the type of AM, since all the studied parameters in the subgroups on LDA or LMWH alone or on combination of both were similar (Figures 3 and 4).
Discussions
There are a lot of studies on UtADI assessment. Sekizuka et al. were the first authors to define the term Uterine Arteries Score (UAS), studying uterine arteries’ Resistance Indices (RI) in their research [10]. The term UAS was later on modified by Hernandez-Andarde et al. who studied PIs instead of RIs in their study [11]. They analyzed 741 high-risk cases in the third trimester of pregnancy. They assessed PIs, bilaterally, as well as the presence or absence of a diastolic notch. Those two parameters comprised the term UAS, which was assigned 0 to 4 points, according to the typical Doppler findings. When both UtAPIs were normal and there were no diastolic notches, the UAS was 0. The UAS was assigned 4 points when there were bilaterally elevated UtAPIs together with persistent diastolic notches in both UtAs [10,11]. Hernandes-Andarde et al. found in their research, that UAS higher than 2 points in the third trimester of pregnancy was related to a siginificantly increased risk for Preterm Birth (PB), longer Neonatal Intensive Care Unit (NICU) stay, increased frequency of operative delivery due to fetal distress, 5 min APGAR scores below 7, greater risk for the delivery of a Small-for-Gestational Age (SGA) newborn [11]. Thus, UAS appeared to be a good predictive risk factor for poor perinatal outcome.
According to the results of Geerts et al. abnormal PIs in both UtAs were found in 98.2% of the cases with early-onset PE between 24-34 gestational weeks (g.w.) [5]. According to another research on 60 high-risk pregnancies, already complicated by early-onset severe PE and IUGR, DIs in the last trimester of pregnancy remained abnormal in 87% of the cases [12]. However, a third research by Gudnason et al. comprising 570 pregancies complicated by PE, showed abnormal UtADIs values in the third trimester of pregnancy in only 25% of the cases. Those were the cases related to severe PE. The percentage of cases with unfavorable perinatal outcome was lower in the cases with bilaterally normal UADIs [13]. Another prospective cohort research compared 40 pregnancies at high risk for the development of IUGR and PE, with 40 normally developing pregnancies [6]. It was proven that abnormal UtADIs had a better prognostic value regarding the possibility of adverse perinatal outcome, compared to abnormal UmbADIs only, as the first ones appeared to identify cases with poor placental vascularisation more precisely [6,9]. In a study of Vergani et al. in 2002, 109 pregnancies, complicated by IUGR were compared to 185 normally developping pregnancies. In the presence of abnormal UtADIs at term there was a 4-fold increase in the risk of poor perinatal outcome [14]. Joern et al. recommended as mandatory the evaluation of UtADIs in high-risk pregnancies [10].
In our research we studied the effect of AM with LDA or LMWH alone or a combination of both on UtAPIs in pregnant women with previous history of PMD. There is little information in literature concerning this matter. In a study carried out in 2001 on 65 such pregnancies, Bar et al. observed some improvement of UtADIs in the group on combined AM with LMWH and LDA, compared to the group on AM only with LDA [7]. According to another research performed by Mello et al. in 2005 AM only with LMWH appeared to have some beneficial effect on recurrent PE development in consecutive pregnancies [15]. In 2017 we conducted a small preliminary study with the same design as the present one on 69 patients on various types of AM due to previous history with PMD-the Study Group (SG). The first CG (CG1) included 47 patients with previous history of PMD but no AM in the current pregnancy. The second CG (CG2) included 78 patients with previous uncomplicated pregnancies, with no history of PMD and no AM. In general, due to the small number of cases, the results were somewhat controversial and inconclusive. Our preliminary results showed that pregnant women with a history of PMD, irrespective of whether they are on AM or not, tend to have significantly more frequent bilateral abnormal UtAPIs compared to women with previous uncomplicated pregnancies. The different types of AM in the particular dosage in the SG with a history of PMD did not seem to improve uteroplacental blood flow in the second and third trimester of pregnancy compared to the control group with similar obstetric history, but with no AM, nor to the control group with previous uncomplicated pregnancies. Therefore, we decided to continue our research and to increase the number of the studied patients [16].
The results from the present study including 169 patients with previous PMD receiving AM (SG) and 158 patients with the same history but without medication (CG1) did not show a statistically significant decrease in the percentage of bilaterally abnormal UtAPIs as compared to the CG1 of 158 patients. The percentage of cases with mean UtAPIs>95c in the SG was, however, significantly lower than the one in the CG1. This effect did not seem to depend on the type of AM, since all the studied parameters in the subgroups on LDA or LMWH alone or on combination of both were similar. The differences between the proportion of cases with bilaterally normal, bilaterally abnormal or mean UtAPIs>95c were also not statistically significant when comparing the three subgroups. Despite the AM, uteroplacental blood flow in the SG of women was significantly more frequently abnormal when compared to the one in women with previous uncomplicated pregnancies without PMD-the CG2.
The results from our study indicate that AM with LDA, LMWH or a combination of them in pregnant women with previous pregnancies complicated with PMD does not contribute significantly to the improvement of uteroplacental circulation, compared to pregnant women with the same obstetric history but no AM in the current pregnancy. AM in pregnancies with a previous history of PMD, applied in the specified doses, did not seem to have a significant beneficial effect on UtAPIs and TI, respectively. Pregnant women with previous PMD, even when on AM, tend to have abnormal uteroplacental blood flow significantly more frequently than patients with previous normal pregnancies. Further prospective studies need to be performed in order to better clarify the effect of diverse types of AM on UtADIs, with respect to the different types of preparations, the dose regimens and onset of therapy together with a longitudinal followup of UtADIs in the course of pregnancy.
Conclusion
As per the observation, by going through above obtained result, AM has less effective in trophoblastic invasion in the SG, while CG1 has more effective trophoblastic invasion. Thus, AM does not seem to improve trophoblast invasion in the SG compared to CG1.
References
- Barton JR, Sibai BM (2008) Prediction and prevention of recurrent preeclampsia. Obstet Gynecol 112: 359-372.
- Bramham K, Briley AL, Seed P, Poston L, Shennan AH, et al. (2011) Adverse maternal and perinatal outcomes in women with previous preeclampsia: A prospective study. Am J Obstet Gynecol 204: 512.e1-9.
- Yinon Y, Kingdom JCP, Odutayo A, Moineddin R, Drewlo S, et al. (2010) Vascular dysfunction in women with a history of preeclampsia and intrauterine growth restriction. Circulation 122: 1846-1853.
- Gomez O, Figueras F, Fernandez S, Benassar M, Martinez JM, et al. (2008) Reference ranges for uterine artery mean pulsatility index at 11-41 weeks of gestation. Ultrasound Obstet Gynecol 32: 128-132.
- Geerts L, Odendaal HJ (2007) Severe early onset pre-eclampsia: Prognostic value of ultrasound and Doppler assessment. J Perinatol 27: 335-342.
- Reddy A, Malik R, Mehra S, Singh P, Ramachandran L (2015) Correlation of doppler studies at 34 weeks of gestation with perinatal outcome in high risk pregnancies. IJRCOG 4: 1894-1899.
- Bar J, Mashiah R, Cohen-Sacher B, Hod M, Orvieto R, et al. (2001) Effect of thrombophylaxis on uterine and fetal circulation in pregnant women with a history of pregnancy complications. Thromb Res 101: 235-241.
- ISUOG (2013) ISUOG practice guidelines: Use of Doppler ultrasonography in obstetrics. Ultrasound Obstet Gynecol 41: 233-239.
- Joern H, Rath W (1998) Comparison of Doppler sonographic examinations of the umbilical and uterine arteries in high-risk pregnancies. Fetal Diagn Ther 13: 150-153.
- Sekizuka N, Hasegawa I, Takakuwa K, Tanaka K (1997) Scoring of uterine artery flow velocity waveform in the assessment of fetal growth restriction and/or pregnancy induced hypertension. J Matern Fetal Invest 7: 197-200.
- Hernandez-Andrade E, Brodszki J, Lingman G, Gudmundsson S, Molin J, et al. (2002) Uterine artery score and perinatal outcome. Ultrasound Obstet Gynecol 19: 438-442.
- Rai L, Lekshmi S (2010) Value of third trimester uterine artery Doppler in high-risk pregnancies for prediction of adverse perinatal outcome. JSAFOG 2: 31-35.
- Li H, Gudnason H, Olofsson P, Dubiel M, Gudmundsson S (2005) Increased uterine artery vascular impedance is related to adverse outcome of pregnancy but is present in only one third of late third trimester pre-eclamptic women. Ultrasound Obstet Gynecol 25: 459-463.
- Vergani P, Roncaglia N, Andreotti C, Alessandra A, Teruzzi M, et al. (2002) Prognostic value of uterine artery Doppler velocimetry in growth restricted fetuses delivered near term. Am J Obstet Gynecol 187: 932-936.
- Mello G, Parretti E, Fatini C, Riviello Ch, Gensini F, et al. (2005) Low-Molecular-Weight Heparin Lowers the Recurrence Rate of Preeclampsia and Restores the Physiological Vascular Changes in Angiotensin-Converting Enzyme DD Women. Hypertension 45: 86-91.
- Neykova K, Dimitrova V, Dimitrov R (2018) Uteroplacental blood flow in patients on antithrombotic medication because of previous obstetric history of placental mediated disorders. Akusherstvo I Ginecologia.
Citation: Neykova KK, Dimitrova V, Dimitrov R (2018) The Impact of Antithrombotic Medication on Uteroplacental Blood Flow in Patients with Previous Obstetric History of Placental Mediated Disorders. J Preg Child Health 5: 391. DOI: 10.4172/2376-127X.1000391
Copyright: © 2018 Neykova KK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2329
- [From(publication date): 0-2018 - Dec 18, 2024]
- Breakdown by view type
- HTML page views: 1728
- PDF downloads: 601