The Glasgow Coma Scale: A Breakthrough in the Assessment of the Level of Consciousness
Received: 21-Mar-2018 / Accepted Date: 05-Apr-2018 / Published Date: 14-Apr-2018 DOI: 10.4172/2573-4555.1000273
Abstract
The Glasgow Coma Scale (GCS) was introduced in 1974 as a measure of a patient’s level of consciousness. Before the development of this scale the level of consciousness was described by the terms like stuperose, comatose, semicomatose, obtunded, decerebrate etc. These terms were ill-defined, confusing and not comparable between different observers.
The GCS is a simple and reliable measure of level of consciousness. Once the medical and nursing staff is trained, the inter-observer variability is low. This scale went on to be accepted and used by most of the neurosurgical unit worldwide. The institute of Neurological sciences Glasgow is a world leader, in brain injury research and clinical care. In 1974, Professor Jennet and Mr. Teasdale of this institute published a paper in the lancet on the assessment of Coma and impaired consciousness. This paper proposed a structured method of assessment called “the Glasgow Coma Scale”. GCS is a component of the acute physiology and chronic health evaluation (APACHE) II score, the (revised) trauma score, the trauma and injury severity score (TRISS) and Circulation, Respiration, Abdomen, Motor, Speech (CRAMS) Scale, demonstrating the world wide adaptation of the scale.
Keywords: Glasgow coma scale; Level of consciousness; APACHE score; TRISS; CRAMS
Introduction
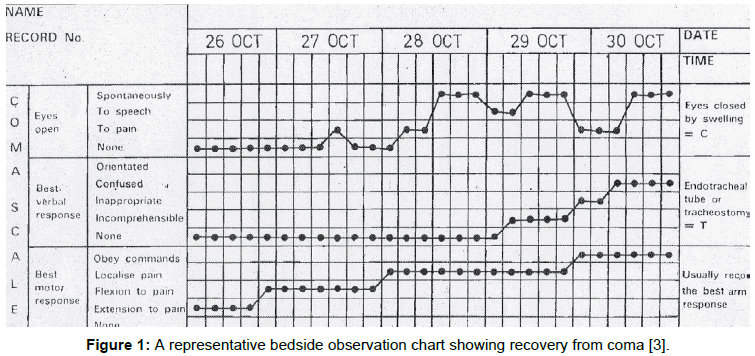
The essence of the GCS is the independent assessment of responses in three behavioural domains i.e. eye opening (E), Motor response (M), and verbal activity (V). These can be displayed as a bedside chart just like charting of temperature, pulse and blood pressure. This leads to early recognition of any deviation from previous reading and help to take appropriate action in time. The scores are given as statistical predictors of outcome. The original overall score was 14, after one year ‘abnormal flexion’ was added in motor response and the total GCS score become 15 [1-3].
The Scale
In a person who is fully conscious, alert and oriented, the Glasgow coma scale will be E4 M6 V5 (15/15) and the reduction in the score is indicative of deterioration in the state of consciousness (Table 1). The minimum score is E1 M1 V1 (3/15) who has no eye opening (E1), no motor response (M1) and no verbal response (V1) to any kind of stimuli. While recording the GCS, it is the best response at that particular moment, which is recorded. The best response is the motor response. The severity of the head injury can be assessed and prognosis can be predicted. GCS score of 13-15 is considered a mild head injury and this makes up almost 80% of cases. Score of 9-12 is moderately severe head injury and the incidence is 10%, score of 3-8 is severe head injury and is 10% of cases, the prognosis is worst in such patients (Figure 1).
| Eye opening | |||
|---|---|---|---|
| S.N. | Score | Parameter | Response |
| 1 | 4 | spontaneous | Indicates arousal, not necessarily awareness |
| 2 | 3 | To Speech | When spoken to- not necessarily command to open eye |
| 3 | 2 | To Pain | Applied to limbs and not face where grimacing can causes closure of eye |
| 4 | 1 | None | |
| Motor response | |||
| 5 | 6 | Obeys command | Exclude grip reflex or postural adjustments |
| 6 | 5 | Localizes | Other limb moves to site of nail bed pressure |
| 7 | 4 | Withdraws | Normal flexion of Elbow or knee to local painful stimulus |
| 8 | 3 | Abnormal flexion | Slow withdrawal with pronation of wrist, adduction of shoulder |
| 9 | 2 | Extensor response | Extension of elbow with pronation and adduction. |
| 10 | 1 | No Movement | |
| Verbal response | |||
| 11 | 5 | Oriented | Knows who, where, when; Year, season, month |
| 12 | 4 | Confused conversation | Attends and responds but answers muddled /wrong |
| 13 | 3 | Inappropriate words | Intelligible words but mostly expletive or random |
| 14 | 2 | Incomprehensible speech | Moans and groans only - no words |
| 15 | 1 | None | |
Table 1: Glasgow come scale with scores [3].
Figure 1: A representative bedside observation chart showing recovery from coma [3].
Strength
1. It helps the medics and paramedics to independently assess the response in three behavioural domains i.e. eye opening (E), Motor response (M), and verbal activity (V).
2. They can readily be displayed as a bedside chart. Charting is easy just as the routine charting of Pulse, Temperature and blood pressure by nursing staff [4,5].
3. It also facilitates communication between doctors who can report a patient’s state, as E2, M4, and V3 for example.
4. Useful tool for initial triage and a guide for shifting to general or specialist care.
5. It acts as a basis for monitoring progress after acute insult and helps in predicting the likely outcome.
6. The database can be used to devise the guidelines and standard operating procedure (SOP) for management of traumatic brain injury. It can be used to classify head injured patients in epidemiological studies worldwide [6].
The Weakness
1. The Glasgow study does not considers the other predictive factors like patient’s age, history of lucid interval, papillary reactions, eye movements, pulse rate, Blood pressure, respiration and initial CT findings etc. [7].
2. It is not applicable in children.
3. It records the best motor response (M6), yet the patient could be monoplegic, hemiplegic or tetraplegic.
4. The response may be impaired due to language problem, alcohol intoxication, shock, hypoxia, Intubation and tracheostomy. Moreover the verbal response cannot be elicited in intubated or tracheostomised patients.
5. There is no check on cranial nerve functions.
6. Eye opening and closing may be impaired by black eye and conjunctival chemosis.
Conclusion
The Glasgow Coma Scale remains the most commonly used method of assessing the level of consciousness in patients of traumatic brain injury. Once learned it becomes a handy and reliable tool to asses, communicate and predict the likely outcome. Out of the three components the motor (M) response is most important. It is also important to stress that for clinical use, patients should be communicated by the three separate scores (E, V, M) and never by total sum. If eye or verbal response cannot be evaluated, this should be indicated by recording as “c” (Eye closed) or “T” (Intubated) respectively. The GC score is useful for research, audit, prognostic calculations and other type of data collection that requires digitising and grouping of clinical information.
References
- Teasdale GM, Jennett B (1974) Assessment of coma and impaired Consciousness: a practical scale. Lancet 2: 81-84.
- Jennett B, Teasdale G (1982) Management of Head Injuries. Published by F. A. Davis Company, Philadelphia 42: 361
- Jennett B (2005) Development of Glasgow coma and outcome scales. Nepal Journal of Neuroscience 2: 24-28.
- Teasdale G (1975) Acute impairment of brain function-1. Assessing conscious level. Nursing times 71: 914-917
- Teasdale G, Galbraith S, Clarke K (1975) Acute impairment of brain function- 2: observation record chart. Nursing Times 71: 972-973.
- Jennett B (1996) Epidemiology of head injury. J Neurol Neurosurg Psychiat 60: 362-369.
- SK Kochar (2013) Principle and practice of Trauma care. Jaypee Brothers Medical Publishers (P) ltd: New Delhi 2nd edition 162-189.
Citation: Agrawal SN (2018) The Glasgow Coma Scale: A Breakthrough in the Assessment of the Level of Consciousness. J Tradit Med Clin Natur 7: 273. DOI: 10.4172/2573-4555.1000273
Copyright: © 2018 Agrawal SN. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 28442
- [From(publication date): 0-2018 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 27568
- PDF downloads: 874