Short Communication Open Access
The Future of Nursing: Assumption of New Roles and Responsibilities
Carlos Alberto Díaz1* and Rodrigo Alberto Castilla21Sanatorio Sagrado Corazón, Public Health, Health Economics and Management Specialisation,Universidad ISALUD, Buenos Aires, Argentina
2Health Economics and Management, Sanatorio Sagrado Corazón, Buenos Aires, Argentina
- *Corresponding Author:
- Carlos Alberto Díaz
Physician, Medical Manager at Sanatorio Sagrado Corazón
Public Health Specialist, Director of the Health Economics and Management Specialisation
Universidad ISALUD, Buenos Aires, Argentina
Tel: +549115750763
E-mail: carlos.diaz@sagrado-corazon.com.ar
Received date: January 25, 2017; Accepted date: February 10, 2017; Published date: February 17, 2017
Citation: Díaz CA, Castilla RA (2017) The Future of Nursing: Assumption of New Roles and Responsibilities. J Comm Pub Health Nurs 3: 158. doi:10.4172/2471-9846.1000158
Copyright: © 2017 Díaz CA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
At present, we are facing a conflictive incoherence between the importance of nursing as a profession, and the social-institutional-political-organisational-economic recognition the nurses actually receive, in spite of the academic improvement. This dilemma seems to be caused by the absence of health as a whole in the political agenda, the health’s system fragmentation, low salaries, lack of collective bargaining, and other sociocultural factors. The future of nursing will be based in management. Professional spaces will need to be amplified; new skills and competencies will need to be developed. Leadership, communication, efficiency, should be key factors. Finally, there will not be any future without professional growth and long-term careers, and an improvement of work conditions and economic remuneration.
Introduction
In our region, we are at present facing a dilemma over the conflictive incoherence between the importance of nursing as a profession, and the social-institutional-political-organisationaleconomic recognition the nurses actually receive. Nursing’s essence, its identity, does not match its social image, which still remains full of stigmas [1]. This inconsistency is mainly based in the fact that health’s politicians, managers, unions, and even nurses, have not cared enough about improving or dismissing this social contradiction. Collière [2], more than twenty years ago, already depicted the relevance of the nurse’s role: “the nurses ensured life’s continuity, helping us through their care, to face life and death, in an underestimated sociocultural background”.
A gap has been created between the relevant role the nurses’ play, through their professional care, in the patients’ clinical results, and the years of education required to train and acquire these skills. Therefore, there is a gap between the professional development and the economic recognition, which is usually lean.
Although professional education, training and academic improvement has been enriched in the last decades, these upgrades were not able to change the society’s unfavourable opinion about nursing. Since 1969, the continuous growth of nursing as a profession has set an example, mainly due to the establishment of a bachelor’s degree, and the institutional mandatory matriculation, which guarantees the quality of the nurse´s skills and abilities. However, the lack of professional nurses in the region and the local traditions have caused these new rules and achievements to become flexible, allowing auxiliary workers to replace the nurses’ roles.
Nursing is of the utmost importance for health management [3]. Their functions include the detection of clinical deterioration, transitional care and continuity assistance of high complexity patients [4]. They replace the autonomy lost by the patients, not only in hospital units but also in home-care. During hospital stay, they prevent infections, skin ulcerations, medication errors and falls.
The nurses’ integration to the multidisciplinary health teams has enhanced institutional management by providing a humanistic vision, with a close proximity to the patient. Their knowledge has evolved substantially, and presently includes clinical communication, care technology and information management [5]. Nursing as an economic good is a rare but valuable asset, in contrast to other modern, positivists, professions, in which sacrifice and abnegation are virtues of only a few individuals [6]. In spite of the central position that nursing has in every health system, which includes care, control, treatment, assistance continuity and transition between levels of care [7], society has not rewarded them with appropriate remuneration or work stability. In Latin America, this lack of recognition is emphasized. Society seems to be unaware of the nurses’ true identity.
In Argentina, the number of health professionals exceeds the minimum proposed by WHO in the Toronto call: 25 per 10.000 inhabitants [8]. However, there are more physicians than nurses, resulting in a nurse/physicians rate below one. The country is actually in need of 80,000-90,000 professional nurses, and a greater number of matriculated nurses. Therefore, in order to solve this situation and match the international standards of an integrated health system, approximately 15,000 nurses should be graduating each year, for the next 8 years [9-12].
The nursing profession is usually biased by certain identifiable conflicts [13]: low salaries, moonlighting, burn-out, and inadequate work structure or equipment [14]. These are often aggravated by sleep deprivation [15], fatigue [16,17], exposure to biological, chemical and physical hazards, and musculoskeletal diseases caused by physical effort [18]. In addition, nursing profession is in disadvantage, due not only to the global lack of nurses [19], but also because of their overassignment to tasks that could be performed by less educated people, their reduced esteem in health’s multidisciplinary teams, and the irrational productivity increase which health institutions’ managers constantly demand. The consequence of these factors is an unattractive career for students, whose concerns about work conditions have been on the rise for many years.
The urgent need to reduce assistance costs makes it impossible for health managers to overlook several contingency strategies. One of these is the increase of the number of patients assisted by one nurse. However, it can lead to worse results in patient morbimortality, which would be a diminished marginal return. The austerity measures being applied in the health systems’ redesign are impoverishing the clinical results [20]. The RN4CAST project studied the difference in nurse per patient rates and nurse education in nine countries. Data was obtained from the clinical history of 422,730 patients over 50 years, which were surgically intervened. The study results showed that the risk of mortality in the first 30 days after hospital discharge had been higher in the group of patients in which a nurse was assigned to care for 8 patients, compared with the group in which a nurse was assigned to care for 6 patients. Besides, the risk of mortality had been reduced 10% in groups which were assisted by a graduated nurse, and an extra 10% if the institution on which the patients were staying had over a third of their nurses graduated. These results prove that the nurses’ education and the number of unqualified personnel have statistical significance in the patients’ clinical results [21-23].
The Argentinean health system’s fragmentation, which has insufficient work offer, forces professionals to search for the better paid and less exigent alternatives. This quest generates an unfair competence between co-workers, which tend to lose the sense of compromise of an individual with an institution. Proofs of this lack of bonding are the high absence rates seen across the country, from 8% to 22%, which amplifies the workload and creates a greater human resources deficit.
The mentioned data should lead to a thorough analysis of which ought to be the conditions offered to the nurses in order to create a healthy work ambient. The resulting strategy should be especially focused in avoiding the need to moonlight. A discussion is nowadays being held over a proposal for the reduction of the nurses’ daily workload from 8 to 6 hours. Although this motion could benefit professionals who, being used to have at least two jobs, would spend 12 hours working instead of 14, it would be a better alternative to consider a well remunerated 8 hour workload. The road we are now treading is one towards complete failure for everyone involved: nurses, employers, financiers, and even the country, because of an increased deficit caused by production direct costs’ or adverse events [24].
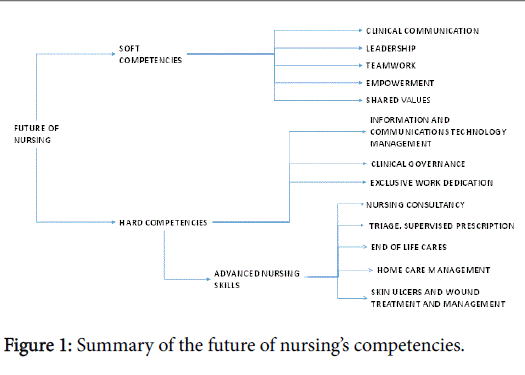
The new roles and responsibilities nursing must assume to properly adapt to the modern and future society will now be listed [25]:
1. Service’s process management: definition and standardisation of patient care. Sequence description. Identification of wasted time and unnecessary activities [26].
2. The 5 key fields’ management: a) administrative and accountancy office; b) human resources; c) leadership; d) efficient use of resources; e) trustworthy corporate image. Nurses will have to supervise the exchange of intermediate products, in order to guarantee an appropriate hospital stay, care transition and continuous assistance, therefore assuring economic efficiency [27,28].
3. Creation of a new professional space: Nurses will have to be in a continuing education cycle, redefining and revising their skills in order to adapt to the never ending changes our dynamic society imposes. This ability will lead to empowerment and a more relevant role in decision-making in health institutions [29,30].
4. Care management of acute and chronic conditions in all complexity levels [31,32]: even home care, with focus on chronic conditions, in which an improvement of production is mandatory.
5. Pre-discharge education and enforcement of the patients’ family role as caregivers: Major involvement in care transition programs and discharged patients’ follow-up.
6. New education strategies and chronic disease screening: Proactive participation in primary and secondary prevention and health promotion.
7. Continuing education in nursing skills, patient safety, skin care, check-lists, bundles, hand hygiene programmes, information and communications technologies, etc [33,34].
8. Work conditions’ improvement [35]: removal of tasks not meant to be performed by nurses. Strategic scheduling in order to enlarge the time spent with patients and to add extra academic activities. Moonlighting prevention. Reduction of absence rates, violent incidents, work-related risks, institutional bullying.
9. Major multidisciplinary and research teams’ integration [36]: Approach and diffusion of the latest scientific evidence. Nursing team image boosting
10. Assistance standardised processes design: Impulse of institutional quality measures and patient safety culture.
11. Advanced nursing skills development and practise: ambulatory and primary level nursing consultancy, triage, supervised prescription, chronic patients’ follow-up, sanitary education, end of life cares, pressure ulcer and wound care treatment and management, pharmacological interactions’ evaluation [37-39].
12. Health policies and tendencies comprehension: epidemiological and demographic transitions, global burden of disease, etc (Figure 1).
Conclusion
Nowadays we are facing a conflictive incoherence between the importance of nursing as a profession, and the social-institutionalpolitical- organisational-economic recognition the nurses actually receive, in spite of the academic improvement. This dilemma seems to be caused by the absence of health as a whole in the political agenda, the health’s system fragmentation, low salaries, lack of collective bargaining, and other sociocultural factors. However, the most worrying issue seems to be the perception that nursing leaders and health managers have not been working hard enough to find a solution.
The future of nursing will be based in management [40]. Professional spaces will need to be amplified; new skills and competencies will need to be developed. Leadership, communication, efficiency, should be key factors. Finally, there will not be any future without professional growth and long-term careers, and an improvement of work conditions and economic remuneration [41].
References
- Calvo Calvo MA (2011) Imagen social de las enfermeras y estrategias de comunicación pública para conseguir imagen positiva. Index Enferm 20: 3.
- Collière MF (1993) Promover la vida, de la práctica de las mujeres cuidadores a los cuidados de enfermerÃa. Madrid: Ed. Interamericana McGraw-Hill.
- Thompson AC (2016) Comprehensive Health Care: Dilemmas and Challenges in Nursing/La salud integral: Dilemas y desafÃos en la enfermerÃa. Hisp Health Care Int 14: 156-157.
- Molina Castillo MC (2016) Mapa de conflictos éticos en enfermeras asistenciales. Tesis de Grado. Universidad Jaen. Mayo.
- Conejero Ferrer P (2016) El rol de la enfermerÃa coordinadora de asistencia ventricular en España: el futuro ya ha llegado. Cir Cardiov. 23: 62-67.
- Waldow VR (2013) Cuidar de si, cuidar del otro, cuidar del todo: Implicaciones para la salud y enfermerÃa. 2: 53-56.
- Fernandez R, Johnson M, Tran DT, Miranda C (2012) Models of care in nursing: a systematic review. Int J Evid Based Healthc 10: 324-337.
- OPS (2006-2015) LLamado a la acción de Toronto 2005.
- World Health Organization. Health Workforce Atlas: Density of nursing and midwifery personnel (total number per 1000 population).
- Cejas DMC (2010) Recursos humanos en salud: Argentina desde una perspectiva comparada.
- Association of American Medical Colleges. The complexities of Physician Supply and Demand: Projection from 2013 to 2025.
- Duré MI Cadile MC (2015) La gestión de recursos humanos en salud en Argentina. Una estrategia de consensos 2008-2015.
- Crojethovic M (2011) Microcosmos Hospitalario. Redefiniendo las reglas en los hospitales del Gran Buenos Aires.
- Merelles Tormo A (2016) Precarización laboral en el sector sanitario: el caso de la enfermerÃa en la comunidad autónoma de valencia. Tesis doctoral.
- Rogers AE. The Effects of Fatigue and Sleepiness on Nurse Performance and Patient Safety.
- Canadian Nurse Association (2010) Nurse Fatigue and Patient safety. ResearchReport.
- Wolf LA, Perhats C, Delao A, Martinovich Z (2017) The effect of reported sleep, perceived fatigue, and sleepiness on cognitive performance in a sample of emergency nurses. J Nurs Adm 47: 41-49.
- Pereira F, Mucha A (2016) la configuración de las condiciones laborales de la enfermerÃa en el área metropolitana de Buenos Aires: un análisis en el cruce del orden de género y la organización del sistema de salud. Salud Colectiva. 12: 221-238.
- Aspiazu E (2016) Nursing working conditions in Argentina: between professional and precarious health care. Trabajo y Sociedad.
- Aiken LH, Sermeus W. Van den Heede K. Sloane DM, et al. (2012) Patient safety, satisfaction and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 344: 1-14.
- Aiken LH, Sloane DM, Bruynell L, Heed KVD, Griffiths P, et al. (2014) Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet 383: 1824-1830.
- Aiken LH, Cimiotti JP, Sloane DM, Smith HL, et al. (2011) The effects of nursing staffing and nurse education on patient deaths in hospital with different nurse work environments. Med Care 49: 1047-1053.
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH (2002) Hospital nurse staffing and patient mortality, nurse burnout and job dissatisfaction. JAMA 288: 1987-1993.
- Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Sermeus W, et al. (2013) Nurse reports of working conditions and hospital quality of care in 12 countries in Europe. International Journal of Nursing Studies 20: 143-153.
- Fernandez R, Johnson M, Tran DT, Miranda C (2012) Models of care in nursing: A systematic review. Int J Evid Based Healthc 10: 324-337.
- DÃaz CA, Braem V, Quiros MC (2012) Innovación gestión hospitalaria. Ediciones ISALUD. Buenos Aires.
- DÃaz CA (2012) Gestión de servicios asistenciales. Ediciones Isalud. BsAs.
- MarrinerTomey A (2009) GuÃa de Gestión y dirección de enfermerÃa: Incluye Evolve.
- International Council of Nurses (2016) ìĀmbitos de la práctica de enfermerÃa y Marcos para la toma de decisiones. GuÃa Práctica. ICN.
- Rivero MartÃnez M (2016) Evaluación de competencias del enfermero especialista de cuidados médico-quirúrgicos, utilizando la escala ECOenf. Tesis doctoral. Universidad Complutense de Madrid.
- Fairbrother G, Chiarella M, Braithwaite J (2015) Models of care choices in today's nursing workplace: Where does team nursing sit? Aust Health Rev 39: 489-493.
- Estefo Agüero S, ParavicKlijn T (2010) EnfermerÃa en el rol de gestora de cuidados. Ciencia y enfermerÃa. XVI: 33-39.
- Cometto MC, Gómez PF, MarconDalSasso GT, Zárate Grajales RA, De BortoliCassiani SH, et al. (2011) Organización panamericana de la salud. EnfermerÃa y Seguridad de los Pacientes.
- Agencia de Calidad del Sistema Nacional de Salud (2009) Dirección del proyecto SENECA. GarcÃa EI. Rodriguez Escobar J (eds.) (2008) Estándares de calidad de cuidados para la seguridad del paciente en los hospitales del SNS. proyecto SENECA: Informe técnico Madrid: Ministerio de Sanidad y polÃtica Social.
- Hernández Cantoral A, Zárate Grajales RA (2011) Hospital Magnet: Ideal scenario to guarantee Quality of care and job satisfaction of nurses. Revista EnfermerÃa Universitaria ENEO â¬?¬? UNAM 8: 25-32.
- Sánchez VD, Noguera MA, Cecilia EC, Sánchez FS, Artacho MDC (2007) El paradigma de la enfermerÃa basada en la evidencia (EBN) en la enfermerÃa clÃnica hospitalaria. Nurse Investigación.
- Negre ML, Montesdeoca CA, RodrÃguez CD, Borja AG, López SM (2011) Nursing consultation, high-resolution in primary care. Rev Enferm 34: 32-39.
- Becker JB, Lopes MCBT, Pinto MF, Campanharo CRV, Barbosa DA, et al. (2015) Triage at the Emergency Department: Association between Triage levels and patient outcome. Rev da EscEnferm da USP 49: 783â¬?¬?789.
- Aiken L, Rafferty AM, Sermeus W (2014) Caring nurses hit by a quality storm. Nurs Stand 28: 22-25.
- Fairbrother G, Chiarella M.Braithwaite J (2015) Models of care choices in today´s nursing workplace: Where does team nursing sit? Aust Health Rev 39: 489-493.
- Fairbrother G, Jones A, Rivas K (2010) Changing model of nursing care from individual patient allocation to team nursing in the acute inpatient environment. Contemp Nurse 35: 202-220.
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 6740
- [From(publication date):
February-2017 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 5799
- PDF downloads : 941