The Frequency of Subtalar Joint Instability in Adult Patients Who Underwent Surgical Correction of First Metatarsophalangeal Joint Surgery-A Retrospective Radiographic Evaluation
Received: 18-Sep-2018 / Accepted Date: 02-Nov-2018 / Published Date: 09-Nov-2018
Abstract
Objective: Subtalar joint instability creates misalignment of talus on the calcaneus. The loss of talar alignment and stability leads to a prolonged period of foot pronation during the stance phase of the gait cycle. Over or hyperpronation is known as a contributing factor to the progression of hallux valgus (HV) and hallux limitus/rigidus (HL/R). The purpose of this retrospective radiographic study is to evaluate the number of adult patients (feet) diagnosed with HV and HL/R who underwent surgical correction within a one year period.
Methods: Pre-operative weightbearing radiographs for one-hundred five feet, that met the inclusion criteria, were retrospectively analyzed. Both transverse (talar second metatarsal (T2M)) and sagittal (talar declination (TD)) plane angular measurements were independently calculated and compared to normal values based on literature.
Results: In this study, 97 (92.38%) of 105 feet with HV and HL/R had values above normal for at least one of the T2M and/or TD angle indicating an abnormal talar alignment. The mean T2M was 21.88 ± 7.95 (range 1.13 to 50.58 degrees) and the mean TD was 23.45 ± 3.94 (range 14.75 to 34.24 degrees). Forty (38.1%) feet exhibited a single plane deformity and 57 (54.28%) comprised of a both transverse and sagittal plane deformities.
Conclusion: This supports the hypothesis that a correlation between subtalar joint instability and HV or HL/R exists. This hind foot deformity should be considered as a contributing factor in the progression of 1st MPJ pathology.
Keywords: Hallux valgus; Hallux limitus; Hallux rigidus; Subtalar joint instability; Hyperpronation; Radiographic measurements
Introduction
Hallux valgus (HV) and hallux limitus/rigidus (HL/R) are some of the most commonly reported chronic foot disorders. [1,2]. Prescribed treatment options vary based on the severity of symptoms and the degree of structural pathology [3]. Most options focus on correcting the local pathomechanic issue at the 1st metatarsophalangeal joint (1st MPJ) and alleviating the associated pain. The prevalence of 1st MPJ disorders has been increasing and is expected to increase in the future with the aging society.
Pronation of the subtalar joint creates an “unlocking” of the joints of the hind and mid foot, whereas supination creates a “locking” or stiffness of those same joints. A loss of stability of the talus on the calcaneus and/or navicular (tarsal mechanism) can lead to a prolonged period of pronation during the stance phase of the gait cycle [4,5]. A primary factor for the progression of both HV and HL/R is over-pronation [6-9]. The excessive subtalar joint pronation can also lead to increased forces on the 1st MPJ and/or the 1st metatarsocuneiform joint (1st MCJ) [10-16].
The purpose of this retrospective study is to evaluate the possible association between pathologic subtalar joint alignment and HV and HL/R. The presence of higher than accepted normal (≥ 17 degrees) weightbearing talar-second metatarsal (T2M) and/or talar declination (TD) angles (≥ 22 degrees) in patients diagnosed with HV and HL/R can be considered an indication of abnormal hindfoot alignment [17].
Patients and Methods
After receiving institution review board approval, the weight bearing relaxed stance position (RSP) dorsoplantar (DP) and lateral radiographs of a total of 105 feet from adults, 18 years of age and older, were specifically diagnosed with 1st MPJ pathology, HV and HL/R. A diagnosis of HV and hallux limitus-rigidus (HL/R) was made via clinical and radiographic examination. Specifically, the diagnosis of HV was based on DP X-ray measurements of the 1st intermetatarsal angle, >9 degrees, and hallux abductus angle >25 degrees [18-20]. Only the feet of patients who underwent surgical correction and met the inclusion criteria, were analyzed. The consecutive patient selection was based on ICD 9 (International Classification of Diseases, World Health Organization, Geneva, Switzerland) (735.0, 735.2) and CPT® (Current Procedural Terminology, American Medical Association, Chicago, IL) (28290, 28293, 28296) codes at the Louis Stokes Cleveland VA Medical Center (Cleveland, OH) from 01/2011 to 12/2011.
The radiographs were then collected and independently evaluated (HMK). Only the patients (feet) who had no history of an acute trauma to their 1st MPJ or previous foot surgery were included. Patients were excluded if they had trauma to their 1st MPJ or previous foot surgery. A total of one-hundred-and-five feet met the inclusion criteria.
Determination of radiographic angles
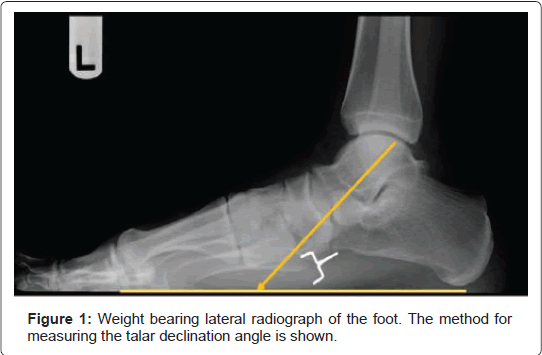
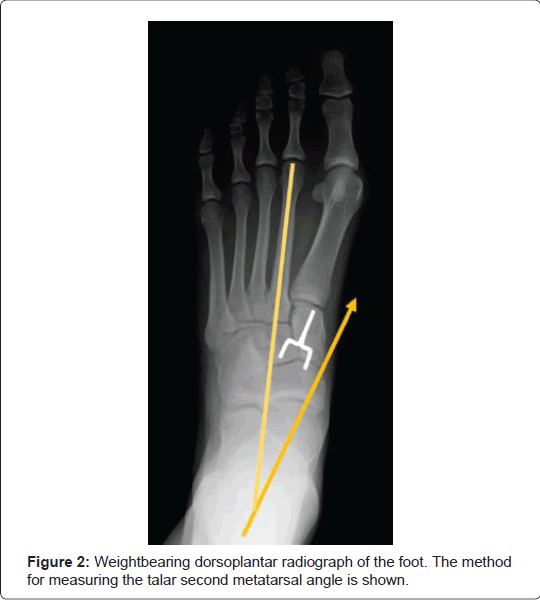
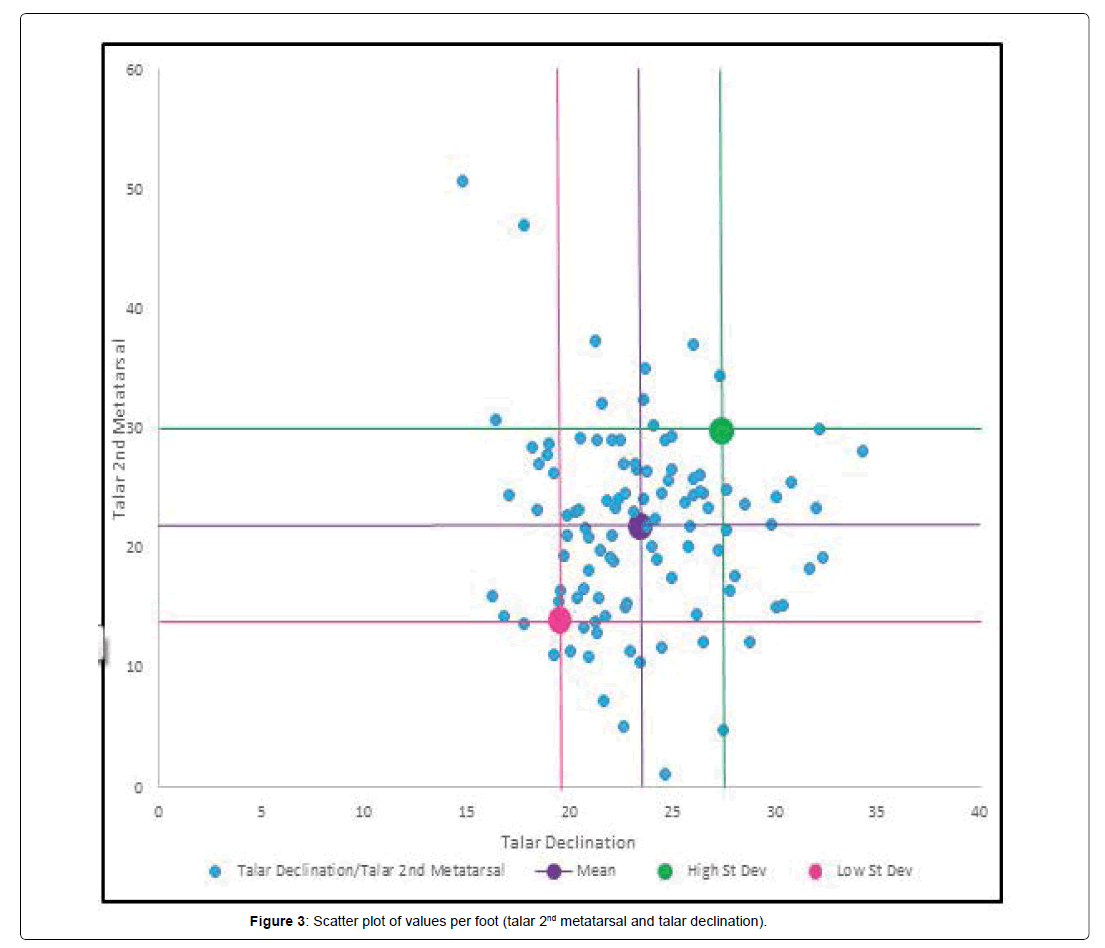
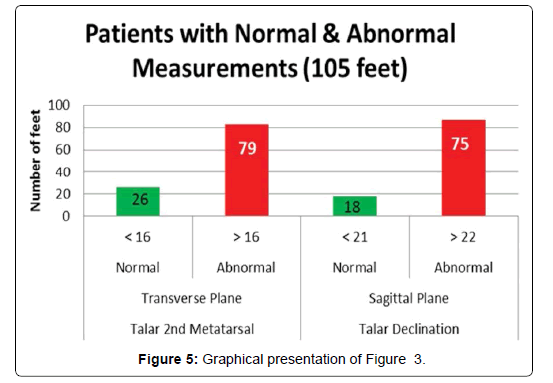
The talar declination (TD) and talar-second metatarsal (T2M) angles were used to determine subtalar joint alignment (Figures 1 and 2). These angles were selected because they provide an accurate representation of sagittal and transverse plane alignment of the subtalar joint. The T2M angle was measured foth angles were independently measured using software thatrom the DP preoperative radiographs (transverse plane) and the TD angle was measured from the lateral preoperative radiographs (sagittal plane). B is part of the VistA Computerized Patient Record System, version 1.0.28.24. by a single individual (HMK) (Tables 1 and Figure 3-5).
| Foot # | Talo-2nd Met | Talar declination | Foot # | Talo-2nd Met | Talar declination | Foot # | Talo-2nd Met | Talar declination |
|---|---|---|---|---|---|---|---|---|
| 1 | 28 | 18 | 36 | 23 | 20 | 71 | 14 | 21.74 |
| 2 | 18 | 24 | 37 | 14 | 18 | 72 | 51 | 14.75 |
| 3 | 19 | 24 | 38 | 15 | 23 | 73 | 47 | 17.74 |
| 4 | 22 | 24 | 39 | 12 | 27 | 74 | 20 | 27.24 |
| 5 | 26 | 24 | 40 | 35 | 24 | 75 | 18 | 28.01 |
| 6 | 26 | 26 | 41 | 37 | 21 | 76 | 24 | 17.03 |
| 7 | 16 | 20 | 42 | 14 | 17 | 77 | 29 | 24.67 |
| 8 | 24 | 24 | 43 | 16 | 21 | 78 | 32 | 21.58 |
| 9 | 19 | 22 | 44 | 27 | 18 | 79 | 19 | 19.75 |
| 10 | 29 | 19 | 45 | 31 | 16 | 80 | 18 | 20.9 |
| 11 | 23 | 20 | 46 | 24 | 22 | 81 | 22 | 24.15 |
| 12 | 11 | 19 | 47 | 27 | 23 | 82 | 22 | 25.85 |
| 13 | 11 | 20 | 48 | 18 | 32 | 83 | 32 | 23.59 |
| 14 | 17 | 21 | 49 | 18 | 25 | 84 | 25 | 26.51 |
| 15 | 7 | 22 | 50 | 27 | 23 | 85 | 29 | 24.91 |
| 16 | 37 | 26 | 51 | 24 | 30 | 86 | 30 | 24.1 |
| 17 | 27 | 23 | 52 | 30 | 32 | 87 | 24 | 22.34 |
| 18 | 25 | 24 | 53 | 34 | 27 | 88 | 26 | 19.25 |
| 19 | 15 | 30 | 54 | 24 | 26 | 89 | 16 | 16.18 |
| 20 | 15 | 30 | 55 | 27 | 25 | 90 | 14 | 21.25 |
| 21 | 22 | 21 | 56 | 23 | 22 | 91 | 13 | 21.28 |
| 22 | 22 | 26 | 57 | 1 | 25 | 92 | 5 | 22.6 |
| 23 | 25 | 31 | 58 | 5 | 27 | 93 | 28 | 18.85 |
| 24 | 29 | 21 | 59 | 22 | 30 | 94 | 29 | 20.49 |
| 25 | 29 | 22 | 60 | 25 | 23 | 95 | 29 | 22.07 |
| 26 | 23 | 18 | 61 | 12 | 24 | 96 | 23 | 32 |
| 27 | 15 | 26 | 62 | 11 | 21 | 97 | 28 | 34.24 |
| 28 | 19 | 22 | 63 | 22 | 28 | 98 | 20 | 24 |
| 29 | 19 | 32 | 64 | 26 | 24 | 99 | 24 | 25.57 |
| 30 | 25 | 26 | 65 | 23 | 23 | 100 | 24 | 28.54 |
| 31 | 10 | 23 | 66 | 11 | 23 | 101 | 12 | 28.72 |
| 32 | 23 | 27 | 67 | 21 | 20.88 | 102 | 16 | 27.81 |
| 33 | 26 | 26 | 68 | 25 | 27.65 | 103 | 13 | 20.69 |
| 34 | 16 | 19 | 69 | 15 | 22.76 | 104 | 20 | 21.45 |
| 35 | 16 | 20 | 70 | 21 | 19.93 | 105 | 21 | 22.03 |
| Mean | 22 | 23 | ||||||
| Standard deviation | 8 | 4 |
Table 1: Radiographic measurements.
| Comparison of Normal to Abnormal Measurements | n | |
|---|---|---|
| Normal T2M and TD Angles | 13 | 12% |
| Abnormal T2M and/or TD Angle | 92 | 88% |
Table 2: Number and percentage of feet exhibited normal or abnormal radiographic measurements.
Data analysis
The angles calculated from the radiographs for patients in both groups were compared to the normal values based on literature [21- 25]. A T2M angle ≤ 16º and the TD angle ≤ 21º would be considered “normal”. Thus, T2M angles greater than ≥ 17º and/or TD angles higher than ≥ 21º may indicate the presence of subtalar joint instability. While a clinical determination of a pathologic angle that is 1 degree difference between normal and abnormal will not alter the treatment, however a “line in the sand” must be made for determining normal and abnormal. For the patient population, the percentage of occurrence of values higher than the normal values in at least one view (DP or lateral) was calculated.
Once a total percentage was calculated, the presence of the deformity was further analyzed with respect to the plane of dominance, if any. Pathologic values of the T2M angle indicates deformity in the transverse plane while pathologic values of the TD angle indicates deformity in the sagittal plane [21-25]. Transverse plane dominance was identified when the radiographs for a single patient showed a higher than normal T2M angle and a TD angle within the normal range. Alternatively, sagittal plane dominance was identified with only a higher TD angle coupled with a normal T2M angle. Pathologic T2M and TD angles together indicate deformity in both planes.
Statistical analysis
The data was tested for normality using the Kolmogorov-Smirnov test to determine distribution of the sample population. For normally distributed data, a t-test was used to determine the statistically significant difference between angle values higher than normal and values less than or equal to normal within a group of patients. The Mann-Whitney Rank Sum test was used for data that was not normally distributed. Statistical analysis was conducted using SigmaStat Software, version 3.5 (Systat, Chicago, Illinois) (JS). Statistical significance was defined at the 5% (p ≤ 0.05) level.
Results
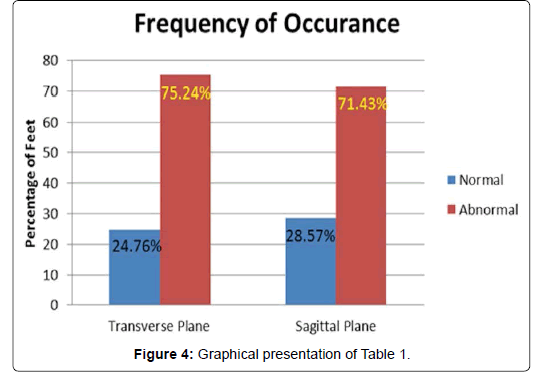
Frequency of occurrence
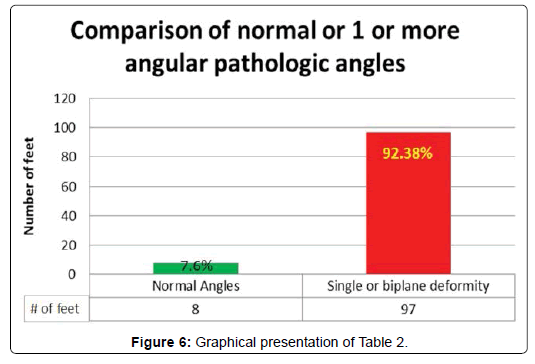
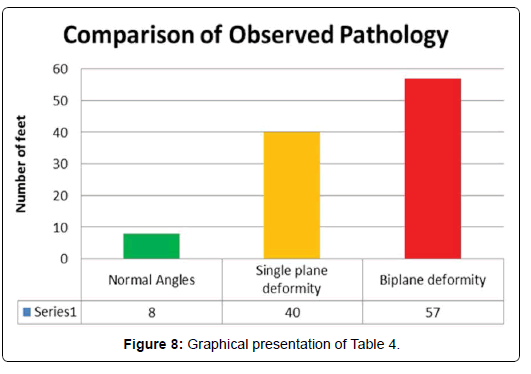
Ninety-two (88%) of the 105 feet diagnosed with HV or HL/R had one or more pathologic angle and only 13 (12%) feet had normal T2M and TD angles (Table 2 and Figure 6). The mean T2M was 22 ± 8 (range 5 to 51 degrees) and the mean TD was 23 ± 4 (range 15 to 34 degrees). The radiographic angles were separated into two sub-groups; pathologic and acceptable normal values. The T2M angle was higher than the normal values in 76 (73%) feet and the TD angle was abnormal in 69 (64%) feet. The number of feet with pathologic and normal values was compared to obtain the frequency of occurrence of these values for feet diagnosed with a HV and HL/R (Table 3 and Figure 7). Forty (38%) of the feet had a single plane involvement and 52 (50%) feet exhibited both transverse and sagittal plane deformities (Table 4 and Figure 8).
| Frequency of Occurrence | n | |
| Transverse Plane | ||
| Normal (≤ 16°) | 29 | 27% |
| Abnormal (≥ 17°) | 76 | 73% |
| Sagittal Plane | ||
| Normal (≤ 21°) | 36 | 36% |
| Abnormal (≥ 21°) | 69 | 64% |
Table 3: The frequency of transverse and sagital plane abnormal findings.
| Frequency of Normal Verse Plane(s) of Deformity | n | |
| Normal | 13 | 12% |
| Single plane deformity | 40 | 38% |
| Biplane deformity | 52 | 50% |
Table 4: Number and percentage of normal, or planar dominace of abnormal radiographic findings.
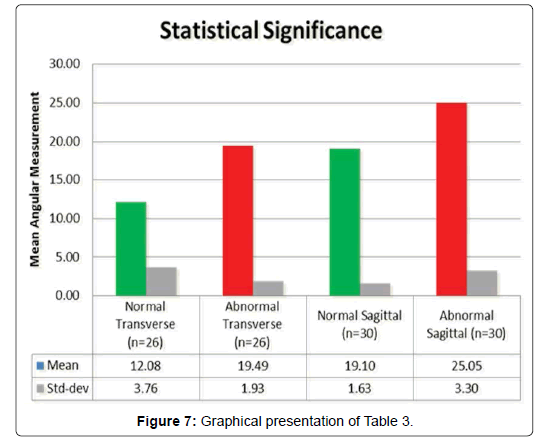
Statistical significance
An equal number of feet were considered to test statistical correlation between pathologic radiographic angles and acceptable values. The mean values for T2M and TD angles were calculated. It was seen that there was a statistically significant difference between the normal T2M values (≤ 16 degrees) and the abnormal T2M values (≥ 17 degrees) for both groups of feet. Moreover, the abnormal TD angle values were statistically different than the normal TD angles. This test helps to further validate the data results.
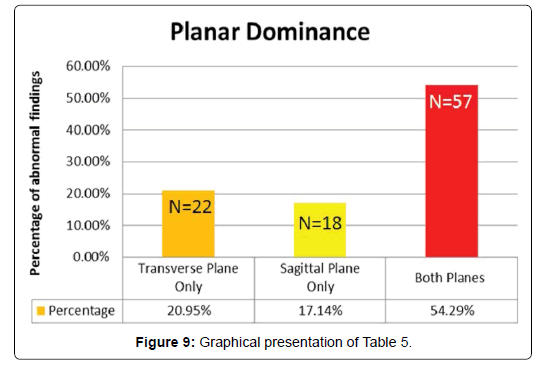
Planar dominance
Planar dominance was also analyzed for abnormal transverse and sagittal plane deformities (Table 5 and Figure 9). Of the 92 (88%) feet that exhibited abnormal radiographic angle, 40 (38%) exhibited a single plane deformity and 52 (50%) comprised of a both transverse and sagittal plane deformity. A trend was identified in feet diagnosed with a HV and HL/R. Twenty-five (24%) feet showed only a transverse plane displacement and a sagittal plane deformity was seen in 15 (14%) feet. Finally, 52 (50%) feet showed evidence of a subtalar joint misalignment in both the transverse and sagittal planes.
| Planar Dominance | n | |
| Transverse only | 25 | 24% |
| Sagittal only | 15 | 14% |
| Both Transverse and Sagittal | 52 | 50% |
>Table 5: Number and percentage of single or biplane plane(s) of deformity.
Discussion
The talotarsal joint (TTJ) is formed by the articular surfaces of the talus with both the calcaneus and navicular. This complex mechanism is responsible for the redistribution of the proximal vertical forces posteriorly and anteriorly [26-27]. A second function of the TTJ is the locking-stabilizing supinatory and unlocking-weakening pronatory motions. There are specific periods during the gait cycle when the TTJ should be pronated and other times supinated [28-30]. The stability of the TTJ will therefore determine the amount of supination or pronation, as well as the redistribution of the vertical forces posteriorly and anteriorly.
The sinus tarsi, a canal formed by the talus and calcaneus, acts as dividing landmark or fulcrum point for the posterior and anterior joint forces. It has been estimated that approximately 52% of the vertical forces, in a stable-aligned TTJ, should pass through the body of the talus onto the posterior talocalcaneal joint, at heel strike and the remaining 48% of the forces should pass anteriorly [31].
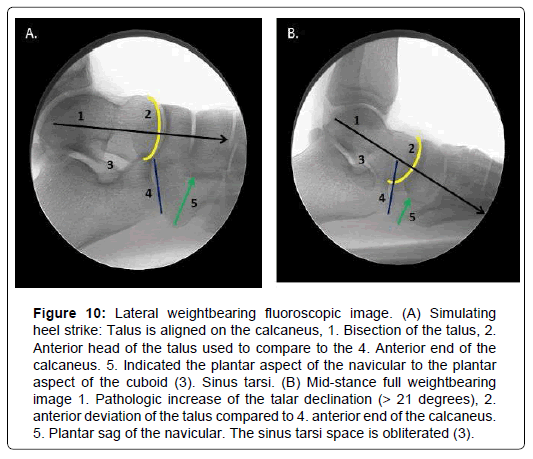
Subtalar joint instability leads to the dynamic displacement of the talus on the calcaneus and/or navicular. During the gait cycle a reloading of joint forces occurs when the talus resupinates on the tarsal mechanism. The excessive subtalar joint motion will occur immediately after heel strike. The talus loses its normal stability and alignment on the tarsal mechanism (Figure 10). It will remain in an unlocked pronated position longer than it should during the weight bearing portion of the gait cycle. This leads to increased forces acting anteriorly [32]. The soft and osseous foot structures will be forced to compensate for the resulting excessive forces in an attempt to resupinate the talus for heel lift [33,34].
Figure 10: Lateral weightbearing fluoroscopic image. (A) Simulating heel strike: Talus is aligned on the calcaneus, 1. Bisection of the talus, 2. Anterior head of the talus used to compare to the 4. Anterior end of the calcaneus. 5. Indicated the plantar aspect of the navicular to the plantar aspect of the cuboid (3). Sinus tarsi. (B) Mid-stance full weightbearing image 1. Pathologic increase of the talar declination (> 21 degrees), 2. anterior deviation of the talus compared to 4. anterior end of the calcaneus. 5. Plantar sag of the navicular. The sinus tarsi space is obliterated (3).
The determination of subtalar joint stability and alignment can be assessed by non-weightbearing and weight bearing examination. However, it is difficult to quantify the degree of deformity from observer to observer. For that reason, the diagnosis of subtalar joint instability should be confirmed with standardized and validated weight bearing radiographic analysis. The dorsoplantar (DP) talar second metatarsal (T2M) angle is formed between the longitudinal bisection of the second metatarsal and the bisection of the talus. The T2M angle is a reliable measurement to determine rear- to forefoot alignment. Values > 16 degrees are considered a pathologic transverse plane deformity. This indicates an abnormal adduction of the talus and abduction of the forefoot [21,23].
The lateral weightbearing radiograph determines a sagittal plane component. The sinus tarsi space should be present or “open” in a foot with an aligned TTJ. There are no specific quantifiable measurements, but a partially obliterated sinus tarsi can be an indication of a misaligned subtalar joint. The talar declination angle (TD) is a quantifiable measurement formed by the bisection of the longitudinal axis of the talus and the plane of support. The accepted value for the TD angle is ≤ 21º [21,24,27]. Any value >21 degrees was considered abnormal.
Hallux valgus (HV) is a pathologic condition where there is a valgus rotation and abduction of the hallux on the first metatarsal. It is usually described as a deformity acquired by abnormal biomechanics at the first metatarsophalangeal joint (MPJ) [35]. HV is often believed to be caused by the use of improper or fashionable footwear [36]. However, this cannot be targeted as the primary reason as the deformity is not necessarily seen in all the population wearing such footwear. It has also been suggested that there exists a relationship between collapse of the medial longitudinal arch and development of HV [37]. It is further believed that intrinsic factors like pes planus, equinus, flexible or rigid pes planovalgus, rigid or flexible forefoot varus, hypermobility of the first metatarsal or a short first metatarsal can be some of the contributing factors that may lead to or exacerbate HV [9,38-41].
There exists much controversy as to the ideal “bunion” treatment [42]. The current HV treatment paradigm has been called into question due to a diversity of mid- and long-term outcomes [43,44]. This is due to the variability of post-treatment results. One of the potential complications of HV surgery is recurrence that is associated with the most common bunion correction techniques [45,46]. It has been said that there are so many different methods described to fix HV because there is lack of agreement on the correction of choice.
The primary goal of hallux valgus surgery is the realignment of the hallux and the 1st metatarsal. However, little attention is given to addressing any underlying or co-existing hindfoot pathology, such as subtalar joint instability. A connection between subtalar or TTJ instability and forefoot pathology has been identified [47]. Coskun et al. also found that “increasing HV angle and pathomechanical changes in the rear foot are correlated, resulting in increasing pain and thus decreasing functional status as well as decreasing quality of life” [48].
Functional hallux limitus and rigidus (HL/R) is 1st MPJ disorder also linked to pathologic hindfoot position/motion [49]. There is an impaction of the head of the first metatarsal into the base of the proximal phalanx resulting in joint spacing narrowing. This 1st MPJ disease is often reported as an osteoarthritis condition. The tissue destruction is due to the years of “wear-and-tear” on the 1st MPJ due to excessive joint forces.
The data from this study helps to establish a connection that abnormal subtalar joint alignment is found in a majority of patients diagnosed with 1st MPJ pathology. Ninety-two (88%) feet with HV and HL/R had higher than the normal values of at least one of the two measured angles. It stands to reason that hind foot instability leads to a prolonged period of instability of the joints of the mid and forefoot and can increase the forces acting on the 1st MPJ during the gait cycle.
In a cadaver study by Graham et al. it was shown that stabilization of the subtalar joint led to a reduction of excessive abnormal forces acting on the middle and anterior talocalcaneal joint [31]. This should also lead to decreased strain on the osseous structures and soft tissues of the medial column of the foot. Arangio et al. showed 37% load under the 1st MPJ in a “flat foot” compared to 12% load for a normal foot [34]. Thus, reduction in pathologic forces acting on the medial column should lead to a reduction in secondary deformities associated with the medial column. The majority of the patient’s in this study had some form of talotarsal joint pathologic measurement indicating an excessive pronating subtalar joint. As Gould concluded in his study “Hyperpronation may exist without pes planus but, pes planus rarely is present without some degree of hyperpronation”. Not all patients with a hyperpronating subtalar joint will have a lower than normal arch. That is because it is possible to have subtalar joint pronation without the navicular dropping and a normal or higher than normal calcaneal inclination angle [50].
It has been the author’s experience that the use of a sinus tarsi stent to stabilize the hind foot has had a positive effect in reducing mild increases the 1st intermetatarsal angle. Other times, it is possible to perform the sinus tarsi stent insertion, observe a reduction of the 1st intermetatarsal angle. If there is not a reduction, then an appropriate form of surgical correction can be performed as a staged procedure. Finally, there are other situations where a semi-rigid or fixed deformity of 1st metatarsocuneiform joint requires surgical intervention at the same surgical setting.
A similar approach to hallux limitus can be offered to a patient. This depends on the degree of the deformity. Hind foot stabilization with a sinus tarsi stent should have a positive effect to the 1st MPJ range of motion. More research is required to substantiate this claim, but the biomechanics make sense as the talus shifts distally ultimate force the head of the 1st metatarsal into the base of the proximal phalanx. Again, a semi-rigid or rigid loss of motion at the 1st MPJ would require additional surgical intervention.
A limitation of this study was that only weight bearing radiographs were evaluated and clinical observations were not available. The clinical range of motion measurements taken would be purely subjective rather than the objective data from standardized weight bearing radiographs and therefore non-contributory to the study. Clinical grading of the severity of the HV and HL/R was not taken into consideration. Yet, the patient’s symptoms and 1st MPJ deformity was such that surgical intervention was desired for all participants in the study.
This study did not evaluate the presence or absence an equinus component, but that was not the purpose of this study. Further research is needed to evaluate the role, if equinus would contribute to 1st MPJ pathology. Another limitation was the failure to exclude acute traumatic episode that contributed to the 1st MPJ disease. It cannot be assumed that all of the feet had atraumatic induced 1st MPJ deformity. None of the patients included had a specific recollection of a traumatic episode that led to their 1st MPJ deformity.
The body-mass-index (BMI) is another factor that can be taken into consideration. The greater the BMI, the greater the forces acting on the 1st MPJ. This data was not factored into this study but would be interesting to note. One would assume that a greater BMI would result in an increase force acting on the anterior rather than the posterior joint facets in a patient with subtalar joint instability.
Conclusion
The data from this study supports the hypothesis that a significant number of feet diagnosed with HV and HL/R also have subtalar joint instability. While the exact nature of any clinical significance is to be determined, there is an argument to be made that the “hindfoot controls the forefoot” and it is possible that excessive hindfoot motion could lead to increased forces acting on the 1st MPJ. These increased forces could play a role in the progression of a pre-existing 1st MPJ misalignment and reduction of those excessive forces should be a consideration in the treatment of 1st MPJ disease.
Availability of data and materials
The data that supports the findings of this study is included in the article.
Author contributions
Conception: MEG; Design of the study: MEG, LK, HK; Analysis and interpretation of data: LK; Literature search: MEG, LK; All authors contributed to the drafting the article and revising it critically for important intellectual content.
Consent for publication
The participants consented to the utilization of their data for the purposes of this scientific study.
Role of the funding source
There was no funding for this manuscript.
Competing interests
The authors declare that they have no competing interests.
References
- Meyr AJ, Adams ML, Sheridan MJ, Ahalt RG (2009) Epidemiological aspects of the surgical correction of structural forefoot pathology. J Foot Ankle Surg 48: 543-51.
- Menz HB, Roddy E, Marshall M, Thomas MJ, Rathod T, et al. (2015) Demographic and clinical factors associated with radiographic severity of first metatarsophalangeal joint osteoarthritis: Cross-sectional findings from the clinical assessment study of the foot. Osteoarthritis Cartilage 23: 77-82.
- Yamamoto Y, Yamaguchi S, Muramatsu Y, Terakado A, Sasho T, et al. (2016) Quality of life in patients with untreated and symptomatic hallux valgus. Foot Ankle Int 37: 1171-1177.
- McPoil T, Cornwall MW (1994) Relationship between neutral subtalar joint position and pattern of rearfoot motion during walking. Foot Ankle Int 15: 141-145.
- Piazza SJ (2005) Mechanics of the subtalar joint and its function during walking. Foot Ankle Clin 10: 425-442.
- Golightly YM, Hannan MT, Dufour AB, Hillstrom HJ, Jordan JM (2014) Foot disorders associated with overpronated and oversupinated foot function: The Johnston county osteoarthritis project. Foot Ankle Int 35: 1159-1165.
- Wong DW, Zhang M, Yu J, Leung AK (2014) Biomechanics of first ray hypermobility: an investigation on joint force during walking using finite element analysis. Med Eng Phys 36: 1388-1393.
- Van Boerum DH, Sangeorzan BJ (2003) Biomechanics and pathophysiology of flat foot. Foot Ankle Clin 8: 419-430.
- Kalen V, Brecher A (1988) Relationship between adolescent bunions and flatfeet. Foot Ankle Int 8: 331-336.
- Geng X, Wang C, Ma X, Wang X, Huang J, et al. (2015) Mobility of the first metatarsal-cuneiform joint in patients with and without hallux valgus: In vivi three-dimensional analysis using computerized tomography scan. J Orthop Surg Res 10: 140.
- Dayton P, Feilmeier M, Hirschi J, Kauwe M, Kauwe JS (2014) Observed changers in radiographic measurements of the first ray after frontal plane rotation of the first metatarsal in a cadaveric foot model. J Foot Ankle Surg 53: 274-278.
- King DM, Toolan BC (2004) Associated deformities and hypermobility in hallux valgus: An investigation with weightbearing radiographs. Foot Ankle Int 25: 251-255.
- Arangio GA, Phillippy DC, Xiao D, Gu WK, Salathe EP (2000) Subtalar pronation: Relationship to the medial longitudinal arch loading in the normal foot. Foot Ankle Int 21: 216-220.
- Gatt A, Mifsud T, Chockalingam N (2014) Severity of pronation and classification of first metatarsophalangeal joint dorsiflexion increases the validity of the hubscher manoeuvre for the diagnosis of functional hallux limitus. Foot (Edinb) 24: 62-65.
- Van Gheluwe B, Dananberg HJ, Hagman F, Vanstaen K (2006) Effects of hallux limitus on plantar foot pressure and foot kinematics during walking. J Am Podiatr Med Assoc 96: 428-436.
- Munuera PV, Dingueq G, Palomo IC, Lafuente G (2006) Effects of rearfoot-controlling orthotic treatment on dorsiflexion of the hallux in feet with abnormal subtalar pronation: a preliminary report. J Am Podiatr Med Assoc 96: 283-289.
- Tarissi N, Vallee A, Dujardin F, Duparc F, Roussignol X (2014) Reducible valgus flat-foot: assessment of posterior subtalar joint surface displacement by posterior arthroscopy during sinus tarsi expansion screwing. Orthop Traumatol Surg Res 100: 395-399.
- Ravenell RA, Camasta CA, Powell DR (2011) The unreliability of the intermetatarsal angle in choosing a hallux abductovalgus surgical procedure. J Foot Ankle Surg 50: 287-92.
- Srivastava S, Chockalingam N, El Fakhri T (2010) Radiographic angles in hallux valugs: comparison between manual and computer-assisted measurements. J Foot Ankle Surg 49: 523-528.
- Menz HB, Munteanu SE (2005) Radiographic validation of the Manchester scale for the classification of hallux valgus deformity. Rheumatology (Oxford) 44: 1061-1066.
- Thomas JL, Kunkel MW, Lopez R, Sparks, D (2006) Radiographic values of the adult foot in a standardized population. J Foot Ankle Surg 45: 3-12.
- Bryant JA (2001) Comparison of radiographic foot measurements taken in two different positions. J Am Podiatr Med Assoc 91: 234-239.
- Graham ME, Chikka A, Jones PC (2011) Validation of the talar–second metatarsal angle as a standard measurement for radiographic evaluation. J Am Podiatr Med Assoc 101: 475-483.
- Gentili A, Masih S, Yao L, Seeger LL (1996) Pictorial review: Foot axes and angles. Br J Radiol 69: 968-974.
- Steel MJ, Johnson KA, DeWitz MA, Ilstrup DM (1980) Radiographic measurements of the normal adult foot. Foot Ankle Int 1: 151-155.
- Brockett CL, Chapman GJ (2016) Biomechanics of the ankle. Orthop Trauma 30: 232-238.
- Tiberio D (1987) The effect of excessive subtalar joint pronation on patellofemoral mechanics: a theoretical model. J Orthop Sports Phys Ther 9: 160-165.
- Picciano AM, Rowlands MS, Worrell T (1993) Reliability of open and closed kinetic chain subtalar joint neutral positions and navicular drop test. J Orthop Sports Phys Ther 18: 553-558.
- Sell KE, Verity TM, Worrell TW, Pease BJ, Wigglesworth J (1994) Two measurement techniques for assessing subtalar joint position: A reliability study. J Orthop Sports Phys Ther 19: 162-167.
- Donatelli RA (1985) Normal biomechanics of the foot and ankle. J Orthop Sports Phys Ther 7: 91-95.
- Graham ME, Parikh R, Goel VK, Mhatre D, Matyas A (2011)Â Stabilization of Joint Forces of the Subtalar Complex via HyProCure. J Am Podiatr Med Assoc 101: 390-399.
- Khamis S, Yizhar Z (2007) Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture 25: 127-134.
- Farokhmanes K, Shirzadian T, Mahboubi M, Shahri MN (2014) Effect of foot hyperpronation on lumbar lordosis and thoracic kyphosis in standing position using 3-dimensional ultrasound-based motion analysis system. Glob J Health Sci 6: 254-260.
- Arangio GA, Chopra V, Voloshin A, Salathe EP (2007) A biomechanical analysis of the effect of lateral column lengthening calcaneal osteotomy on the flat foot. Clin Biomec (Bristol. Avon) 22: 472-477.
- Glasoe WM, Nuckley DJ, Ludewig PM (2010) Hallux valgus and the first metatarsal arch segment: a theoretical biomechanical perspective. Phys Ther 90: 110-120.
- Nguyen US, Hillstron HJ, Li W, Dufour AB, Kiel DP, et al. (2010) Factors associated with hallux valgus in a population-based study of older women and men: The MOBILIZE Boston Study. Osteoarthritis Cartilage 18: 41-46.
- Burns PR, Mecham B (2014) Biodynamics of hallux abductovalgus etiology and preoperative evaluation. Clin Podiatr Med Surg 31: 197-212.
- Eustace S, Byrne JO, Beausang O, Codd M, Stack J, et al. (1994) Hallux valgus, first metatarsal pronation and collapse of the medial longitudinal arch: A radiological correlation. Skeletal Radiol 23: 191-194.
- Yamada S, Hirao M, Tsuboi H, Akita S, Matsushita M, et al. (2014) Involvement of valgus hindfoot deformity in hallux valgus deformity in rheumatoid arthritis. Mod Rheumatol 24: 851-854.
- Doty JF, Coughlin MJ (2013) Hallux valgus and hypermobility of the first ray: facts and fiction. Int Orthop 37: 1655-1660.
- Perera AM, Mason L, Stephens MM (2011) The pathogenesis of hallux valgus. J Bone Joint Surg Am 93: 1650-1661.
- Harrison WD, Walker CR (2016) Controversies and trends in the United Kingdom bunion surgery. Foot Ankle Clin 21: 207-217.
- Dayton P, Kuawe M, Feilmeier M (2015) Is our current paradigm for evaluation and management of the bunion deformity flawed? A discussion of procedure philosophy relative to anatomy. J Foot Ankle Surg 54: 102-111.
- Chong A, Nazarian N, Chandrananth J, Tacey M, Shepherd D, et al. (2015) Surgery for the correction of hallux valgus: minimum five-year results with a validated patient-reported outcome tool and regression analysis. Bone Joint J 97: 208-214.
- Jeuken RM, Schotanus MG, Kort NP, Deenik A, Jong B, et al. (2016) Long-term follow-up of a randomized controlled trial comparing scarf to chevron osteotomy in hallux valgus correction. Foot Ankle Int 37: 687-695.
- Bock P, Kluger R, Kristen KH, Mittlbock M, Schuh R, et al. (2015) The scarf osteotomy with minimally invasive lateral release for treatment of hallux valgus deformity: Intermediate and long-term results. J Bone Joint Surg Am 97: 1238-1245.
- Silva RS, Ferreira AL, Veronese LM, Serrao FV (2014) Forefoot varus predicts subtalar hyperpronation in young people. J Am Podiatr Med Assoc 104: 594-600.
- Coskun G, Talu B, Bek N, Mayramlar KY (2016) Effects of hallux valgus deformity on rear foot position, pain, function, and quality of life of women. J Phys Ther Sci 28: 781-787.
- Harradine PD, Bevan LS (2000) The effect of rearfoot eversion on maximal hallux dorsiflexion. A preliminary study. J Am Podiatr Med Assoc 90: 390-393.
- Gould N (1983) Evaluation of hyperpronation and pes planus in adults. Clin Orthop Relat Res 181: 37-45.
Citation: Graham ME, Kolodziej L, Kimmel HM (2018) The Frequency of Subtalar Joint Instability in Adult Patients Who Underwent Surgical Correction of First Metatarsophalangeal Joint Surgery-a Retrospective Radiographic Evaluation. Clin Res Foot Ankle 6: 280.
Copyright: © 2018 Graham ME, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3180
- [From(publication date): 0-2015 - Dec 01, 2025]
- Breakdown by view type
- HTML page views: 2363
- PDF downloads: 817