Short Communication Open Access
The Feasibility of eHealth in Mental Health Care
Syaron Basnet1,2*, Manu Tamminen3 and Tuuli Lahti1,21National Institute for Health and Welfare, Department of Mental Health and Substance Abuse Services, Helsinki, Finland
2Faculty of Social Sciences, Department of Behavioural Sciences and Philosophy, University of Turku, Finland
3Department of Food and Environmental Sciences, University of Helsinki, Finland
- Corresponding Author:
- Syaron Basnet
National Institute for Health and Welfare
Department of Mental Health and Substance Abuse Services
Helsinki Finland, P.O. Box 30
FI-00271 Helsinki, Finland
Tel: +358443223660
E-mail: syaronbasnet@gmail.com
Received date: October 15, 2014; Accepted date: December 15, 2014; Published date: December 20, 2014
Citation: Basnet S, Tamminen M, Lahti T (2014) The Feasibility of eHealth in Mental Health Care. J Addict Res Ther 5:205. doi:10.4172/2155-6105.1000205
Copyright: © 2014 Basnet S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Addiction Research & Therapy
Abstract
Currently, eHealth is widely used in mental health care. Most eHealth services have been developed for mental health care due to its distinctive features such as privacy, accessibility, affordability, acceptability, and cost-efficiency. This review summarizes existing literature on the feasibility of eHealth in mental health care and discusses its pros and cons as a service delivery tool. To conduct a systematic literature search, over 11000 articles were retrieved from PubMed and Medline. The keywords used in eHealth studies are diverse: according to the two databases, eHealth and mHealth are the most common ones. To date, a variety of eHealth applications have been developed for obsessive-compulsive disorders, phobias and other common mental health problems such as depression, anxiety, panic disorder, and generalized anxiety disorder. Both short and long-term positive outcomes have been reported when using these applications. eHealth has potential to overcome the fear of shame, guilt, and stigma, which are common concerns of mental health patients. However, licensing, ethical standards and guidelines for eHealth applications in mental health care is urgently needed as currently the rapid proliferation and commercialization of unproven electronic materials reduce the liability of eHealth services.
Keywords
eHealth; Mental health care; Feasibility; Ethical standards
Background
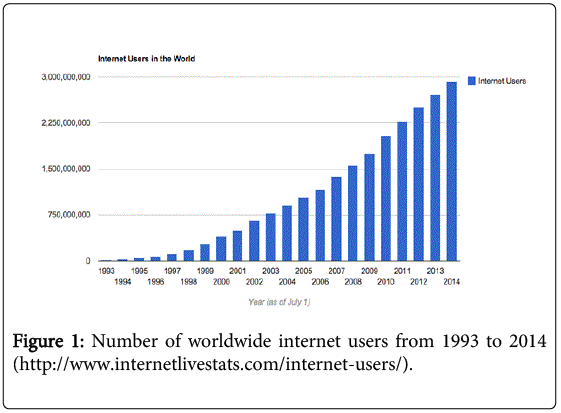
The concept of eHealth, as defined by the World Health Organization (WHO), is the use of information and communication technologies (ICT) in support of health and health–related fields including health care services, health surveillance, literature, and education, knowledge and research [1]. High accessibility makes Internet (Figure 1) a particularly good ICT platform for eHealth by lowering the threshold for help-seeking and enabling services to be delivered independently of time and place [2].
Figure 1: Number of worldwide internet users from 1993 to 2014 (http://www.internetlivestats.com/internet-users/).
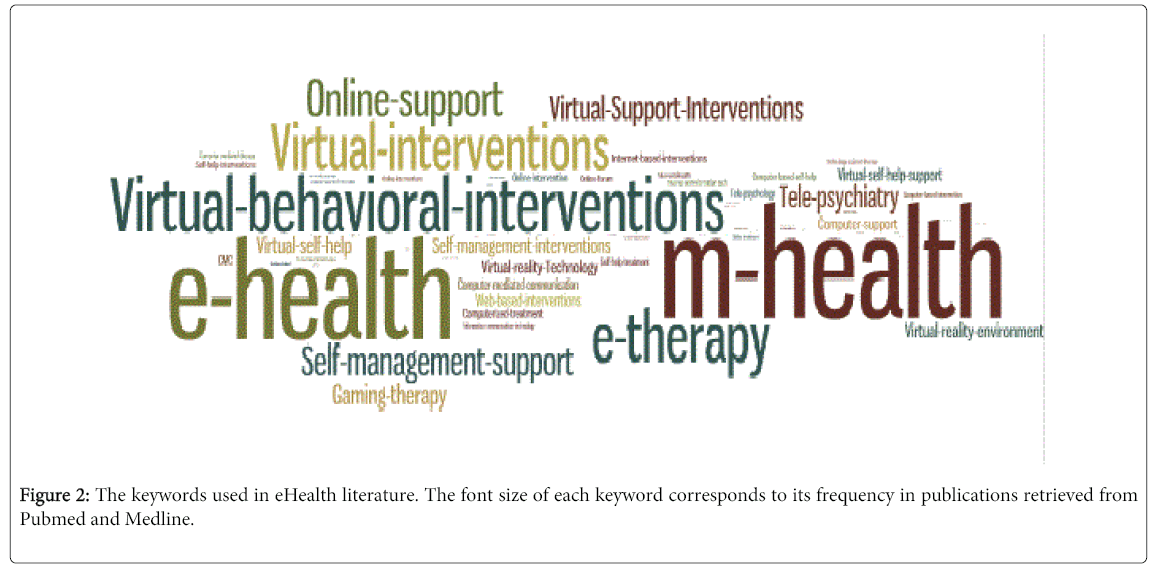
Current terminology related to eHealth is diverse. Extensive literature searches carried out by the first author between July and September 2014 in the databases of Pubmed and Medline (covering a majority of publications in mental health field) revealed more than 11000 articles related to eHealth in mental health care. The keywords used in these articles are diverse, with eHealth and mHealth being the most common ones (Figure 2).
Distant communication between a therapist and a client is not a new concept: already in 19th century Sigmund Freud extensively used letters to communicate with his clients [3]. Since the first study of eHealth in 1977 [4], helplines became the means of delivery, and in the 21st century Internet became the most common platform for eHealth services, permitting the use distant communication on a large scale for health care service delivery.
Most eHealth services have been developed for mental health care due to distinctive features such as privacy, accessibility, affordability, acceptability, and cost-efficiency [2,5-8]. This review summarizes existing literature on the feasibility of eHealth in mental health care and discusses its pros and cons as a service delivery tool.
eHealth in Mental Health Care
eHealth services have been developed for the treatment of a variety of mental health problems [9-20] as well as for the purposes of mental health promotion and education [21-23]. One of the first eHealth applications applied in mental health care was OC-Check, which was developed in 1987 to assist OCD patients in larger reduction of OCD symptoms by reminding instructions and tracking intensity of the obsessions [10]. Later in 1998, computer-aided vicarious exposure (CAVE) program was introduced to encourage OCD patients in self-management of their symptoms [24]. The same method has later been successfully used to treat other phobias such as fear of flying and glossophobia [9,25]. To date, a variety of eHealth applications have been developed for OCDs [10,11,26,27], phobias [15,16,29] and other common mental health problems such as depression [26,30,53], anxiety [54], panic disorder [12], and generalized anxiety disorder [12,28,29]. Both short and long-term positive outcomes have been reported when usi
ng these applications [12,28-35].
Pros of eHealth Applications in Mental Health Care
eHealth has a number of strengths in mental health care. First, eHealth applications reduce patients’ threshold to seek both information and help as eHealth can be utilized privately from home environment [7]. By providing anonymity, eHealth has the potential to overcome the fear of shame, guilt and stigma, which are common concerns of mental health patients [36,37]. Text-based communication via eHealth applications provides anonymity by removing social distinctions (such as disability, gender and age) [38] as well as non-verbal social cues (such as facial expressions, body language or vocal intonation) [39]. Further, text-based communication gives health care professionals and patients an opportunity to have more thorough and clear communication [39]. eHealth also provides a permanent record of the communication between patients and health care professionals [39] and hence allows proper monitoring and follow-up of the patients’ situation.
Second, eHealth is both accessible and affordable: most eHealth services are available 24/7 and often free of charge. When utilizing eHealth from home, the patients save also in travel expenses. Affordability of eHealth makes it an especially good option for patients with financial difficulties [36]. As eHealth can be used from home, it is applicable also for individuals with difficulties to travel, such as elderly and disabled people. The use of eHealth also reduces the expenses for the health care system [2,40]. Etter estimated that the total cost of implementing an eHealth application reaching 600 000 visitors per year per year is comparable to running a small smoking cessation clinic treating 600 patients per year [41].
Third, eHealth empowers the patients by giving them more responsibility over their own situation and activating them [42]. eHealth promotes self-monitoring, provides feedback and helps the patients to develop coping skills [43,44].By using mobile devices, help is at the hand all the time, which is often an important feature for the patients giving them the feeling of control over their symptoms [36]. eHealth has been shown to reduce both symptoms and clinician contact time as well as to increase patients’ adherence to the treatment, effectiveness even after years of follow up, improved quality of life, and increasing suitability to underserved population [14,45-51].
Fourth, applications of eHealth can easily be customized for the needs of different patient groups [36], for example separately for men and women or for different age groups. Customized content is more likely to be read, remembered and viewed as personally relevant and may thus increase the efficacy of eHealth services [52-54]. Lastly, eHealth provides sharing and networking possibilities among people with similar conditions: it promotes wellbeing by giving a sense of belonging within similar group of people who share similar problems [55].
Cons of eHealth Applications in Mental Health Care
A major weakness of eHealth is that it is not suitable for patients with low performance [56]. The use of eHealth requires initiative from the patients and thus severe physical or mental problems can prevent patients from using eHealth applications [15,56,57]. The convenient use of eHealth requires a certain degree of technical proficiency from both health care professionals and patients. This may leave especially elder patients outside the scope of eHealth.
In some cases relatively high dropout rates have been reported [58] and it has been suggested that anonymity may reduce the patients engagement in eHealth services [59]. This topic demands further attention to promote the patients’ adherence to eHealth services.
Licensing ethical standards and guidelines for eHealth in mental health care at an international level [60] is urgently needed as currently the rapid proliferation and commercialization of unproven electronic materials reduce the liability of eHealth services. Lee et al. [61] have identified five common ethical concerns of eHealth that should be addressed during the informed consent process i.e. addressing the concerns related to the use of eHealth, the possibility of misunderstanding, maintenance of professional boundaries, issues of confidentiality, and interruption of services.
Performance indicators and training manuals for health care professionals needs to be developed, addressing concerns such as patient privacy, patient safety, treatment adherence, data protection, and doctor-patient relationship. Finally, it is important to remember that technology needs maintaining and proper help-desk services are needed alongside the eHealth services.
Future of eHealth
Currently, more than 250 websites and e-clinics are offering eHealth services for mental health problems [62-64]. According to the American Psychiatric Association (APA), the trend in using eHealth in mental health care is increasing [65]. Some national and international standards for eHealth applications have been recently established. In United States, the ethical guidelines outlined by APA (2002) and the International Society of Mental Health Organization’s (2009) (ISMHO) helps to better organize and develop eHealth. In European Union (EU) electronic commerce Directive 2000/31/EC (E-commerce Directive) provides the legal framework for eHealth information dissemination [60]. In UK, all e-health operators working within National Health Services (NHS) needs to comply with the Department of Health’s confidentiality code of practice and guidelines on information security.
The current health care system has trained its professionals primarily for face-to-face treatment. However, due to the increasing demand for eHealth services, certified eHealth training programs for health care professionals need to be developed. Also the development and recognition of eHealth guidelines is of high importance. More studies are needed concerning patient satisfaction, safety considerations and long-term benefits of eHealth services [66].
References
- 58th World Health Assembly (2005)eHealth. World Health Organisation.
- Muñoz RF (2010) Using evidence-based internet interventions to reduce health disparities worldwide. J Med Internet Res 12: e60.
- Freud S (1992) Letters of Sigmund Freud.(E. L. Freud, editor.)Dover Publications INC.; Reprint edition (1 Feb 2000), p 470.
- Fisher LA, Johnson TS, Porter D, Bleich HL, Slack WV (1977) Collection of a clean voided urine specimen: a comparison among spoken, written, and computer-based instructions.Am J Public Health 67: 640-644.
- Newman MG, Szkodny LE, Llera SJ, Przeworski A (2011) A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: is human contact necessary for therapeutic efficacy? ClinPsychol Rev 31: 89–103.
- Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, et al. (2006) Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.Health Technol Assess 10: iii, xi-xiv, 1-168.
- Ball MJ, Lillis J (2001) E-health: transforming the physician/patient relationship.Int J Med Inform 61: 1-10.
- Newman MG1, Erickson T, Przeworski A, Dzus E (2003) Self-help and minimal-contact therapies for anxiety disorders: Is human contact necessary for therapeutic efficacy?J ClinPsychol 59: 251-274.
- North MM, North SM, Coble JR (1998) Virtual reality therapy: an effective treatment for phobias.Stud Health Technol Inform 58: 112-119.
- Baer L, Minichiello WE, Jenike MA (1987): Use of a portable-computer program in behavioral treatment of obsessive-compulsive disorder. Am J Psychiatry 144: 1101.
- Herbst N, Voderholzer U, Stelzer N, Knaevelsrud C, Hertenstein E, et al. (2012) The potential of telemental health applications for obsessive-compulsive disorder.ClinPsychol Rev 32: 454-466.
- Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N (2010) Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis.PLoS One 5: e13196.
- Christensen H, Reynolds J, Griffiths KM (2011) The use of e-health applications for anxiety and depression in young people: challenges and solutions.Early Interv Psychiatry 5 Suppl 1: 58-62.
- Carlbring P, Degerman N, Jonsson J, Andersson G (2012) Internet-based treatment of pathological gambling with a three-year follow-up.CognBehavTher 41: 321-334.
- Carlbring P, Smit F (2008) Randomized trial of internet-delivered self-help with telephone support for pathological gamblers.J Consult ClinPsychol 76: 1090-1094.
- Civljak M, Sheikh A, Stead LF, Car J (2010): Internet-based interventions for smoking cessation. Cochrane database Syst RevCD007078.
- Civljak M, Stead LF, Hartmann-Boyce J, Sheikh A, Car J (2013): Internet-based interventions for smoking cessation. Cochrane database Syst Rev 7: CD007078.
- Sharabi A, Margalit M (2010): The mediating role of internet connection, virtual friends, and mood in predicting loneliness among students with and without learning disabilities in different educational environments. J Learn Disabil 44: 215–27.
- Hill W, Weinert C, Cudney S (2006) Influence of a computer intervention on the psychological status of chronically ill rural women: preliminary results.Nurs Res 55: 34-42.
- Dominick SA, Irvine AB, Beauchamp N, Seeley JR, Nolen-Hoeksema S, et al. (2009) An internet tool to normalize grief.Omega (Westport) 60: 71-87.
- Overcoming (2008) Suns Des.
- Ecouch (2005)NatlInstMent Heal Res AustNatl Univ.
- Beating the blues (2006)Ultrasis.
- Clark A, Kirkby KC, Daniels BA, Marks IM (2009) A pilot study of computer-aided vicarious exposure for obsessive-compulsive disorderInforma UK Ltd UK.
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition: DSM-IV-TR®,4th ed. te. Washington DC: American Psychiatric Press.
- BT Steps (2014) Waypoint Heal Innov
- Swinburne University of Technology.OCD STOP.
- TheMoodGYM (2004)NatlInstMent Heal Res AustNatl Univ.
- Hedman E, Andersson G, Ljótsson B, Andersson E, Rück C et al. (2011) Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: a randomized controlled non-inferiority trial. PLoS One 6: e18001.
- Herbst N, Voderholzer U, Stelzer N, Knaevelsrud C, Hertenstein E, et al. (2012) The potential of telemental health applications for obsessive-compulsive disorder.ClinPsychol Rev 32: 454-466.
- Lovell K, Fullalove L, Garvey R, Brooker C (2000) Telephone treatment of obsessive-compulsive disorder. BehavCognPsychother 28: 87–91.
- Moritz S, Jelinek L,Hauschildt M, Naber D (2010): Cómotratar lo intratable? Eficacia de un programa de auto-ayuda de entrenamientometacognitivo (miEMC) para el trastornoobsesivo-compulsivo. Dialogues ClinNeurosci 12: 209–220.
- Muroff J, Steketee G, Himle J, Frost R (2010) Delivery of internet treatment for compulsive hoarding (D.I.T.C.H.).Behav Res Ther 48: 79-85.
- Himle JA, Fischer DJ, Muroff JR, Van Etten ML, Lokers LM, et al. (2006) Videoconferencing-based cognitive-behavioral therapy for obsessive-compulsive disorder.Behav Res Ther 44: 1821-1829.
- Comer JS, Furr JM, Cooper-Vince CE, Kerns CE, Chan PT, et al. (2014) Internet-delivered, family-based treatment for early-onset OCD: a preliminary case series.J Clin Child AdolescPsychol 43: 74-87.
- Labrie RA, Peller AJ, Laplante DA, Bernhard B, Harper A, et al. (2012) A brief self-help toolkit intervention for gambling problems: a randomized multisite trial.Am J Orthopsychiatry 82: 278-289.
- Davison KP, Pennebaker JW, Dickerson SS (2000) Who talks? The social psychology of illness support groups.Am Psychol 55: 205-217.
- Burgstahler S, Doyle A (2005) Gender Differences in Computer-Mediated Communication Among Adolescents with Disabilities: A Case Study. Disabil Stud Q 25:
- Murphy LJ, Mitchell DL (1998) When writing helps to heal: E-mail as therapy. Br J GuidCounc 26: 21–32.
- McCrone P, Knapp M, Proudfoot J, Ryden C, Cavanagh K, et al. (2004) Cost-effectiveness of computerised cognitive-behavioural therapy for anxiety and depression in primary care: randomised controlled trial.Br J Psychiatry 185: 55-62.
- Etter JF (2005) Comparing the efficacy of two Internet-based, computer-tailored smoking cessation programs: a randomized trial.J Med Internet Res 7: e2.
- Sood S, Mbarika V, Jugoo S, Dookhy R, Doarn CR, et al. (2007) What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings.Telemed J E Health 13: 573-590.
- Wright JH, Wright AS (1997) Computer-assisted psychotherapy.J PsychotherPract Res 6: 315-329.
- Arrow A (2009) Best Cognitive Behavioral Therapy (CBT) iPhone and Android App - cbtreferee.com.
- Hodgins DC, Currie SR, el-Guebaly N (2001) Motivational enhancement and self-help treatments for problem gambling.J Consult ClinPsychol 69: 50-57.
- Rodda S, Lubman D, Dowling NA, Bough A, Jackson AC (2013) Web-based counseling for problem gambling: exploring motivations and recommendations.J Med Internet Res 15: e99.
- Petry NM, Weinstock J, Morasco BJ, Ledgerwood DM (2009) Brief motivational interventions for college student problem gamblers.Addiction 104: 1569-1578.
- Wood RT, Griffiths MD, Parke J (2007) Acquisition, development, and maintenance of online poker playing in a student sample.CyberpsycholBehav 10: 354-361.
- Andrews G, Titov N (2010) Is internet treatment for depressive and anxiety disorders ready for prime time?Med J Aust 192: S45-47.
- Bennett K, Reynolds J, Christensen H, Griffiths KM (2010) e-hub: an online self-help mental health service in the community.Med J Aust 192: S48-52.
- Eells TD, Barrett MS, Wright JH, Thase M (2014) Computer-assisted cognitive-behavior therapy for depression.Psychotherapy (Chic) 51: 191-197.
- Brug J, Campbell M, van Assema P (1999) The application and impact of computer-generated personalized nutrition education: a review of the literature.Patient EducCouns 36: 145-156.
- Dijkstra A, De Vries H (1999) The development of computer-generated tailored interventions.Patient EducCouns 36: 193-203.
- Watts S, Mackenzie A, Thomas C, Griskaitis A, Mewton L, et al. (2013) CBT for depression: a pilot RCT comparing mobile phone vs. computer.BMC Psychiatry 13: 49.
- Hinton L, Kurinczuk JJ, Ziebland S (2010) Infertility; isolation and the Internet: a qualitative interview study.Patient EducCouns 81: 436-441.
- Choi NG, Dinitto DM (2013) The digital divide among low-income homebound older adults: Internet use patterns, eHealth literacy, and attitudes toward computer/Internet use.J Med Internet Res 15: e93.
- Kohl LF, Crutzen R, de Vries NK (2013) Online prevention aimed at lifestyle behaviors: a systematic review of reviews.J Med Internet Res 15: e146.
- Moreira Tde C, Signor L, Figueiró LR, Fernandes S, Bortolon CB, et al. (2014) Non-adherence to telemedicine interventions for drug users: systematic review.Rev SaudePublica 48: 521-531.
- Clarke AM, Kuosmanen T, Barry MM (2014) A Systematic Review of Online Youth Mental Health Promotion and Prevention Interventions.J Youth Adolesc .
- Kelly B (2011)E-health:ethical and data privavcy challenges in EU. Inf UK Ltd.
- Lee S (2010) Contemporary Issues of Ethical E-therapy. J Ethics Ment Heal 5
- Ainsworth M (2001a) E-therapy: history and survey.
- Dunaway O (2000) Assessing the potential of online psychotherapy. Psychiatr Times
- Grohol J(1999a) Best practices in e-therapy: Definition and scope of etherapy.
- American Psychological Association Monitor (2010) Am Psychol Assoc.
- Rabius V, Pike KJ, Wiatrek D, McAlister AL (2008) Comparing internet assistance for smoking cessation: 13-month follow-up of a six-arm randomized controlled trial.J Med Internet Res 10: e45.
Relevant Topics
- Addiction Recovery
- Alcohol Addiction Treatment
- Alcohol Rehabilitation
- Amphetamine Addiction
- Amphetamine-Related Disorders
- Cocaine Addiction
- Cocaine-Related Disorders
- Computer Addiction Research
- Drug Addiction Treatment
- Drug Rehabilitation
- Facts About Alcoholism
- Food Addiction Research
- Heroin Addiction Treatment
- Holistic Addiction Treatment
- Hospital-Addiction Syndrome
- Morphine Addiction
- Munchausen Syndrome
- Neonatal Abstinence Syndrome
- Nutritional Suitability
- Opioid-Related Disorders
- Relapse prevention
- Substance-Related Disorders
Recommended Journals
Article Tools
Article Usage
- Total views: 17562
- [From(publication date):
December-2014 - Jul 06, 2025] - Breakdown by view type
- HTML page views : 12828
- PDF downloads : 4734