The Exposure Risk of Covid-19: HCWs are Threat to their Families; the Time to Take Action is Now
Received: 28-Jul-2020 / Accepted Date: 13-Aug-2020 / Published Date: 17-Aug-2020
Abstract
The recent emergence of a new respiratory disease called COVID-19 from a metropolitan city of the Hubei Province of China, called Wuhan, in December 2019, demonstrated its epidemic potential with a rapid spread of this virus across the globe in just two months period. This highlights the higher rate of transmissibility of this virus and further its higher morbidity and mortality, especially in aged population or people with co-morbidities and/or immune gap.
COVID-19 is a highly contagious respiratory disease that is caused by novel corona virus. Its main clinical symptoms are fever, dry cough, fatigue, myalgia and dyspnea. In Pakistan the literature so for covering the prevalence and incidence is deficient. In Pakistan the so for (24th July 2020) reported data from government sources declares 270,400 confirmed cases with 5763 deaths. 219783 cases are recovered so for and 1316 cases are under treatment in high dependency units countrywide. Sindh is the province with highest number of corona cases crossing 115883.
The early available information’s so for concluded that Health Care workers (HCW) are at increased risk of contracting the corona infection ranging from 15-18% and in some cases up to 20%. Major contributing factors are inadequate availability of the Personal Protective Equipment’s (PPE), uncertain diagnosis, non-availability of the diagnostic facilities in all health care centers and related psychological stress while working in COVID-19 treatment facilities.
Another study concluded that the exposure risk of health care workers was higher than general population and they experienced a risk of transmission of the disease to their families, though the rate of transmission of the disease was lower.
In present study we analyzed the data of COVID-19 surveillance system of our teaching hospital to see the prevalence of infection (COVID-19) in HCWs and contribution of family contacts in transmission of this deadly disease.
Methodology
This cross-sectional study was conducted from 20th February to 30th May, M2020 at Medical Teaching Institution, Qazi Hussain Ahmed Medical Complex, Nowshera.
The sample was selected through consecutive, non-probability technique. All the patients from COVID clinics, or strong suspects with history of close contacts of COVID-19 positive patients, with PCR report received from the Khyber Medical University, Public Health Research Laboratory, irrespective of age and gender, were randomly selected [1-6].
All patients attended in emergency or outdoor patient’s department were excluded. Similarly, patients attending the COVID-19 clinic without securing the optimum marks for selection to be enrolled of PCR testing were also excluded.
Ethical endorsement was obtained from the institutional ethical review board of Nowshera Medical College Hospital administration before the execution of the study. Prior informed consent was obtained from all suspects and they were assured of confidentiality.
Seventy (70%) of the cases were selected from COVID-19 clinic of Qazi Hussain Ahmed Medical Complex; however, the patients whose PCR was sent by the district health authorities were also included from the available district line list.
All samples were sent under strict observance of protocols to the Public Health Research Laboratory of Khyber Medical University Peshawar (a designated Lab for PCR of nCoV-2019).
All of these patients, whose samples were collected, had been isolated mainly in the isolation unit of our hospital as well as designated quarantine areas; very few cases were allowed home isolation under strict observance of the health/district administration to contain the spread of the virus.
Results were received in 2-3 days, all with positive PCR reports were isolated and kept under treatment, and their samples were repeated after 7 days of isolation/treatment. Those who were negative in repeated sample reporting were shifted to quarantine; one case that reported positive on second phase belonging to Karachi was kept under strict isolation.
Data were entered in SPSS 25th version and descriptive and correlation statistics were applied. The frequency and proportion of numerical and categorical variables were presented in percentages. 2-D line graph were designed from the data to show the frequency/ contribution of the HCW and family contact in COVID-19.
Results
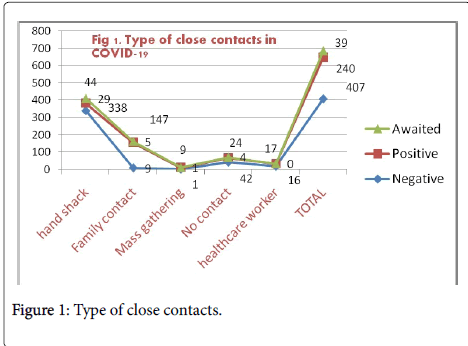
We observed that out of total cases screened 240(34.68%) were COVID-19 confirmed patients and 407(58.8%) were negative (Table 1).
| Frequency of Health care workers and family contacts in COVID-19 | ||||||
|---|---|---|---|---|---|---|
| Type of contact | Total | |||||
| PCR Result | Hand shack | Family member/contacts | Mass gathering | No contact | Health care worker | |
| Negative | 338 | 9 | 1 | 42 | 17 | 407 |
| Positive | 44 | 147 | 9 | 24 | 16 | 240 |
| Awaited | 29 | 5 | 1 | 4 | 0 | 39 |
| Not done | 0 | 0 | 0 | 3 | 0 | 3 |
| Inconclusive | 0 | 3 | 0 | 0 | 0 | 3 |
| Total | 411 | 164 | 11 | 73 | 33 | 692 |
Table 1: Frequency of Health care workers and family contacts in COVID-19.
Our findings are still comparably lower than Qiu H et al6 who reported (89%) positive cases from the suspects with history of exposure to COVID-19 positive patients in China.
The contribution of health care workers as profession to acquire infection was 17/240(7.08%). Family contacts as part of the close contact was major factor for transmission of the disease )147/240, 61%) (Figure 1).
The data reports the HCWs who had no PPEs or re-using the same PPE are at a significantly higher risk of contracting the COVID-19 infection. However, adequate supplies of PPE did not completely mitigate high-risk exposures [7].
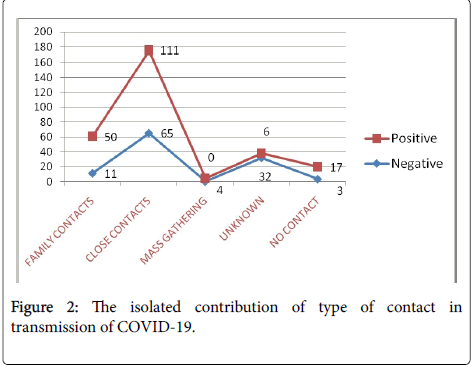
While among the type of contacts the isolated contribution of family contact was 50/240 (20.83%). (Figure 2).
This further stamp the importance of the positive contact history of the healthcare worker who is considered to be potential sources of transmission of the disease from the health care facility to homes. In China where unprecedented measures were taken well in time to control the rapid spread of COVID-19 epidemics in china. They succeeded to adhere people to homes that was properly achieved by their improved Knowledge, attitude and practices towards COVID-19 [8].
The rate of infectivity depends widely on the incubation period that is reported between 2-14 days in the literature and also on the duration of exposure and also on the immune status of the patient to acquire infection [6].
Discussion
The current situation will not go away overnight “it’s a marathon and not the sprint”. The policy makers should focus on long term occupational capacity rather than repeated short-term crisis response plans.
The key message from this short communication in to “Pay respect to HCWs” that put themselves and their families at risk for the health and safety of the general community. The government should take strict and urgent measure to provide PPEs to the health care worker and also to ensure their safety, they must be honored and supported as in many cases we noticed that the Sindh and Punjab government announced incentives and packages specially to the staff working in COVID-19 isolation. This would increase them well to work besides being their primary duty and their inside satisfaction.
Furthermore, early identification of the disease by enhancing the capacities of the tertiary care hospitals to perform PCR for 2019 nCoV detection, Antibodies detection, making strategies to design accurate triage system can reduce the risk of cross infection in COVID-19.
References
- Weston S, Frieman MB (2020) COVID-19: Knowns, Unknowns, and Questions. mSphere 5: 203-220.
- Chen N, Zhou M, Dong X, Qu J, Gong F (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395: 507-513.
- Ali S, Noreen S, Farooq I, Bugshan A, Vohra F (2020). Risk Assessment of Healthcare Workers at the Frontline against COVID-19. Pak J Med Sci, 36: 99-103.
- Dioscoridi L, Carrisi C (2020) Covid-19 exposure risk for family members of healthcare workers: an observational study, Int J Infect Dis 98: 287-289.
- Qiu H, Wu J, Hong L, Luo Y, Song Q (2020) Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID). Lancet Infect Dis 3099: 30198-30205.
- Nguyen LH, Drew DA, Joshi AD (2020) Risk of COVID-19 among frontline healthcare workers and the general community: a prospective cohort study. MedRxiv 29: 20084111.
- Zhong BL, Luo W, Li HM, Zhang QQ, Liu XG (2020) Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci 16: 1745-1752.
- De-Vitis R, Passiatore M, Perna A, Proietti L, Taccardo G (2020) COVID-19 contagion and contamination through hands of trauma patients: what risks and what precautions? J Hosp Infect 6701: 30175-30164.
Citation: Hamzullah Khan (2020) The Exposure Risk of Covid-19: HCWs are Threat to their Families; the Time to Take Action is Now. J Clin Exp Pathol 10: 381.
Copyright: © 2020 Khan H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2476
- [From(publication date): 0-2020 - Nov 17, 2025]
- Breakdown by view type
- HTML page views: 1645
- PDF downloads: 831