The Effects of Simultaneous Versus Staged Bilateral Femoral Intramedullary Nailing for Metastatic Disease on Survival Time and Perioperative Complications: A Systematic Review
Received: 29-Jun-2018 / Accepted Date: 16-Aug-2018 / Published Date: 23-Aug-2018 DOI: 10.4172/2472-016X.1000125
Keywords: Metastatic cancer; Intramedullary nailing; Timing; Reaming; Prophylactic; Outcomes
Introduction
Operative treatment of metastatic bone disease in the femur is challenging, as the surgeon must consider many patient factors when tailoring their approach to optimize benefits. One commonly used method to treat impending or acute pathological femoral fractures is intramedullary nailing (IMN). Insertion of intramedullary nails reduces the length of stay in hospital and promotes the patient’s independence at the end of life [1,2]. However, IMN carries a risk of fat embolism-a well-documented and sometimes fatal complication that arises when embolic substances from the tumor or bone marrow enter the circulation [3,4]. This risk appears to be more pronounced in the setting of femoral malignancy, where abnormal angiogenesis offers greater embolic access to venous circulation [4,5].
Bilateral intramedullary nailing may be occasionally needed in patients with impending or pathological fractures involving both femurs. However, the relative timing of these procedures has been a subject of debate [1,3]. Given the theoretically additive risk of fat emboli in patients undergoing bilateral IMN, several studies have recommended a staged approach to offset the higher risk of embolus under single anesthesia [4,5]. However, increased costs, limited operating room time, the need for early fixation, and the deteriorating condition of the patient may make staged operations less feasible [3]. Additionally, simultaneous nailing of both femurs precludes the potential complications and morbidity of a second operation [1].
Though IMN is generally regarded as a safe procedure, the associated complications-namely fat emboli-are well documented [6,7]. Femoral canal venting has been devised as a method to reduce the intramedullary pressure which is thought to mediate the increased risk of fat embolism syndrome in reamed intramedullary nails [8]. However, the effects of canal venting in IMN are considered theoretical and have yet to be studied closely.
The purpose of this study is, in the context of bilateral impending and pathological femoral fractures caused by metastatic cancer, to compare survival length and the rate of perioperative complications amongst patients who received simultaneous intramedullary nailing to those whose procedures were staged. The effects of femoral canal reaming, venting, and implant failure on intraoperative complications are also discussed as secondary outcomes of this study.
Methods
Eligibility
This systematic review is based upon raw data from case reports and cohort studies of bilateral femoral intramedullary nail fixation in patients with known metastatic malignancy. Studies were excluded if the length of time between the fixations of both femurs was unknown, the length of survival time was unknown, the femoral lesion was nonmetastatic, the outcomes were not listed by individual patients, and if other surgical interventions were performed concurrently.
Search strategy
The Preferred Reporting Item for Systematic Reviews and Meta- Analyses (PRISMA) statement was used for this study. The Cochrane Library, Medline, PubMed, and Scopus were searched to identify relevant literature. All articles until December 1st, 2017 were considered, and the language was limited to English and French.
Data collection
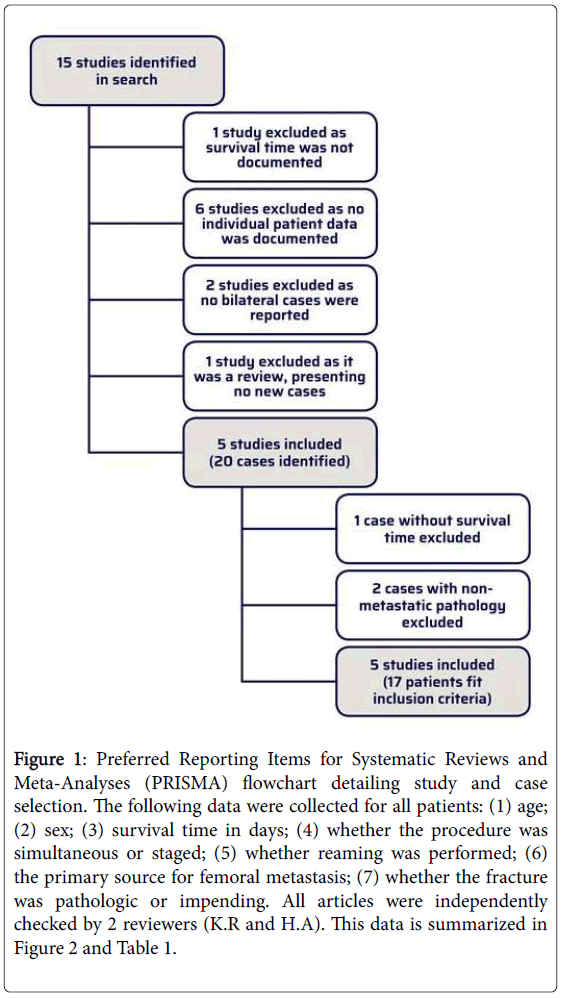
There were 15 studies identified and screened for relevance, ten of which were excluded. The remaining five full text articles were assessed for eligibility, and a total of 20 bilateral cases were identified. Three of these cases were excluded: one case did not describe an exact survival time and two cases did not have an established primary etiology. The remaining five studies and 17 bilateral femoral IMN cases were included in our analysis. The PRISMA flowchart is shown in Figure 1.
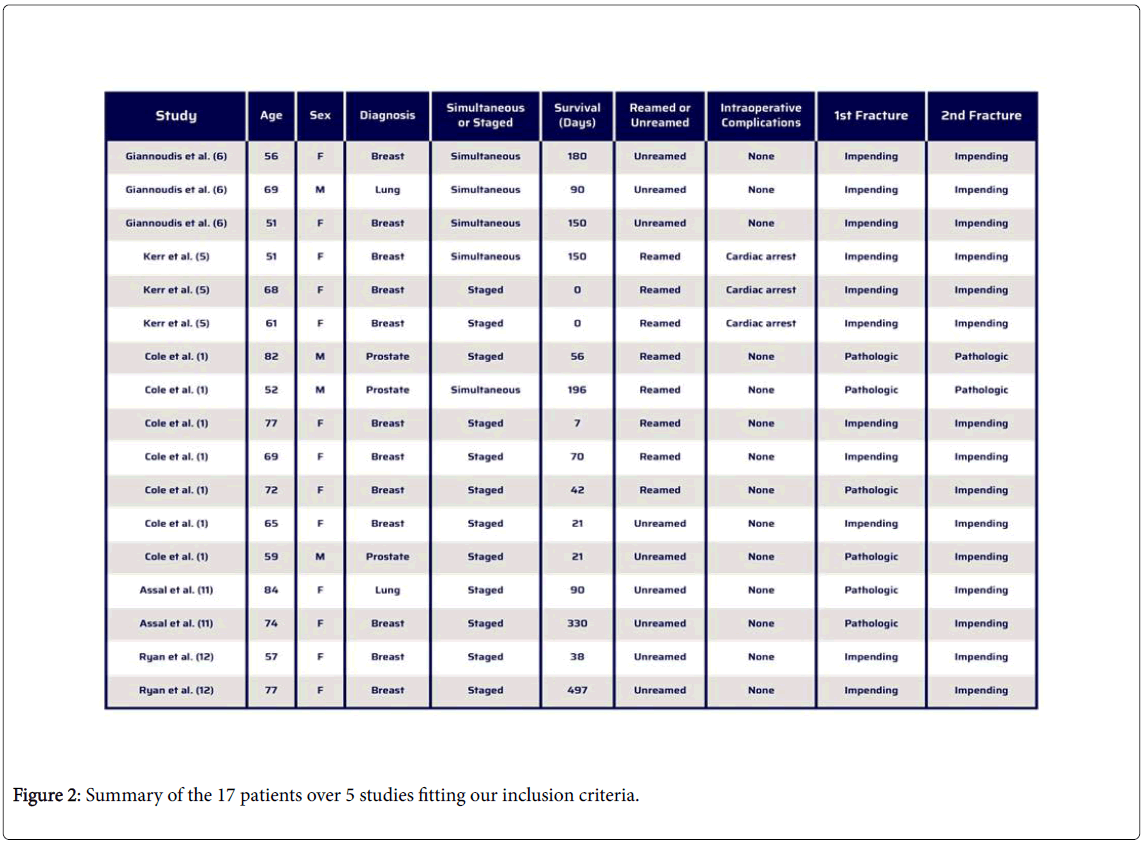
Figure 1: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart detailing study and case selection. The following data were collected for all patients: (1) age; (2) sex; (3) survival time in days; (4) whether the procedure was simultaneous or staged; (5) whether reaming was performed; (6) the primary source for femoral metastasis; (7) whether the fracture was pathologic or impending. All articles were independently checked by 2 reviewers (K.R and H.A). This data is summarized in Figure 2 and Table 1.
| Study | Age | Sex | Diagnosis | Simultaneous or Staged | Survival (Days) | Reamed or Unreamed | Intraoperative Complications | Canal venting |
|---|---|---|---|---|---|---|---|---|
| Giannoudis et al. [6] | 56 | F | Breast | Simultaneous | 180 | Unreamed | None | No |
| Giannoudis et al. [6] | 69 | M | Lung | Simultaneous | 90 | Unreamed | None | No |
| Giannoudis et al. [6] | 51 | F | Breast | Simultaneous | 150 | Unreamed | None | No |
| Kerr et al. [5] | 51 | F | Breast | Simultaneous | 150 | Reamed | Cardiac arrest | No |
| Kerr et al. [5] | 68 | F | Breast | Staged | 0 | Reamed | Cardiac arrest | No |
| Kerr et al. [5] | 61 | F | Breast | Staged | 0 | Reamed | Cardiac arrest | Yes |
| Cole et al. [1] | 82 | M | Prostate | Staged | 56 | Reamed | None | No |
| Cole et al. [1] | 52 | M | Prostate | Simultaneous | 196 | Reamed | None | No |
| Cole et al. [1] | 77 | F | Breast | Staged | 7 | Reamed | None | No |
| Cole et al. [1] | 69 | F | Breast | Staged | 70 | Reamed | None | No |
| Cole et al. [1] | 72 | F | Breast | Staged | 42 | Reamed | None | No |
| Cole et al. [1] | 65 | F | Breast | Staged | 21 | Unreamed | None | No |
| Cole et al. [1] | 59 | M | Prostate | Staged | 21 | Unreamed | None | No |
| Assal et al. [11] | 84 | F | Lung | Staged | 90 | Unreamed | None | No |
| Assal et al. [11] | 74 | F | Breast | Staged | 330 | Unreamed | None | No |
| Ryan et al. [12] | 57 | F | Breast | Staged | 38 | Unreamed | None | No |
| Ryan et al. [12] | 77 | F | Breast | Staged | 497 | Unreamed | None | No |
Table 1: Summary of the 17 patients over.
Outcomes measured
Clinical outcome was defined primarily by the patients’ survival time, namely the number of days after the placement of both intramedullary nails until death. Perioperative complications were a secondary outcome measure. Categorical data are presented as counts and percentages.
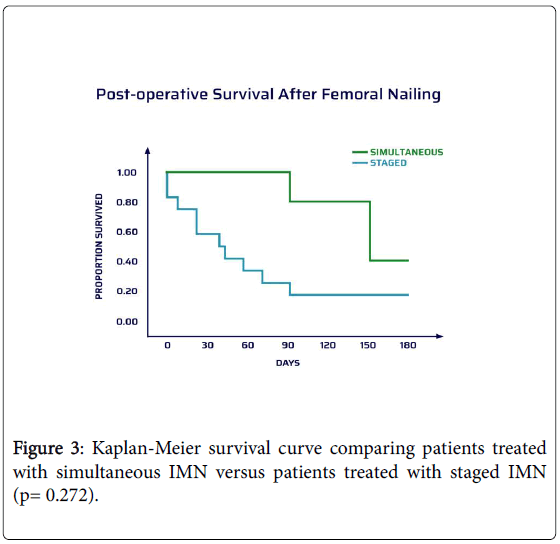
Statistical analysis
Data was analyzed using Microsoft Excel and R-Studio. The logrank test was used to reports differences in survival rates. Kaplan Meier survivorship curves were produced to differentiate between patients who had staged versus simultaneous procedures. Mean survival times were calculated and compared for reamed and unreamed patient subgroups.
Results
Demographics
The literature review yielded a total of 17 patients across five studies. Average age was 66.1 years and 76.4% were female. Breast cancer was found to be the primary malignancy in 12 patients (70%), followed by prostate (18%) and lung cancers (12%).
Simultaneous versus staged
Five of these patients were treated simultaneously while 12 were treated with staged procedures. The probability of surviving beyond 90 days was 100% for the simultaneous group compared to 25% for the staged group. Higher survival rates were shown up to 180 days for patients who underwent simultaneous nailing, demonstrated by the Kaplan Meier survivorship curves shown in Figure 3. However, this difference was not statistically significant (p=0.272). Two intraoperative deaths were observed in those treated with staged procedures while none were observed in those treated simultaneously. One patient who received simultaneous nails sustained intraoperative cardiac arrest and was revived; she survived for 150 days thereafter. No other post-operative complications were reported.
Reaming
Eight (47%) of the patients had undergone reaming while nine (53%) had received unreamed nails. On average, the patients treated with a reamed nail survived 65.1 days, while those who had not survived 157.4 days. All three patients who sustained an intraoperative cardiac arrest received reamed nails, while no complications were observed in the unreamed group.
Venting, implant failure and fracture type
Among 17 patients, one patient had femoral canal venting. Despite this, that patient had intraoperative cardiac arrest and subsequently deceased. No implant failure was observed. Eight out of the 34 IM nails were for pathological fractures; the remaining nails were for impending fractures [9,10].
Discussion
Authors in the orthopaedic oncology literature have cautioned against performing simultaneous bilateral nailing of metastatic lesions, citing the theoretically increased risk of cardiopulmonary complications [11-14]. This notion has perpetuated such that the standard recommendation has become to adopt a staged approach when bilateral nailing is required. However, there is a lack of robust evidence to support this advice, as the few studies on this topic describe a very low number of patients in a haphazard manner.
For example, an influential study by Kerr et al. [12] reported an incidence of 100% cardiac arrest in patients who received bilateral nailing. They concluded that bilateral nailing puts patients at high risk for embolic complications and that staged nailing should delayed for as long as possible [12]. However, this conclusion was drawn from only three patients who received bilateral nailing in this study, only one of which underwent a simultaneous procedure. Their recommendation regarding the increased benefits staged procedures may offer is inherently biased as well as illustrates the paucity of simultaneous bilateral femoral IMN data, demonstrating the need to evaluate the safety of both techniques in earnest.
Therefore, the purpose of our study was to compare the survival and perioperative complications of simultaneous versus staged IMN in bilateral femoral metastatic disease. Survivorship and perioperative complications were our primary and secondary clinical outcomes respectively. We note limitations to our study - the fact that the need for bilateral nailing is an uncommon event and the strict inclusion criteria our study has imposed to create an adequate comparison have both made the small study size unavoidable. Although no definitive conclusions can be drawn due to the low number of patients identified in the literature, simultaneous nailing can be considered safe and may give the patient better survivorship than previously expected.
Our evaluation of the literature shows that among the five patients who received simultaneous nailing, only one developed intraoperative complications. This patient was from the aforementioned Kerr et al. study [12] and developed cardiac arrest. However, this patient was revived and survived the operation. Moreover, all five patients in the simultaneous IMN group survived beyond 90 days postoperatively. In contrast, two of the 12 patients who received staged IMN died from intraoperative complications. We demonstrated higher survival rates for the simultaneous group up to 180 days than those in the staged group. However, the sample size was insufficient to demonstrate statistical significance. The low perioperative mortality of the simultaneous IMN group along with the higher survival when compared to the staged group appears to support Moon et al.’s findings, validating that the mortality rate of simultaneous fixation had previously been overestimated [10].
The results of a recent Canadian study emphasize the importance of earlier definitive treatment for patients with pathologic fractures [15]. Ristevski et al. demonstrated decreased blood loss, decreased length of stay in hospital, better patient function, and decreased one-year mortality in patients who underwent prophylactic fixation versus fixation of actual fractures [15]. This reported benefit of early fixation further favors simultaneous IMN, as patients would be stabilized earlier than a staged procedure. Additionally, one consolidated bilateral procedure would as reduce OR time and cost as well as avoid the potential complications and morbidity of a second operation.
Eight (47%) of the patients in the current study had undergone reaming while nine (53%) had received unreamed nails. All three patients who sustained an intraoperative cardiac arrest received reamed nails, while no complications and a higher average survival rate were observed in the unreamed group. There was no hardware failure reported, irrespective of whether the nail was reamed or not. Consequently, it may seem safer to avoid reaming, if possible, to reduce the risk of complications. If reaming is required, the use of a suction and irrigation reamer may be advisable. Currently, there is no literature to support a statically significant difference of perioperative complications between reamed and unreamed femoral nails [16].
The current orthopedic oncology literature recommends canal venting for pathological fractures to offset the rise in intramedullary pressure with nail fixation, thereby decreasing the risk of the patient sustaining a fat embolism [17-19]. However, our findings do not support these experimental studies. With regards to canal venting during femoral nail reaming and insertion, our results showed that 95% of patients did not receive canal venting, and more than 80% of patients survived the procedure without intraoperative complications. In fact, the only patient in whom canal venting was performed died secondary to fat embolism. We have shown that it is safe to perform femoral nail insertion without canal venting in patients with metastatic femoral lesions. However, new techniques such as reaming irrigating aspiration (RIA) show promise in that initial studies have supported their benefits, though further studies are still required [20].
Conclusion
This meta-analysis of current literature supports the safety of both staged and simultaneous bilateral femoral IMN for metastatic disease. The survival length and intraoperative complication rates are superior in simultaneous IMN than in staged IMN. However, the low number of patients did not permit statistical significance. Moreover, intraoperative complications have been observed only in patients who received reamed femoral nails, and canal venting added no benefits to minimize these complications. Therefore, although there has been concern about simultaneous treatment of bilateral femoral nailing in the literature, this study suggests that it can be safe. Simultaneous and unreamed bilateral nailing may allow for longer survivorship for patients and should be considered by the treating surgeon. Further studies are required to contribute towards clearer guidelines for the treatment of patients with bilateral femoral metastatic lesions.
References
- Hage WD, Aboulafia AJ, Aboulafia DM (2000) Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am 31: 515-528.
- Tanaka T, Imanishi J, Charoenlap C, Choong PFM (2016) Intramedullary nailing has sufficient durability for metastatic femoral fractures. World Journal of Surgical Oncology 14: 80.
- Shimoyama T, Katagiri H, Harada H, Murata H, Wasa J, et al. (2017) Fracture after radiation therapy for femoral metastasis: incidence, timing and clinical features. Journal of Radiation Research 58: 661-668.
- Riccio AI, Wodajo FM, Malawer M (2007) Metastatic carcinoma of the long bones. American family physician 76.
- Forsberg JA, Wedin R, Bauer H (2013) Which implant is best after failed treatment for pathologic femur fractures? Clin Orthop Relat Res 471: 735-740.
- Capanna R, Campanacci DA (2001) The treatment of metastases in the appendicular skeleton. J Bone Joint Surg Br 83: 471-481.
- Bohm P, Huber J (2002) The surgical treatment of bony metastases of the spine and limbs. J Bone Joint Surg Br 84: 521-529.
- Cole A, Hill G, Theologis T, Gibbons C, Willett K (2000) Femoral nailing for metastatic disease of the femur: a comparison of reamed and unreamed femoral nailing. Injury 31: 25-31.
- Arvinius C, Parra JL, Mateo LS, Maroto RG, Borrego AF, Stern LL (2014) Benefits of early intramedullary nailing in femoral metastases. Int Orthop 38: 129-132.
- Moon B, Lin P, Satcher R, Lewis V (2014) Simultaneous nailing of skeletal metastases: is the mortality really that high? Clinical Orthopaedics and Related Research 469: 2367-2370.
- Kontakis GM, Tossounidis T, Weiss K, Pape H-C, Giannoudis PV (2006) Fat embolism: special situations Bilateral femoral fractures and pathologic femoral fractures. Injury 37: S19-S24.
- Kerr P, Jackson M, Atkins R (1993) Cardiac arrest during intramedullary nailing for femoral metastases. Bone & Joint Journal 75: 972-973.
- Charnley G, Coleman N, Hashemi-Nejad A (1994) Cardiac arrest during nailing. Journal of Bone & Joint Surgery, British Volume;76-B: 506.
- Peter RE, Schopfer A, Le Coultre B, Hoffmeyer P (1997) Fat embolism and death during prophylactic osteosynthesis of a metastatic femur using an unreamed femoral nail. Journal of orthopaedic trauma 11: 233-234.
- Ristevski B, Jenkinson RJ, Stephen DJ, Finkelstein J, Schemitsch EH, et al. (2009) Mortality and complications following stabilization of femoral metastatic lesions: a population-based study of regional variation and outcome. Canadian Journal of Surgery 52: 302.
- Shepherd LE, Shean CJ, Gelalis ID, Lee J, Carter VS (2001) Prospective randomized study of reamed versus unreamed femoral intramedullary nailing: an assessment of procedures. J Orthop Trauma 15: 28-32.
- Manning JB, Bach AW, Herman CM, Carrico CJ (1983) Fat release after femur nailing in the dog. J Trauma 23: 322-326.
- Wozasek GE, Simon P, Redl H, Schlag G (1994) Intramedullary pressure changes and fat intravasation during intramedullary nailing: an experimental study in sheep. J Trauma 36: 202-207.
- Duwelius PJ, Huckfeldt R, Mullins RJ, Shiota T, Woll TS, L, et al. (1997) The effects of femoral intramedullary reaming on pulmonary function in a sheep lung model. J Bone Joint Surg Am 79: 194-202.
- John W, Munz, Andrea L Gale, Rex AW Marco (2015) Reamer/irrigator/Aspirator (RIA) and Intramedullary Fixation for Impending Pathologic Femur Fractures. Texas Orthopaedic Journal 1: 45-52.
Citation: Raasck K, Al Farii H, Alnusif N, Wang X, Wang C, et al. (2018) The Effects of Simultaneous Versus Staged Bilateral Femoral Intramedullary Nailing for Metastatic Disease on Survival Time and Perioperative Complications: A Systematic Review. J Orthop Oncol 4: 125. DOI: 10.4172/2472-016X.1000125
Copyright: © 2018 Raasck K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3632
- [From(publication date): 0-2018 - Dec 22, 2024]
- Breakdown by view type
- HTML page views: 2981
- PDF downloads: 651