Research Article Open Access
The Effects of Noise Disturbed Sleep in Children on Cognitive Development and Long Term Health
Irene van Kamp1,2*, Kerstin Persson Waye2 and Anita Gidlöf-Gunnarsson31National Institute for Public Health and the Environment, Centre for Sustainability, Environment and Health, Netherlands
2University of Gothenburg, Department of Occupational and Environmental Medicine, Netherlands
3Örebrö University, Clinic for Occupational and Environmental Medicine, Netherlands
- *Corresponding Author:
- Irene van Kamp
National Institute for Public Health and the Environment
Centre for Sustainability, Environment and Health, Netherlands
Tel: 31629555704
E-mail: vankamp.irene@gmail.com
Received Date: December 19, 2014; Accepted Date: January 19, 2015; Published Date: January 23, 2015
Citation:Kamp IV, Waye KP, Gunnarsson AG (2015) The Effects of Noise Disturbed Sleep in Children on Cognitive Development and Long
Term Health. J Child Adolesc Behav 3:179. doi:10.4172/2375-4494.1000179
Copyright: ©2015 Irene van Kamp, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Abstract Undisturbed sleep is essential for physiological and psychological health. Children have a special need for uninterrupted sleep for growth and cognitive development. Noise is an environmental factor that affects most children, but the knowledge of how children's health, wellbeing and cognitive development are affected by noise disturbed sleep due to road traffic is very incomplete. It has been shown that although children are less likely to wake up or react with sleep cycle shifts due to nighttime exposure, they might be more likely to react with physiological effects such as blood pressure reactions and related motility during sleep. The aim of this paper is to formulate a set of hypotheses as a base for future studies into the short and long term effects of noise induced sleep deprivation on health and child development and how this effects health and wellbeing later on in life. Because the literature is still trying to understand the nature of sleep disturbance among children in general a scoping review was used to achieve this, combining conceptual issues with a description of the scarce literature on noise and sleep disturbance in children as example. Based on this a set of hypotheses was formulated. It is concluded that future studies into the health effect of environmental noise exposure in early life should address these potential hypotheses and mechanisms and pay specific attention to the mediating role of sleep related aspects, including noise in conjunction with other environmental exposures such as indoor climate and exposure to sounds and light from electronic devices.
Keywords
Sleep; Children; Noise; Cognitive development; Health
Introduction
In the recently published guideline by the WHO [1] for the burden of disease from environmental noise and elsewhere [2] it is concluded that future epidemiological noise research will need to focus on vulnerable groups; some noise exposures may be worse for particular subgroups than for others such as children, older people and lower socioeconomic groups. This conclusion supports the notion that noise effects can and should be differentiated between subgroups. In most recent reviews on noise and health, this topic has been touched upon, but evidence is still scarce and scattered. A recent review [3] identified thirty seven papers (2007-2011) pertaining to primary school children, two to preschool children and four to neonates. Four papers address effects of noise in specific patient groups such as children with autism, asthma and Attention Deficit Hyperactivity Disorder (ADHD) Health effects most frequently described in the literature are annoyance, sleep disturbance, cardiovascular disease, cognitive effects and effects on hearing. Knowledge of how cognitive and long term health effects are mediated by noise disturbed sleep is very incomplete. It is generally accepted that undisturbed sleep is essential for physiological and psychological health. Children have a special need for uninterrupted sleep for growth and cognitive development. Environmental noise is a well-known factor to disturb sleep and it can be assumed to affect most children living in urbanized areas. In addition to noise in schools and preschools, many children are exposed to potentially disturbing traffic related noise at night. One of the most serious effects of community noise is sleep disturbance [4]. In this paper we are particularly interested in the role of sleep disturbance in cognitive development and cardiovascular effects in children and the (health) effects of childhood noise exposure and sleep disturbance later on in life. The aim of this narrative review is to formulate a set of hypotheses as a base for future studies into the effects of noise induced sleep deprivation on health and child development. Although we are aware that environmental noise is only one of the causes of childhood sleep disturbance we want to draw attention to this understudied and increasing problem, while at the same time placing the issue in a broader context. After a general introduction on sleep and indicators of sleep disturbance, in adults and children existing evidence in children is described in terms of prevalence and effects moving from acute biological effects, day after effects on performance and cognition to more chronic effects of sleep disturbance on health, wellbeing and cognitive impacts later on in life. The possible mechanisms are described and a set of hypotheses is formulated.
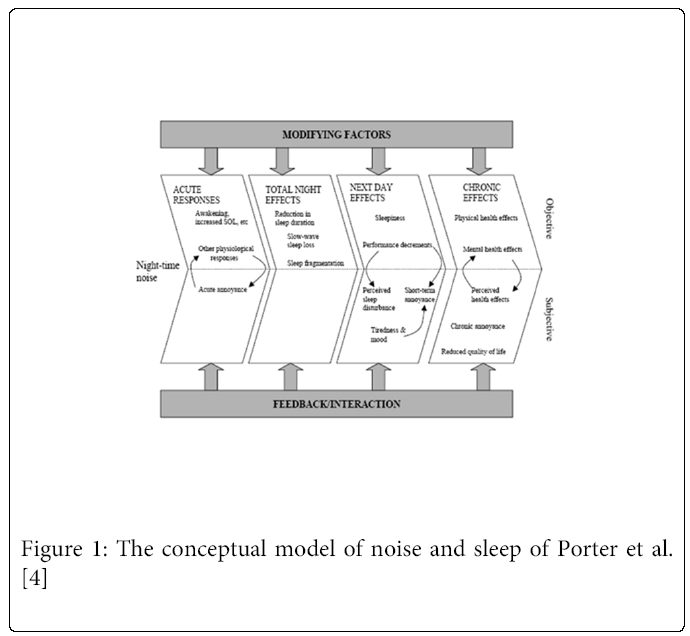
A conceptual model
It has been shown that nighttime noise can negatively affect people’s sleep. The relationship between environmental noise and different aspects of sleep, and long term health effects, is a complex one. Several researchers have presented conceptual models to describe this complex interplay [5-7]. The model described by Porter et al. [5], which is presented below, can be considered as representative for current thinking about the mechanism by which environmental noise can lead to sleep disturbance and (long term) health effects. This model shows that noise can directly lead to acute effects and then through a chain of negative consequences to long term health consequences. Feedback mechanisms and modifying factors are hereby assumed, meaning that noise can lead to health consequences through indirect pathways. This complex web of interactions makes it difficult to quantify any simple exposure-response relationship between noise exposure and health effects.
* SOL: Sleep Onset
The model distinguishes:
• acute responses that include immediate or direct disturbances caused by noise events,
• total night effects that are aggregations of (1) over the whole night,
• next day effects that are a result of (1) and (2), and
• chronic effects that are pervasive long-term consequences of (1,2) and (3).
Sleep disturbance is generally seen as an intermediate effect of noise and is assumed to be a potential initiator of diseases and/or a potential aggravator of existing disease. Whether this will happen depends on the person’s vulnerability and/or sensitivity. [8-11] Potentially vulnerable groups are people with a somatic or mental disorder, shift workers and the elderly. Although some studies have shown that children are less likely to awake or to react with a shift in sleep cycles shifts, [12,13], there are indications that children are especially respond with stronger physiological effects during sleep such as blood pressure reactions than adults. [14-17]. However, in 2004 the Dutch Health Council [18] concluded that the strength of the evidence for children’s sensitivity for acute cardiovascular effects in relation to noise disturbed sleep, is weak and even weaker for other biological responses. In general this conclusion still holds at this point in time: no additional evidence has accumulated on this since then.
Normal sleep in children
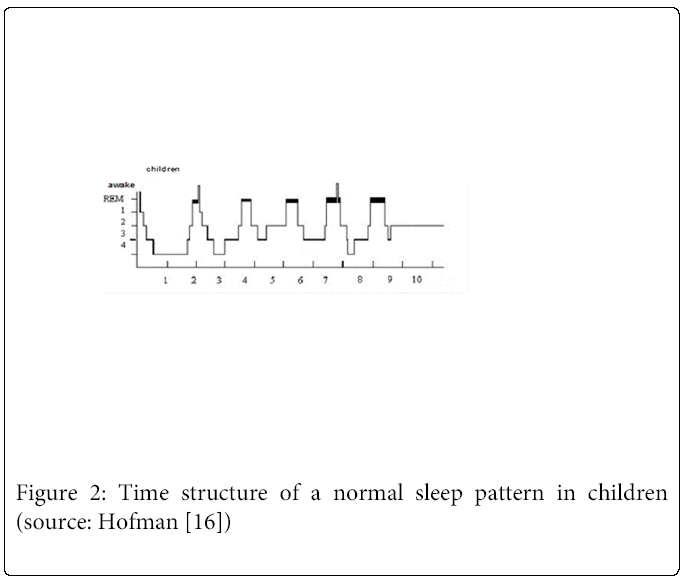
Sleep patterns can be described by ways of brain activity (electroencephalogram cq EEG), information about eye movement (electro-oculogram cq EOG) and muscle tone (electromyogram cq EMG). The sleep cycle contains two main states: rapid eye movement (REM) and non-rapid-eye movement (NREM), while NREM is subsequently separated into 3 sleep stages. [18,19]
REM sleep features a low-amplitude, mixed frequency electroencephalogram EEG, with eye movements (EOG) showing bursts of REM activity similar to that seen during eyes-open wakefulness, and absent EMG activity due to brainstem-mediated muscle atonia that is characteristic of REM sleep. NREM (including slow wave) sleep is required for the brain to recover from fatigue, while REM sleep was for a long time considered as necessary for physical recovery and essential for the maintenance of quality sleep. Today there is no consensus on the exact relative functions of the various sleep stages for mental and physical health. Slow wave N3 stage sleep is generally considered to be important for physical restoration [20-22] and memory [23], while REM sleep is also believed to be important for cognition [24]. Indicators of disturbed sleep
Indicators of disturbed sleep
Sleep disturbance is a multi-faceted concept, referring to a broad range of effects from awakening to subtle changes in autonomic physiology, and these changes are not necessarily consistent within an individual for a given level of noise stimulus as there are complex patterns of neurophysiology associated with the different EEG defined sleep stages and the time of night. Given this complex process there are various end-points that can be chosen to assess the degree of sleep disturbance These range from measures extracted from the EEG based polysomnography, which is considered the ‘gold-standard’ of sleep recording and provides a direct measure of cerebral activity from which a number of macro and microstructural features can be extracted. [15] Sleep disturbance also refers to subjective effects such as perceived quality of sleep or nighttime annoyance.
As a consequence, many different methods and techniques are used to investigate the possible effects of noise on sleep disturbance which vary widely depending on the responses/effects being studied (see the model of Porter in figure 1). These methods can roughly be divided into two categories: physiological measures and self-report measures such as diaries and questionnaires.
Table 1 gives an overview of physiological parameters, the underlying concept and their operationalization.
| Type of examination | Indicator for | What is examined? |
|---|---|---|
| Electroencephalograph (EEG)1) | The sleep stages | Total sleep time, total time spent overnight in Slow Wave Sleep(SWS; deeper sleep) and in the stage of Rapid Eye Movement (REM; dream sleep) |
| EMG1 EOG1 Electrocardiography (ECG) Plethysmography Actimetry |
Muscle tone Eye-movements Cardiac function Heart rate and blood pressure Motility |
Heart rate Total sleep time, time of falling asleep, wake-up time, Number of awakenings |
| Overnight cortisol in blood or fluvia Overnight urinary catecholamine |
Level of circulating catecholamine Level of total catecholamine released during sleep, not taken up by sympathetic nerve endings |
Sympathetic nervous activity |
Table 1: Overview of physiologic examinations used in studies investigating the possible effects of noise on sleep. (Source: van Kempen, Staatsen, and van Kamp, 2005 [25])
1The measurement of brain activity by means of EEG, EMG and EOG is also called polysomnography.
As Table 1 shows, awakenings can be measured and defined in several ways. A distinction is made between arousals (or EEG awakenings) and behavioral awakenings. An arousal is defined as an EEG response that has all the characteristics of an individual awake; behavioral awakening is confined to a verbal or motor response, indicating the subject is awake.
The quality of sleep can also be measured in a subjective way, usually as (non-acute) after effect.
Indicators used in child studies
Sleep studies in children using these different methods described above are rare and even more so are studies into the effect on sleep due to noise exposure. In 2004 a committee of the NL Health Council [18] concluded that very little is known about the biological effects on children of exposure to noise when sleeping, or about the impact on children’s health and well-being and this conclusion still holds today. Although the findings of the European research project Road traffic and Aircraft Noise exposure and children’s cognition and Health (RANCH) and the Munich study [26,27] have shed some light on the effects of noise on children as compared to their parents, there is still an overall lack of knowledge regarding the issue of childhood exposure to noise when sleeping. During a noise-disturbed night, effects might show at different stages, e.g. the sleep onset might be slightly delayed or while REM sleep might still shows clear rhythmic occurrence, some of its episodes might be fragmented. Also significant awakenings might occur throughout the sleep process and overall sleep efficiency is reduced as was shown by Muzet [14] in a hypnogram of a young adult during a noise disturbed sleep, as compared to a normal night. To our knowledge no such example is available for children. More objective measures of after effects include excretion of hormones, sleepiness, task performance tests, and cognitive functioning tests.
The quality of the sleep can also be measured in a subjective way using questionnaires on sleep quality, tiredness and annoyance. After effects (non-acute) are usually measured subjectively using questionnaires on sleep quality, tiredness, and annoyance. Subjective ´measures are rarely applied to children. One of the few exceptions is the study of Öhrström et al. [13] among 9-12 year old children, in which both the parents and children were asked to rate their overall sleep quality, frequency of movement and extent of sleepiness when waking up on an 11 point scale.
Methods
In view of the main aim of this paper to formulate a set of hypotheses regarding the short and long term effects of sleep disturbance in children, this paper combines a conceptual approach with a more narrative review method, which both build on the work we have previously performed in the field of noise and sleep disturbance in adults and children. Primarily, previous reviews on the topic have been used as a basis as well as a systematic review on the association between environmental noise and sleep disturbance performed for the EPD Hong Kong [3a] and an ICBEN review on health effects of noise in vulnerable groups [3]. More recent literature on the topic was sought making use of the major literature data bases (MEDLINE, PUBMED, SCOPUS and GOOGLE SCHOLAR). Since the current literature is still trying to understand the mechanisms and meaning of sleep disturbance in children it is still too early for a proper systematic review on this topic.
Results
Prevalence
Estimates of the prevalence of sleep disorders in children vary on average between 10% to 25% [28,29]. In a large epidemiological study in the USA based on GP registry data and using the ICD-9 sleep diagnoses, Meltzer et al. [30] found much lower figures with prevalence in the range of 3-5%. This might be indicative of underreporting by GP’s, as the authors suggest, but more likely these low prevalence rates are associated with the way sleep disturbance was defined. The GP registry data seem to only ‘catch’ the more serious and chronic forms of disturbance; milder cases of child’s sleep disturbance are not per se reported to the GP’s by the parents. Comparable rates were reported by Rona et al. [31], based on a large epidemiological study in English and Scottish children which found that 4% of the 14 372 children experienced sleep disturbances at least once a week. Important risk factors identified were socioeconomic factors associated with ethnicity and respiratory illness. In 1999 Thunström [32] found in Sweden that 16% of the parents of children aged 6 to 18 months reported moderate to severe problems with falling asleep and up to 30% frequent awakenings per night. Parental worry and anxiety were found to be the most common causes of the child’s sleeping problems. In 6% of the children severe sleep disorders as defined by the ICSD were diagnosed. A Finnish study performed in 2000 [33] among a sample of 8 to 9 year old schoolchildren estimated the prevalence of sleep problems by asking the children as well as the parents. Disturbed sleep was reported by 22% of the parents and 18% of the children. Remarkable was that these did not always overlap and adding both resulted in an estimate of 32%, concerning mild cases. In less than 0.5 % the problems were serious. It was concluded that sleep problems are often overlooked by parents and therefor parents as well as the children should be asked to provide information.
A Swedish survey at the national level [34] performed in 2005 reports that one out of seven 12-year-old children (15%) indicated themselves that noise prevented them from falling asleep. For about 25,000 schoolchildren aged 7-14 years this occurred several times a week. Approximately half of these children state that several times a week they had difficulties to sleep the whole night without waking up. There are only a few examples of studies of how children are affected by sleep due to road traffic noise [17].
Evidence for noise disturbed sleep in children
The Night Noise Guidelines of WHO [17] concluded that children with disturbed sleep present cognitive dysfunction and behavioral disturbances, abnormal growth hormone release, increase of diastolic BP and an increased risk of accidents and use of sleeping pills. These effects form a mix of acute, next day and long term outcomes and are primarily based on older studies from before 1990 in specific patient groups. Below more recent evidence on the effect on environmental noise on children’s sleep per outcome category is summarized.
Acute effects and effects over a night
The Health Council Netherlands [18] made the following distinction of effect within the category of acute effects of noise on sleep: Heart rate acceleration, a change in the quantity of a stress hormone, sleep stage changes (EEG), EEG awakening, motility and motility onset and finally behavioral awakening (self-indicated/ registered). Because of the lack of research data on children, it is not possible to say with confidence whether children are more reactive than adults to other acute biological responses.
Next day effects
A study of 9-12 year olds in the EU project RANCH showed that children’s problems with daytime sleepiness was higher with increasing road traffic noise exposure levels outside the children's home. [13] Sadeh et al. [35] found an association between poor sleep quality and worsened performance on complex cognitive tasks in school related to difficulty in sustaining attention. A sub-study [26] on aircraft noise at night in RANCH found no effect on children's reading comprehension or memory in addition to the effect of aircraft noise during daytime. However, the aircraft noise exposure during the day at school and at night at home were so strongly correlated that the variation was insufficient to test whether day time noise at school and night noise at home had independent effects.
Regarding cognitive after effects of sleep deprivation, Hygge et al. [27] (see also WHO background paper NNGL) deduced that noise in the early night, e.g. aircraft noise before midnight, could be particularly damaging to memory and related cognitive functions. Although these effects have been found in adults, this implication has not yet been explicitly tested in children. At the moment it is known that sleep affects memory, but not clear is how. New evidence primarily based on adult studies points in the direction of an increased effect on memory due to noise in the early night, but there is as yet no graded quantification about whether ordinary before-midnight noise levels around large airports are sufficient to make a difference. Further, since children's memory systems pass through developmental changes and are not structured in the same way as in adults, it would be interesting to know to what extent the results found for adults are also valid for children, and whether the depth of children's sleep counteract or enhance the slow wave sleep (SWS) dominance in the early night. An important conclusion is that studies into the cognitive effects of daytime noise levels cannot be used as a proxy for effects of night time exposure. Wilhelm et al. [36] studied the beneficial effects of sleep on retention of declarative memories and concluded that this was comparable to results in adults. Children showed smaller improvement in finger-tapping skill across retention sleep than wakefulness, indicating that sleep-dependent procedural memory consolidation depends on developmental stage. Secondary analysis of two large airport data [26] showed that nighttime aircraft noise exposure has no additional impact on reading or recognition memory beyond the effects of daytime noise exposure. It also showed no effects of nighttime noise exposure on self-rated health or overall mental health. Effects on motivation and further studies into the restorative function of sleep [37] are brought forward as important topics for future studies. Healthy normal children with fragmented sleep (measured by actigraphy) also showed lower performance on neurobehavioral functioning (NBF) measures, particularly those associated with more complex tasks, and also had higher rates of behavioral problems. [38] In normal children without sleep disorders, modest sleep restriction was found to affect children’s neurobehavioral functioning (NBF). Sadeh, Gruber and Raviv [39] monitored 77 children for 5 nights with activity monitors. On the third evening, the children were asked to extend or restrict their sleep by an hour on the following three nights. Their NBF was reassessed on the sixth day following the experimental sleep manipulation and this showed that extended sleep led to improved sleep quality and sleep restriction led to a reduction in self-reported alertness.
Also the cardiovascular first sentence is somewhat odd, Suggest:
Long term health effect of disturbed sleep
Long term health effects of disturbed sleep have been studied primarily in adults. In general we still lack evidence regarding the long term effects of instantaneous sleep-disturbances, but more recently there is evidence of increased risk for several diseases in adults. For example there is increasing evidence that chronic sleep deprivation and cardiovascular disease are associated. Non night-time dipping effect DBP as indicator of a lack of restoration has lately received more attention; in a study on a sub-sample of the EU HYENA project (N=149) a non-dipping effect of diastolic BP at night was found in the noise exposed group, which has previously been identified as independent risk factor for CVD. [41] Patients with chronic insomnia show a disturbed balance in their immune system. [42,43] Circadian disorganization in relation to sleep deprivation may also be important: changed body metabolism and potential effects on obesity showed in a study of Taheri. [44,45] An imbalance between leptin and ghrelin can lead to an increased sense of hunger with weight gain as a consequence. Obesity in its own turn is a risk factor for cardiovascular disease and diabetes, by creating a disturbance of the glucose metabolism. [46] Also the risk of diabetes due to sleep disturbance [53] and poorer cognitive performance [30,47] have been identified as accompanying long term effects of disturbed circadian rhythms.
Important finding on the relation between (noise-related) insomnia and mental health, reported in the background paper of Stansfeld for the WHO NNGL, is that insomnia more often precedes rather than follows incident cases of a mood disorders. [42] Compared to good sleepers, severe insomniacs reported more medical problems, had more physician-office visits, were hospitalized twice as often, and used more medication. Severe insomniacs had a higher rate of absenteeism, missing work twice as often as did good sleepers. They also had more problems at work including decreased concentration, difficulty performing duties, and more work-related accidents. [43] It is concluded that evidence regarding the role of noise exposure, sleep and the development of depression, is still scarce.
Studies on long term health effects due to noise disturbed children are practically rare. It has been put forward that an elevated BP during childhood might be a good predictor of hypertension later on in life. [40] However, secondary analysis of two large airport data on the health effects of noise in children (aged 9-11) [26] showed that nighttime aircraft noise exposure had no additional impact on selfrated health or overall mental health in schoolchildren. Longitudinal studies are urgently needed in order to evaluate long term consequences of a disturbed sleep.
Cardiovascular effects of noise and the role of sleep disturbance
Only a few epidemiological studies exist long term nocturnal noise exposure affects cardiovascular health/outcomes. An exception is a study of Maschke et al. [48], the results of which suggested slightly higher effect estimates (odds ratio 1.9 vs. 1.5) for the prevalence of hypertension in adults with respect to the noise exposure of the bedroom (during the night) compared with the exposure of the living room (during the day). Critique on these findings is directed at the composition of the sample (older and health conscious group). There is some new evidence that the association between annoyance and CVD outcomes is stronger for sleep related annoyance/disturbance. [40,49,50] Sleeping behavior such as closing windows, moving to another room are assumed to play a mediating role in this association.
As for children, analysis on the pooled data set (Heathrow, Schiphol) of the RANCH study [51] indicated that aircraft noise exposure at school was related to a statistically non-significant increase in BP and heart rate in children. Road traffic noise showed an unexplained negative effect. Significant associations with night-time exposure were found and based on this it is concluded that blood pressure elevations might also be seen as an effect of sleep disturbance. [49] Babisch and van Kamp [52] and a later review of studies within the UK [53] concluded that there was an inconsistent association between aircraft noise and children’s BP primarily due to methodological differences between studied. In their recent review, Paunovic et al. [54] concluded a tendency towards positive associations, but they also observed large methodological differences between studies. A study among children aged 8-14 years by Babisch et al. [55] concluded that road traffic noise at home as a stressor could affect children’s BP.
There is some evidence that short-term cardiovascular reactions during sleep are more pronounced in children. [25,56] Lepore et al [56] concluded that compared with quiet-school children, noisyschool children had significantly lower increases in BP when exposed to either acute noise or non-noise stressors, indicative of a generalized habituation effect. Studies in Serbia [57,58] among schoolchildren and pre-school children indicated a raised BP among children from noisy schools who live in quiet residences compared with children from quiet school and quiet home environments indicating that the effects due to daytime noise exposures while at school were not compensated for by quiet periods while at home .
Discussion
This scoping review has shown that studies into the short and long term effects of noise disturbed sleep in children on health and cognition are scarce. This is expected to change in the near future. In the context of continuing urbanization noise exposure will increase in the coming decades also for young children. Due to the 24 hour economy noise exposure starts earlier and ends later in the day and will continue over the weekend. Since sleep patterns change with age these developments might primarily affect young children and noise policies have to account for these differences in their noise regulations. For example: only in children the deep sleep stage is observed in the later parts of the nights and current curfews around airports do not take this into account. These developments include that not only the moments and places of quiet and restoration are diminishing, but also that sleep disturbance in children might be an increasing problem. In particular the combination with other environmental stressors such as frequent use of computer screens, which has been shown to affect sleep duration as well as sleep quality, will be of concern. New developments in the field of genomics and gene- environment [64] interactions will allow for studying the effects of early childhood exposures later on in life and sleep disturbance is identified as a potentially important mediator in this process. There are new but still highly theoretical notions on early gene-environment interactions [59] which suggest that lifespan exposure to stress influences brain structures involved in cognition and mental health. This sheds new light on the importance of developmental sensitive periods.
In line with the Health Council Netherlands [18] in reviewing the results a distinction was made between acute effects, next day effects, after effects and long term effects. There is insufficient evidence to know whether children are more responsive than adults to other acute biological responses than those found for adults. Studies into the next day or after effects have shown that exposure to increased transport related noise levels were associated with daytime sleepiness and performance on complex tests and problems with sustaining attention. [62] After effects on cognition and performance have been studied in adults only and for adults early night exposure, e.g. aircraft noise before midnight, was shown to be particularly damaging to memory and related cognitive functions [27]. However it is not clear whether these findings apply to children in the same way. It would be interesting to know to what extent the results found for adults are also valid for children, and whether the depth of children's sleep counteract or enhance the slow wave sleep (N3) dominance in the early night.
A more recent study [63] indicated that nighttime noise was found in particular to be associated with more emotional symptoms. This association may be confounded by the presence of sleeping problems and the authors recommend that more longitudinal studies are required to explore the temporal sequence of noise exposure, sleep disturbances and behavioral problems.
Effects on motivation and further studies into the restorative function of sleep have also been brought forward in the literature as important topics for future studies. Regarding the long term health effects of sleep disturbance it has been put forward that an elevated BP during childhood might be a good predictor of hypertension later on in life. The non-dipping effect of diastolic BP at night was found in noise exposed groups, which has previously been identified as independent risk factor for CVD. How this effect is related to early childhood exposure should be studied in more depth.
Several mechanisms were described to explain the association between sleep disturbance and obesity as well as diabetes type 2. Circadian disorganization in relation to sleep deprivation is one of them. An imbalance between leptin and ghrelin can lead to an increased sense of hunger with weight gain as a consequence. [46,64] The risk of diabetes due to sleep disturbance and poorer cognitive performance have been identified as accompanying long term effects of disturbed circadian rhythms. The hypothesis that childhood noise related sleep disturbance could lead to more serious sleep disturbance and insomnia later on in life is mentioned in the literature, but would need much more attention in prospective cohort studies. Potential mechanisms brought forward in relation to the effect of sleep disturbance and cognitive effects were extensively described by Stansfeld at al. [26] Evidence is still lacking, but narrowing of the attention focus, impairments of auditory discrimination and speech perception, and communication difficulties in the classroom and learned helplessness were brought forward as plausible candidates. It is not clear yet if and how noise-related behavior in the long term has a negative influence on children's health and learning.
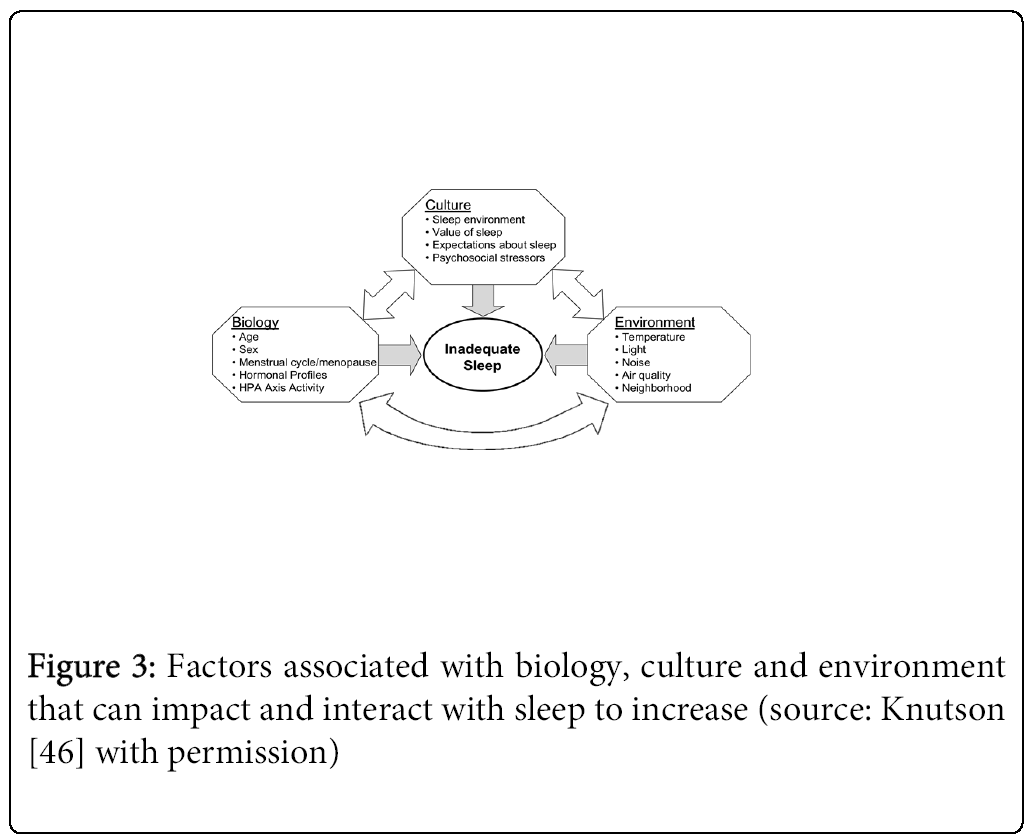
Future studies into the mechanisms behind the issue of noise and sleep in children should be placed in a broader environmental and cultural context as was canvassed by Knutson [46] in her model presenting the environmental factors that can impair sleep in conjunction with biological and cultural factors.
It is known from previous studies that sleep could be disturbed when the ambient temperature is too hot, too humid or too cold. [60] Another factor of influence is light, either caused by natural light (Northern hemisphere) or artificial sources in the bedroom due to street lamps, greenhouses, indoor lighting or daytime sleep. One mechanism through which exposure to light at night can impair sleep is the inhibition of melatonin. Transport related pollutions which are common characteristics of large urban areas according to the model are noise that can impair sleep via physiological arousal as measured by (motility, EEG awakenings, BP changes and heart rate variability) and air pollution both indoor and outdoor via breathing. Recently it was shown [65] that bruxism during sleep was more prevalent in children exposed to light and noise.
Lastly, the model mentions neighborhood characteristics which primarily refer to social safety. Studies addressing the joint effect of environmental and neighborhood aspects on sleep quality are rare but can be considered as important in particular to understand the disparities in sleep between different populations [46].
Conclusion
Effects of noise disturbed sleep in children is an understudied topic, while due to the 24 economy and ongoing process of urbanization nighttime noise exposure is expected to pose an increasing problem. Evidence on acute and long term effects of childhood sleep disturbance is still scarce. In specific more information is needed on long term health effects and long term impacts on cognitive development of disturbed sleep in early childhood. A more integrated approach is needed to further the field including experimental as well as epidemiological studies such as prospective cohort studies
This study was made possible with a grant from the Swedish Research Council for Health, Working life and Welfare (FORTE) Guest researcher program 2011-1446.
References
- WHO (2011) Burden of disease from environmental noise. Quantification of healthy life years lost in Europe. Copenhagen: WHO Regional Office for Europe.
- Basner, M Griefahn, B, van den Berg, M. (2010) Aircraft noise effects on sleep: mechanisms, mitigation and research needs. Noise Health 12: 95-109.
- Van Kamp I, Davies H (2013) Noise and health in vulnerable groups: a review. Noise Health 15: 153-159.(3a). van Kamp I, Lam KC, Brown AL, Wong TW, Law CW (2012) Sleep-disturbance and quality of sleep in relation to night time noise exposure. J AcoustSoc Am 131:3222.
- Griefahn B (2002) Sleep Disturbances Related to Environmental Noise. Noise Health 4: 57-60.
- Porter ND, Kershaw AD, Ollerhead JB (2000) Adverse effects of Night-time aircraft noise. CAA ERCD Report 9964.
- Ising H, Babisch W, Kruppa B (1999) Noise-Induced Endocrine Effects and Cardiovascular Risk. Noise Health 1: 37-48.
- Passchier-Vermeer W (2003) Night-time noise events and awakening TNO, INRO.
- Cohen S, Evans GW, Stokols D, Krantz DS (1986) Behavior health and environmental stress. N.Y: Plenum Press.
- Berglund B, Lindvall T, Schwela DH (1999) Guidelines for community noise. World Health Organisation.
- Van Kamp, I, Job JR, Hatfield, J et al. (2004) The role of noise sensitivity in the noise-response relation: A comparison of three international airport studies .Acoustical Society of America Journal 116: 3471-3479.
- Staatsen BAM, Nijland HA, Kempen EMM van, Hollander AEM de, Franssen AEM, et al. (2004) Assessment of health impacts and policy options in relation to transport-related noise exposures. Topic paper noise. Bilthoven: RIVM.
- Eberhardt JE (1990) The disturbances by road traffic noise of the sleep of prepuberal children as studies at home in Berglund and Lindvall, Proceedings ICBEN, Stockholm, 65-79.
- Öhrström E, Hadzibajramovic E, Holmes M (2006) Effects of road traffic noise on sleep - studies on children and adults. J Environ Psychol 26: 116-126.
- Muzet A (2007) Environmental noise, sleep and health. Sleep Med Rev 11: 135-142.
- Hume KI (2008) Research over the last and next five years. Proccedings ICBEN.
- Hofman WF (2013) Geluid en Gezondheid. (Noise and Health)In Dutch.
- WHO (2009) Night noise guidelines (NNGL) for Europe EU centre for environment and health Bonn Office Grant Agreement 2003309 between the European Commission, DG Sanco and the World Health Organization. Copenhagen: WHO Regional Office for Europe.
- Health Council of the Netherlands (2004). The Influence of Night-time Noise on Sleep and Health. The Hague: Health Council of the Netherlands.
- Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, et al. (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8: 597-619.
- Bonnet MH (1985) Effect of sleep disruption on sleep, performance, and mood. Sleep 8: 11-19.
- Borbély AA (1982) A two process model of sleep regulation. Hum Neurobiol 1: 195-204.
- Young JS, Bourgeois JA, Hilty DM, Hardin KA (2008) Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med 3: 473-482.
- Diekelmann S, Wilhelm I, Born J (2009) The whats and whens of sleep-dependent memory consolidation. Sleep Med Rev 13: 309-321.
- Walker MP, Liston C, Hobson JA, Stickgold R (2002) Cognitive flexibility across the sleep-wake cycle: REM-sleep enhancement of anagram problem solving. Brain Res Cogn Brain Res 14: 317-324.
- Kempen, E van, Staatsen, BAM, Kamp, drop et al. (2005) Selection and evaluation of exposure response relationships for HIA in the field of noise and health RIVM report 630400001/2005.
- Stansfeld S, Hygge S, Clark C, Alfred T (2010) Night time aircraft noise exposure and children's cognitive performance. Noise Health 12: 255-262.
- Hygge S, Evans GW, Bullinger M (2002) A prospective study of some effects of aircraft noise on cognitive performance in schoolchildren. PsycholSci 13: 469-474.
- van Litsenburg RR, Waumans RC, van den Berg G, Gemke RJ (2010) Sleep habits and sleep disturbances in Dutch children: a population-based study. Eur J Pediatr 169: 1009-1015.
- Liu X, Zhao Z, Jia C, Buysse DJ (2008) Sleep patterns and problems among chinese adolescents. Pediatrics 121: 1165-1173.
- Meltzer LJ, Johnson C, Crosette J, Ramos M, Mindell JA (2010) Prevalence of diagnosed sleep disorders in pediatric primary care practices. Pediatrics 125: 1410-1418.
- Rona RJ, Li L, Gulliford MC, Chinn S (1998) Disturbed sleep: effects of sociocultural factors and illness. Arch Dis Child 78: 20-25.
- Thunström M (1999) Severe sleep problems among infants in a normal population in Sweden: prevalence, severity and correlates. ActaPaediatr 88: 1356-1363.
- Paavonen EJ, Aronen ET, Moilanen I, Piha J, Räsänen E, et al. (2000) Sleep problems of school-aged children: a complementary view. ActaPaediatr 89: 223-228.
- Miljöhälsorapport (2005)Stockholm: Socialstyrelsen.
- Sadeh A, Gruber R, Raviv A (2002) Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Dev 73: 405-417.
- Wilhelm I, Diekelmann S, Born J (2008) Sleep in children improves memory performance on declarative but not procedural tasks. Learn Mem 15: 373-377.
- Hartig,T, Evans GW, Jamner LD et al? (2003) Tracking restoration in natural and urban field settings. Journal of Environmental Psychology 23: 109–123.
- Bistrup ML, Babisch W, Stansfeld S, Sulkowski W (2006) PINCHE's policy recommendations on noise: how to prevent noise from adversely affecting children. ActaPaediatrSuppl 95: 31-35.
- Sadeh A, Gruber R, Raviv A (2003) The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev 74: 444-455.
- Babisch W (2006) Transportation noise and cardiovascular risk. Review and synthesis of epidemiological studies. Dose-effect curve and risk estimation. Federal Environmental Agency.
- Haralabidis AS, Dimakopoulou K, Vigna-Taglianti F, Giampaolo M, Borgini A, et al (2008) Acute effects of night-time noise exposure on blood pressure in populations living near airports. Eur Heart J 29: 658-664.
- Ohayon MM, Roth T (2003) Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res 37: 9-15.
- Léger D, Guilleminault C, Bader G, Lévy E, Paillard M (2002) Medical and socio-professional impact of insomnia. Sleep 25: 625-629.
- Taheri S, Lin L, Austin D, Young T, Mignot E (2004) Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 1: e62.
- Taheri S (2007) Sleep and metabolism: bringing pieces of the jigsaw together. Sleep Med Rev 11: 159-162.
- Knutson KL, Spiegel K, Penev P, Van Cauter E (2007) The metabolic consequences of sleep deprivation. Sleep Med Rev 11: 163-178.
- Donga E (2010) A Single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. Journal of Clinical Endocrinology & Metabolism 95:2963-2968.
- Maschke C, Wolf U, Leitmann T (2003) EpidemiologischeUntersuchungenzumEinfluss von Lärmstress auf das Immunsystem und die Entstehung von Arteriosklerose. WaBoLu-HefteUmweltbundesamt, Berlin.
- Maschke C, Hecht K, Wolf U (2004) Nocturnal awakenings due to aircraft noise. Do wake-up reactions begin at sound level 60 dB (A)? Noise Health 6: 21-33.
- Maschke C, Hecht K (2005) [Noise induced annoyance and morbidity. Results from the pan European LARES-survey]. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 48: 315-328.
- van Kempen E, van Kamp I, Fischer P, Davies H, Houthuijs D, et al (2006) Noise exposure and children's blood pressure and heart rate: the RANCH project. Occup Environ Med 63: 632-639.
- Babisch W, van Kamp I (2009) Exposure-response relationship of the association between aircraft noise and the risk of hypertension. Noise Health 11: 161-168.
- Stansfeld S, Crombie R (2011) Cardiovascular effects of environmental noise: research in the United Kingdom. Noise Health 13: 229-233.
- PaunovicK, Belojevic G(2011) Epidemiological studies on noise and blood pressure in children: Observations and suggestions. Environ Int 37: 1030-1041.
- Babisch W, Neuhauser H, Thamm M, Seiwert M (2009) Blood pressure of 8-14 year old children in relation to traffic noise at home--results of the German Environmental Survey for Children (GerES IV). Sci Total Environ 407: 5839-5843.
- Lepore SJ, Shejwal B, Kim BH, Evans GW (2010) Associations between chronic community noise exposure and blood pressure at rest and during acute noise and non-noise stressors among urban school children in India. Int J Environ Res Public Health 7:3457-3466.
- Belojevic G, Jakovljevic B, Stojanov V, Paunovic K, Ilic J (2008) Urban road-traffic noise and blood pressure and heart rate in preschool children. Environ Int 34: 226-231.
- Belojevic G, Paunovic K, Jakovljevic B, Stojanov V, Ilic J, et al (2011) Cardiovascular effects of environmental noise: research in Serbia. Noise Health 13: 217-220.
- Lupien SJ, McEwen BS, Gunnar MR, Heim C (2009) Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci 10: 434-445.
- Kräuchi K, Gasio PF, Vollenweider S, Von Arb M, Dubler B, et al (2008) Cold extremities and difficulties initiating sleep: evidence of co-morbidity from a random sample of a Swiss urban population. J Sleep Res 17: 420-426.
- Cain N, Gradisar M (2010) Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med 11: 735-742.
- Carskadon MA (2004) Sleep difficulties in young people. Arch PediatrAdolesc Med 158: 597-598.
- Tiesler CM, Birk M, Thiering E, Kohlböck G, KoletzkoS,et al (2013) Study Groups Exposure to road traffic noise and children's behavioural problems and sleep disturbance: results from the GINIplus and LISAplus studies. Environ Res123:1-8.
- Hart CN, Carskadon MA, Considine RV, Fava JL, Lawton J, et al (2013) Changes in children's sleep duration on food intake, weight, and leptin Pediatrics 132: 1473-1480.
- Initial Serra-Negra J M, Ramos-Jorge ML, Flores-Mendoza CE et al (2014) Environmental factors, sleep duration, and sleep bruxism in Brazilian schoolchildren: a case-control study. Sleep Medicine e 15: 236–239.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 23092
- [From(publication date):
February-2015 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 18191
- PDF downloads : 4901