The Effects of Cervical and Thoracolumbar Thrust Manipulation on Shoulder Range of Motion in Patients with Rotator Cuff Related Shoulder Pain
Received: 02-Feb-2022 / Manuscript No. jnp-22-52356 / Editor assigned: 04-Feb-2022 / PreQC No. jnp-22-52356 (PQ) / Reviewed: 18-Feb-2022 / QC No. jnp-22-52356 / Revised: 24-Feb-2022 / Manuscript No. jnp-22-52356 (R) / Accepted Date: 02-Mar-2022 / Published Date: 03-Mar-2022 DOI: 10.4172/ 2165-7025.1000505
Abstract
Background and Purpose: Thrust manipulation (TM) to the cervical and thoracic spines have been investigated in Rotator Cuff Related Shoulder Pain (RCRSP), however the effects on clinical range of motion has not been quantified. The purpose of this study was to investigate the immediate and medium-term effects of cervical and thoracolumbar TM on shoulder flexion range of motion (ROM).
Methods: Twenty subjects with RCRSP were recruited via convenience sample and randomly allocated to receive either a C6-C7 or T12-L1 TM. Outcome measures of pain intensity and two shoulder flexion ROM values were assessed before treatment, immediately post-treatment and 2 weeks after treatment.
Results: Statistically significant increase in shoulder ROM with cervical TM (3.75 cm; p<.01) and thoracolumbar TM (7.25 cm; p<.01) were demonstrated immediate post-treatment. No significant differences were noted at two-week follow-up.
Discussion/Conclusion: Cervical and thoracolumbar TM demonstrated within session immediate increased shoulder ROM in RCRSP patients. Potential mechanisms for this change include reduction of muscle tone through alteration of Golgi Tendon Organ and muscle spindle activity via stretch-reflex response or descending pain inhibition. Clinicians may consider cervical or thoracolumbar TM to improve immediate shoulder flexion ROM.
Keywords
Thrust Manipulation; Rotator Cuff Related Shoulder Pain; Manual Therapy; Shoulder ROM
Introduction
Shoulder pain is a frequent complaint in the general population with a lifetime frequency of up to 70%. The prognosis is variable, with many patients reporting persistent pain between 6 and 12 months after primary care consultation [1]. The term Rotator cuff related shoulder pain (RCRSP) has been proposed to include a variety of pathologies including rotator cuff partial tear and full-thickness tear, rotator cuff tendinopathy, tendinitis, tendinosis, impingement and subacromial pain [2]. This broad term accounts for 50-85% of shoulder pain diagnoses. There is ongoing debate as to the etiology of RCRSP, the mechanisms that produce the sensation of pain, the role of inflammation, and the relationship between symptoms of structural changes in the rotator cuff tendons [2]. Due to the complex nature of the condition several factors may contribute to the development of RCRPS including muscle length, posture, anatomical acromion variations, capsular restrictions, aberrant scapular muscle activity, decreased thoracic extension, maladaptation to tendon loading and lifestyle [2-4].
Mal-adaptive and excessive loads imposed on shoulder tissues still appear to influence pain behavior in RCRPS2. There have been several studies that have emphasized the biomechanical influences on RCRSP including manual therapy techniques and progressive exercise therapy that have shown improvements in pain and shoulder function [5-7]. However, there has been conflicting literature on the effectiveness of spinal manipulation as part of a treatment plan to reduce pain and improve range of motion (ROM) in patients with RCRSP [8-10].
Several investigations [8, 9] have examined the effect of cervical, upper thoracic, and rib thrust manipulation (TM) on shoulder function and pain with various levels of effectiveness [11-13]. Some investigations have demonstrated positive outcomes including improved Shoulder Pain and Disability Index (SPADI) scores, [11] less pain with resisted and provocative testing immediately and 48 hours after TM, [11] increased shoulder ROM, [12] and reduced shoulder pain [12]. Other investigations demonstrated no significant improvement in pain or disability [8,10], no change in scapulothoracic mechanics with arm elevation after TM [10], and no change in peak force for scapulothoracic muscles [9,10]. Only one of these studies reported changes in shoulder ROM [12] and none examined the specific effect that TM may have on muscle length. Furthermore, each included multiple thrust manipulations within the same treatment session rather than assessing the response to a single TM.
There have been several studies that have investigated the effects of manipulation of the cervical or thoracic spine on posture, aberrant scapular muscle activity, and pain. Boyles [11] found that participants with Subacromial Impingement syndrome (SAIS) showed improved Shoulder Pain and Disability Index (SPADI) scores and less pain with resisted and provocative testing immediately and 48 hours after manipulation of the cervicothoracic junction and mid-thoracic spine.
Kardouni [9] investigated the effect of six manipulations on thoracic and scapular mechanics and showed no change in scapulothoracic mechanics with elevation after a thoracic manipulation. Lastly, Strunce [12] examined the effects of thoracic and rib manipulation on shoulder pain and ROM and showed an increase in shoulder ROM between 30- 38 degrees as well as a 51% reduction in shoulder pain. To date, there have been no studies to examine the effects of manipulation on muscle length.
One of the muscles that affects the kinematics of shoulder elevation is the latissimus dorsi (LD). Shoulder elevation requires an optimal length of the LD to allow for full external rotation of the humerus and scapular upward rotation [14]. Adequate scapulohumeral rhythm maintains the necessary sub-acromial space to reduce placing excessive stress on the subacromial structures such as the subacromial bursa and rotator cuff tendons [15, 16]. Stiffness of the LD has been shown to impact the kinematics of shoulder elevation and potentially lead to the development of shoulder pain or RCRSP [15, 16].
TM to a spinal segment has demonstrated transient reflexic contractions of local muscles using electromyography (EMG) in both asymptomatic and symptomatic subjects [17, 18]. Keller and Colloca (2000) demonstrated an immediate increase in muscle strength of the erector spinae after lumbar TM [19]. Wang and Meadows (2010) showed a similar transient effect in external rotation strength following graded mobilizations to the cervical spine [20]. Dunning and Rushton (2007) showed an immediate increase in EMG activity of the biceps following TM to the C5-C6 segment [17]. However, an immediate reduction in paraspinal muscle activity as measured by EMG has been shown in asymptomatic and symptomatic participants with lower back pain following a lumbar TM [21]. It has been proposed that the neurophysiologic response following TM involves activation of mechanoreceptors in the joints, ligaments, or intervertebral disc as well as the muscle spindles and golgi tendon organs of the associated muscle [22].
The LD is innervated by the thoracodorsal nerve (C6-C8), a facilitation of this spinal segment could lead to increased muscle tone and reduced shoulder ROM contributing to RCRSP [23-27]. The LD is also segmentally innervated by the dorsal primary rami through its fascial connections of the thoracolumbar fascia (TLF) [28]. Furthermore, rat studies have indicated that while 6 to 14% of neurons at the spinal segments between T12-L2 contained nociceptive input from the TLF, no nociceptive fibers were present between L3-L5 [29].
Schelip reported the TLF had the contractile ability to alter motoneural coordination secondary to its structure containing Golgi tendon organs, muscle spindles, Pacini corpuscles, and Ruffini endings [30]. TM to the cervical and thoracic spines have been investigated in Rotator Cuff Related Shoulder Pain (RCRSP), however the effects on clinical range of motion not been quantified. The purpose of this study was to compare the immediate and medium-term effects of lower cervical versus thoracolumbar TM on shoulder ROM in individuals with RCRPS.
Methods
Participants: 20 participants (table 1) with RCRSP were recruited from physical therapy clinics and bulletin board postings in local universities. The inclusion criteria were pain duration of 6 weeks or longer, pain intensity in the shoulder region of 2/10 or greater on an 11-point pain rating scale (NPRS), and age 18-60 years. In addition, 3 out of 5 special tests for RCRSP (Hawkins-Kennedy, Neer, Empty Can, pain or weakness with resisted shoulder external rotation with arm at 0 degrees abduction, and a painful arc were required to be positive [31,32].
Exclusion criteria included a history of shoulder, cervical, or thoracic surgery; primary complaints of neck pain; signs of central nervous system involvement; signs of cervical nerve root involvement; contraindications for manipulative therapy (included, but not limited to osteoporosis, systemic arthritis, or metastatic disease); primary diagnosis of adhesive capsulitis; or reproduction of shoulder or arm pain with cervical rotation, axial compression, or Spurling test [9] (Table 1).
| Parameters | Cervical TM | Thoracolumbar TM |
|---|---|---|
| Age, y | 32.20 ± 5.80 | 28.90 ± 5.32 |
| Gender | 7 Male, 3 Female | 5 Male, 5 Female |
| Symptom duration, m | 7.30 ± 2.11 | 6.20 ± 2.64 |
| BMI | 25.97 ± 2.61 | 24.24 ± 2.71 |
Table 1: Subject characteristics.
Procedures: All subjects were provided with verbal and written explanations of study procedures and signed an informed-consent form prior to participation. Testing and treatment occurred in a research lab in the Department of Physical Therapy at Texas Woman’s University. The Texas Woman’s University Institutional Review Board approved the study protocol. Participants completed an intake questionnaire consisting of medical screening questions, demographics, and symptom history including aggravating and relieving factors, history of surgeries, location and duration of symptoms, and the nature of symptoms. They also completed a baseline Numeric Pain Rating Scale (NPRS) for their current pain level. The NPRS is an 11-point Likert-scale ranging from 0 to 10 with 0 representing “no pain at all,” and 10 representing “the worst pain imaginable” which has shown good reliability in patients with shoulder pain [33].
Following testing for RCRSP, baseline shoulder ROM was completed using two different techniques. Each technique was done three times and the average was recorded.
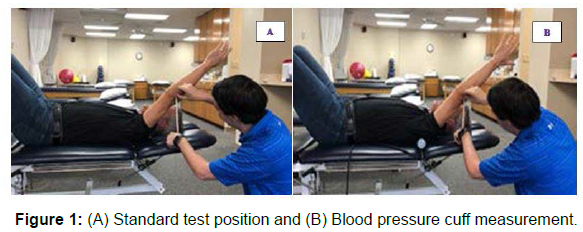
The first technique was conducted as described by Kendall using a tape measure [34]. The participant was instructed to lie in the hook lying position and flex their shoulder through full pain-free available ROM, keeping the arm close to their head. The examiner ensured that the elbow remained extended, the shoulder externally rotated, and lumbar spine remained flat against support surface by instructing the subject to flatten their back (perform a posterior pelvic tilt). Using a tape measure, the distance in centimeters was measured between the lateral epicondyle of humerus and the support surface. This measure was only taken once. This technique has shown good reliability (к = 0.69 to 0.81, ICC = .91-.93) [35, 36].
In the second technique a standard blood pressure cuff was placed beneath the lumbar spine and inflated to 60mmHg. The examiner then instructed the subject to flex their shoulder, as before ensuring that the blood pressure cuff remained at 60mmHg so the lumbar spine remained flat. We measured the distance from the lateral epicondyle to the support surface (Figure 1). Although reliability of this technique has not been assessed to our knowledge, specifically the use of a cuff, it does have clinical utility.
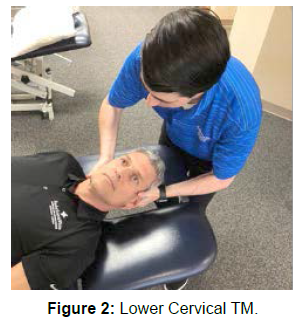
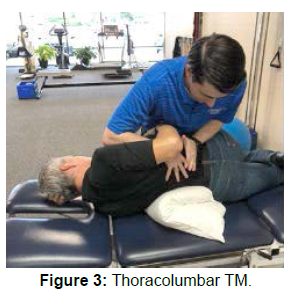
After baseline testing, subjects were randomly assigned to receive either a lower cervical or thoracolumbar TM. The tester randomly drew a number from 1-20 without replacing it. If an even number was drawn, then the participant was assigned to receive a lower cervical TM. If an odd number was drawn, then the participant was assigned to receive a thoracolumbar junction TM. The lower cervical spine (C6- T2) or thoracolumbar junction (T11-L2) was assessed to identify the most hypomobile segment. The intervertebral motion of the lower cervical spine was assessed using lateral glides [37]. The thoracolumbar junction was assessed using passive physiological intervertebral motion to determine the hypomobile segment, followed by a passive accessory intervertebral motion to establish the end feel. These techniques have been previously described by Maitland et al [38]. Following the assessment, a TM targeted either the C6-C7 segment or T12-L1, as described by Pettman (Figure 2, 3) [39, 40, 41]. The target segment was reassessed and if it was identified as hypomobile then a second TM was attempted at the same level. In four cases, a second TM was delivered, and the target segment was identified as normal upon reassessment. The technique was performed by two licensed physical therapists with orthopedic specialist certifications, which were certified orthopedic manipulative therapists with at least five years of experience and fellowship training in manual therapy. Immediately following and at a two-week follow up, the two shoulder measurements were repeated. During the two-week period between measurements, the participants were instructed to continue their daily lifestyle and exercise routine. This routine was variable between participants and was selfadministered without guidance from the examiners. The participants were instructed to avoid exercises that reproduced shoulder pain and refrain from receiving any manipulative therapy (Figure 1A and 1B, Figures 2 and 3).
Results
Twenty subjects with primary complaints of shoulder pain included 12 men and 8 females ranged in age from 23 to 50, with a mean age of 30.6 (SD = 3.43) years. Symptom duration ranged from 1 to 12 months with a mean duration of 6.75 (SD = 1.66) months.
Statistical significance was set at p = 0.05. Paired t-tests were performed to detect any differences between baseline and posttreatment shoulder ROM immediately and at 2-week follow up. An independent t-test was performed to detect any differences between groups immediately and at 2-week follow up.
Statistical (p<.01) and minimal detectable change (MDC) (change score >4cm) were demonstrated in pre and post-treatment using the standard measurement immediately for the thoracolumbar (TL) and lower cervical (LC) TM groups [36]. Shoulder ROM improved by 7.25cm in the TL group and by 3.75cm in the LC manipulative group (p<.01). There were no statistical differences at two-week follow up (Table 2).
Statistical and minimal detectable changes were also demonstrated in pre and post treatment using the blood pressure cuff measurement immediately for the TL TM groups. Shoulder ROM improved7.22cm in the TLJ group and 3.60cm in the C6-C7 group (p<.01). There were no statistical differences at two-week follow up (Table 3).
An independent t-test was run to compare the changes for the lower cervical TM and TL groups. A statistically significant difference was found when using the standard measurement and blood pressure cuff measurement (Table 4). There were no reported adverse effects following treatment with TL or lower cervical TM. No participant reported a worsening of symptoms with an increase in NPRS or decreased ROM following manipulative treatment.
Intraclass Correlations (ICC) was run to compare the techniques. The two techniques showed excellent agreement (Table 2-5).
| Technique | Pre-treatment | Post-Treatment | Change Score | P-value | Two-Week Follow up | Change Score | P-value |
|---|---|---|---|---|---|---|---|
| TLJ Manipulation | 21.55cm (SD = 4.6) |
14.30cm (SD = 3.11) |
7.25cm | < .01* | 20.08cm (SD = 4.10) |
0.75cm | 0.11 |
| LC Manipulation | 20.55cm (SD = 6.26) |
16.80cm (SD = 7.03) |
3.75cm | < .01* | 19.70 cm (SD = 4.72) |
0.85cm | 0.34 |
| *Statistically significant difference using paired t-test (P=0.05) | |||||||
Table 2: Pre-treatment and post-treatment immediate and 2-week follow up analysis of Latissimus dorsi muscle length.
| Technique | Pre-treatment | Post-Treatment | Change Score | P-value | Two-Week Follow up | Change Score | P-value |
|---|---|---|---|---|---|---|---|
| TLJ with BP Cuff | 21.78cm (SD = 4.45) |
14.56 cm (SD = 3.35) |
7.22cm | < .01* | 21.10cm (SD = 3.45) |
.68cm | 0.25 |
| LC with BP Cuff | 20.30cm (SD = 6.22) |
16.70cm (SD = 6.71) |
3.60cm | < .01* | 19.52cm (SD = 4.86) |
.78cm | 0.31 |
| *Statistically significant difference using paired t-test (P=0.05) | |||||||
Table 3: Analysis of change in shoulder clinical ROM in the TLJ and LC manipulation.
| Technique | Immediately | Two-week |
|---|---|---|
| p-value | p-value | |
| Without BP cuff | 0.024* | 0.906 |
| With BP Cuff | 0.024* | 0.909 |
| *Statistically significant difference using independent t-test (P=0.05) | ||
Table 4: Analysis of change in shoulder clinical ROM in the TLJ and LC manipulation.
| Measurement | Correlation of Two Techniques of LD Muscle Length |
|---|---|
| Cervical Pre-Intervention | 0.99 |
| Cervical Post-intervention | 0.99 |
| Cervical 2-week follow-up | 0.97 |
| TLJ Pre-Intervention | 0.98 |
| TLJ Post-intervention | 0.98 |
| TLJ 2-week follow-up | 0.97 |
Table 5: Correlation of two techniques of LD muscle length.
Discussion
Several studies have examined the effect of TM on shoulder function and pain, most often using a biomechanical regional interdependence model [8, 9, 11, 12], with varying results. Most of these studies have chosen TM purported to improve spinal or rib mobility, improve thoracic or cervical spine joint mechanics, and prevent or decrease RCRSP. These studies used cervical, upper thoracic, and rib TM with various levels of effectiveness [8, 9, 11, 12].
This study assessed the effect of two different TM attempting to target the segmental innervation of the LD. The direct segmental motor innervation of LD is C6-8 via the thoracodorsal nerve. However, the LD also has a secondary sensory innervation through its attachment to the TFL. According to Willard the fascial attachments of the TLF to the LD are segmentally innervated by the dorsal rami of the spinal cord [28]. As such a TM directed at one of these segments may cause an effect on the LD and lead to the improved ROM observed. In addition to a neurophysiological effect from a TM performed on a structure remote from the shoulder, there is possibly a direct segmental effect due to the unique anatomy of the TLF and its attachment to the LD. Although no direct cause-and-effect relationship may be determined, our data suggests that statistically significant changes in shoulder ROM (consistent with LD length) occur immediately following both LC and TL TM, with a significant difference favoring the TL TM. If segmental innervation were the only aspect affecting these techniques efficacy, we suggest they would be equally effective; however, the TL technique was nearly twice as effective. Additionally, the MDC for the Latissimus dorsi muscle length has been reported to be >4cm. Only, the thoracolumbar TM produced change scores greater than 4cms.
It is theorized the presence of structures such as Golgi tendon organs, muscle spindles, Pacini corpuscles, and Ruffini endings present in the TLF and LD structure play a proprioceptive role that may provide additional feedback and allow for an additional effect on the muscle [28]. The quick stretch provided by the TM may provide input into any of these structures thereby eliciting a further increase in shoulder ROM. The mechanism through which this occurred may be associated with increased afferent discharge and motoneuron pool depression or through changes in motor activity such as reflexive muscle activation, decreased resting electromyographic signal intensity, or reduction of pain perception in response to a standard stimulus [42]. However, further study will be necessary to shed light on this mechanism.
Another potential reason for improved shoulder ROM may be the reported hypoalgesic effect associated with spinal TM. A systematic review on spinal TM revealed that all types of pain respond to TM [43]. A decrease in the subjects shoulder pain may have allowed for increased shoulder ROM. The mechanism by which TM alters pain is unknown, however current evidence suggests the rapid hypoalgesia with concomitant sympathetic nervous system and motor system response may be the result of descending inhibition mediated by the periaqueductal gray [44, 45]. Additionally, the forces required to produce a TM may affect the degree of the neurophysiological response [46]. The amount of force required to produce the TLJ TM would be significantly higher than the LC TM technique. This increased force that was dissipated over a large surface area and may have set off a larger reaction of neurophysiologic effects.
Clinical implications for this study are to provide an alternative TM to improve shoulder ROM in the appropriate shoulder patient with RCRSP. The results suggest considering mobility examination of both the LC spine and TL in patients with RCRSP who have pain with overhead reaching. Manual therapy or manipulative techniques to the lower cervical spine may be contraindicated in some patients with RCRSP secondary to concomitant cervical pathology such as cervical fusion making these segments inappropriate for manual therapy. However, the lower thoracic and upper lumbar spines may not be pathological, allowing the TLJ technique to be performed to help the appropriate patient.
In addition, within-session changes such as pain and ROM can be predictive of between session changes. Current evidence has shown the strongest evidence in support of the spine however; studies have also shown support in the shoulder and hip [47-49]. These studies do not appear to indicate long-term functional improvement. This research suggests that using a TM to gain a within-session change in ROM could produce a meaningful change in ROM between visits.
No changes from baseline motion were found at the two-week follow-up for either technique. This was not unexpected as no manual neuromuscular re-education was performed or follow up exercises were given. Furthermore, Wang reported cervical mobilizations at C5- C6 produced increased strength in the shoulder external rotators for 10 minutes before returning to baseline [20]. Further study on the temporal effects of mobilization and TM on ROM are needed. The participants also continued their prior exercises, which were not prescribed by a physical therapist and may not have been specific enough to allow for carry-over effects at two weeks.
This investigation had several limitations. Investigators were not blinding to the TM technique which may have introduced investigator bias. Our study lacked a control group in our design, which may have been beneficial for our analysis, and therefore, we acknowledge that we lack a consistent conclusion. There was a lack of post-intervention neuromuscular re-education which does not reflect a recommended comprehensive multi-modal treatment approach and may have contributed to a lack of change at two-week follow up [2]. Additionally, a power analysis was not performed prior to collecting data from subjects, which, may have varied our sample size. Given the small sample size, it increases the risk of a type II error during data analysis.
We are unable to make any direct cause-and-effect relationship of the techniques in this study to the increase in shoulder ROM. Future research is needed to determine long-term effects of these techniques and the possible mechanisms involved. This may include combining TM with an exercise protocol including neuromuscular re-education of the LD with a longer follow-up to assess more lasting changes. Additionally, performance on an overhead reaching task pre and post intervention is also of interest in patients with RCRSP. Despite these limitations this study suggests both LC and TLJ TM may be correlated with short-term improvements in LD length in subjects with RCRSP.
Conclusion
The results of this investigation appear to demonstrate that LC and TLJ TM were associated with within-session improvements in shoulder flexion immediately following intervention in subjects with RCRSP. Potential mechanisms for this change that may warrant further investigation include reduction of resting muscle tone through alteration of Golgi Tendon Organ and muscle spindle activity, descending pain inhibition mediated by the Periaqueductal Gray (PAG), or the stretch-reflex response. Additionally, investigation is warranted to address potential temporal effects of the interventions on the change in LD muscle length. Although further research is necessary, this preliminary study supports the use of LC and TL TM to improve short term shoulder flexion motion through improvements in Latissimus dorsi muscle length in patients with RCRSP.
References
- Dubé M, Desmeules F, Lewis J, Roy JS (2020) Rotator cuff-related shoulder pain: does the type of exercise influence the outcomes? Protocol of a randomized controlled trial. BMJ Open10:e039976.
- Lewis J (2016) Rotator cuff related shoulder pain: assessment, management and uncertainties. Man Ther 23:57-68.
- Umer M, Qadir I, Azam M (2012) Subacromial impingement syndrome. Orthop Rev 4:e18.
- Seitz Amee L, Philip W McClure, Sheryl Finucane, N Douglas Boardman III and Lori A Michener (2011) Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both. Clin biomech 26:1-12.
- Winters JC, Jorritsma W, Groenier KH, Sobel JS, Meyboom-de Jong B, et al. (1999) Treatment of shoulder complaints in general practice: long term results of a randomised, single blind study comparing physiotherapy, manipulation, and corticosteroid injection. Br Med J 318:1395-6.
- Bang MD, Deyle GD (2000) Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther 30:126-137.
- Bergman GJ, Winters JC, Groenier KH, Pool JJ, Meyboom-de Jong B, et al. (2004) Manipulative therapy in addition to usual medical care for patients with shoulder dysfunction and pain: a randomized, controlled trial. Ann Intern Med 141:432-439.
- Mintken PE, McDevitt AW, Cleland JA, Boyles RE, Beardslee AR, et al. (2016) Cervicothoracic Manual Therapy Plus Exercise Therapy Versus Exercise Therapy Alone in the Management of Individuals With Shoulder Pain: A Multicenter Randomized Controlled Trial. J Orthop Sports Phys Ther 46:617-628.
- Kardouni JR, Pidcoe PE, Shaffer SW, Finucane SD, Cheatham SA, et al.(2015) Thoracic Spine Manipulation in Individuals With Subacromial Impingement Syndrome Does Not Immediately Alter Thoracic Spine Kinematics, Thoracic Excursion, or Scapular Kinematics: A Randomized Controlled Trial. J Orthop Sports Phys Ther 45):527-538.
- Grimes JK, Puentedura EJ, Cheng MS, Seitz A (2019) The Comparative Effects of Upper Thoracic Spine Thrust Manipulation Techniques in Individuals With Subacromial Pain Syndrome: A Randomized Clinical Trial. J Orthop Sports Phys Ther 49:716-724.
- Boyles RE, Ritland BM, Miracle BM, Barclay DM, Faul MS, et al. (2009) The short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Man Ther 14(4):375-380.
- Strunce JB, Walker MJ, Boyles RE, Young BA (2009) The immediate effects of thoracic spine and rib manipulation on subjects with primary complaints of shoulder pain. J Man Manip Ther 17(4):230-236.
- Herrington L, Horsley I (2013) Effects of Latissimus Dorsi length on shoulder flexion in canoeists, swimmers, rugby players, and controls. J Sport Health Sci1:1-4.
- Bhatt CR, Prajapati B, Patil DS, Patel VD, Singh BG, Mehta CD (2013) Variation in the insertion of the latissimus dorsi & its clinical importance. J Orthop 10(1):25-28.
- Laudner LG, Williams JG (2013) The relationship between latissimus dorsi stiffness and altered scapular kinematics among asymptomatic collegiate swimmers. Phys Ther Sport 14(1):50–53.
- Karduna AR, Kerner PJ, Lazarus MD (2005) Contact forces in the subacromial space: effects of scapular orientation. J Shoulder Elb Surg 14(4):393e399.
- Dunning J, Rushton A (2009) The effects of cervical high-velocity low-amplitude thrust manipulation on resting electomyographic activity of the biceps brachii muscle. Man Ther 14(5):508-513.
- Herzog W, Scheele D, Conway PJ (1999) Electromyographic responses of back and limb muscles associated with spinal manipulative therapy. Spine 24(2):2834-2840.
- Keller TS, Colloca CJ (2000) Mechanical force spinal manipulation increases trunk muscle strength assessed by electromyography: a comparative clinical trial. J Manip Physiol Ther 23(9):585-595.
- Wang SS, Meadows J (2010) Immediate and carryover changes of C5-6 joint mobilization on shoulder external rotator muscle strength. J Manipulative Physiol Ther 33(2):102-108
- Dishman DJ, Bulbulian R (2000) Spinal reflex attenuation associated with spinal manipulation. Spine 25(19):2519-2525.
- Pickar J, Kang Y (2006) Paraspinal muscle spindle responses to the duration of a spinal manipulation under force control. J Manipulative Physiol Ther 29(1):22-31.
- Korr IM (1955) Clinical significance of the facilitated state. J Am Osteopath Assoc 54:277-282.
- Pheasant S (2016) Cervical Contribution to Functional Shoulder Impingement: Two Case Reports. Int J Sports Phys Ther 11(6):980-991.
- Suter E, McMorland G, Herzog W, Bray R (1999) Decrease in quadriceps inhibition after sacroiliac joint manipulation in patients with anterior knee pain. J Manipulative Physiol Ther 22(3):149-153.
- Keller TS, Colloca CJ (2000) Mechanical force spinal manipulation increases trunk muscle strength assessed by electromyography: a comparative clinical trial. J Manipulative Physiol Ther 23(9):585-595.
- Suter E, McMorland G, Herzog W, Bray R (2000) Conservative lower back treatment reduces inhibition in knee-extensor muscles: a randomized controlled trial. J Manipulative Physiol Ther 23(2):76-80.
- Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R (2012) The thoracolumbar fascia: anatomy, function and clinical considerations. J Anat 221(6):507-536.
- Hoheisel U, Taguchi T, Treede RD, Mense S (2011) Nociceptive input from the rat thoracolumbar fascia to lumbar dorsal horn neurones. Eur J Pain 15(8):810-815.
- Schleip R, Gabbiani G, Wilke J, Naylor I, Hinz B, et al. (2019) Fascia Is Able to Actively Contract and May Thereby Influence Musculoskeletal Dynamics: A Histochemical and Mechanographic Investigation. Front Physiol 10:336.
- Michener LA, Walsworth MK, Doukas WC, Murphy KP (2009) Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil 90(11):1898-1903.
- Salamh P, Lewis J (2020) It Is Time to Put Special Tests for Rotator Cuff-Related Shoulder Pain out to Pasture. J Orthop Sports Phys Ther 50(5):222-225.
- Mintken PE, Glynn P, Cleland JA (2009) Psychometric properties of the Shortened Disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J Shoulder Elbow Surg 18:920-926.
- Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA (2005) Muscles testing and function with posture and pain. Lippincott Williams & Wilkins: Baltimore 5:1-100.
- Cleland JA, Childs JD, Fritz JM, Whitman JM (2006) Inter rater reliability of the history and physical examination in patients with mechanical neck pain. Arch Phys Med Rehabil 87(10):1388-1395.
- Shahidi B, Johnson CL, Curran-Everett D, Maluf KS (2012) Reliability and group differences in quantitative cervicothoracic measures among individuals with and without chronic neck pain. BMC Musculoskelet Disord 13:215.
- Fernández-de-las-Peñas C, Downey C, Miangolarra-Page JC (2005) Validity of the lateral gliding test as tool for the diagnosis of intervertebral joint dysfunction in the lower cervical spine. J Manipulative Physiol Ther 28(8):610-616.
- Maitland GD (1986) Vertebral manipulation. 7th Edition Elsevier Health Sciences, London, UK.
- Pettman E (2006) Manipulative Thrust Techniques: An evidence-base approach. Aphema Publishing, Canada.
- Pettman E (2006) Manipulative Thrust Techniques: An evidence-base approach. Abbotsford, Canada 186: 170-177.
- Dunning J, Mourad F, Barbero M, Leoni D, Cescon C, et al. (2013) Bilateral and multiple cavitation sounds during upper cervical thrust manipulation. BMC Musculoskelet Disord 14:24.
- Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ (2009) The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther 14(5):531-538.
- Millan M, Leboeuf-Yde C, Budgell B, Amorim MA (2012) The effect of spinal manipulative therapy on experimentally induced pain: a systematic literature review. Chiropr Man Therap 20(1):26.
- Plaza-Manzano G, Molina-Ortega F, Lomas-Vega R, Martínez-Amat A, Achalandabaso A, et al. (2014) Changes in biochemical markers of pain perception and stress response after spinal manipulation. J Orthop Sports Phys Ther 44(4):231-239.
- Vernon H (2000) Qualitative review of studies of manipulation-induced hypoalgesia. J Manipulative Physiol Ther 23(2):134-138.
- Bialosky JE, George SZ, Bishop MD (2008) How spinal manipulative therapy works: why ask why? J Orthop Sports Phys Ther 38(6):293-295.
- Cook C, Lawrence J, Michalak K, Dhiraprasiddhi S, Donaldson M, et al. (2014) Is there preliminary value to a within- and/or between-session change for determining short-term outcomes of manual therapy on mechanical neck pain? J Man Manip Ther 22(4):173-180.
- Garrison JC, Shanley E, Thigpen C, Hegedus E, Cook C (2011) Between-session changes predict overall perception of improvement but not functional improvement in patients with shoulder impingement syndrome seen for physical therapy: an observational study. Physiother Theory Pract 27:137-145.
- Wright AA, Abbott JH, Baxter D, Cook C (2010) The ability of a sustained within-session finding of pain reduction during traction to dictate improved outcomes from a manual therapy approach on patients with osteoarthritis of the hip. J Man Manip Ther 18:166-172.
Google Scholar Cross Ref
Google Scholar Cross Ref
Google Scholar Cross Ref
Google Scholar Cross Ref
Citation: Brown J, Alexander D, Kearns G, Karas S (2022) The Effects of Cervical and Thoracolumbar Thrust Manipulation on Shoulder Range of Motion in Patients with Rotator Cuff Related Shoulder Pain. J Nov Physiother 12: 505. DOI: 10.4172/ 2165-7025.1000505
Copyright: © 2022 Brown J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3264
- [From(publication date): 0-2022 - Dec 05, 2025]
- Breakdown by view type
- HTML page views: 2640
- PDF downloads: 624