Research Article Open Access
The Effectiveness of Interferential Current on Overactive Bladder Syndrome
Ali Rafaqat1*, Muhammad Irfan Sattar2, Muhammad Hafeez3 and Muhammad Farrukh Shahzad41Department of Health Management, European University of Lefke, Lefke, North Cyprus
2Isra Institute of Rehabilitation Science, Isra University, Islamabad, Pakistan
3Agile Institute of Rehabilitation Science, Bahawalpur ,Pakistan
4Department of Health Management, European University of Lefke, Lefke, North Cyprus
- *Corresponding Author:
- Ali Rafaqat
Department of Health Management
European University of Lefke, Lefke, North Cyprus
Tel: 90 5428855418
E-mail: alirafaqat64@gmail.com
Received date: March 19, 2017; Accepted date: May 25, 2017; Published date: June 01, 2017
Citation: Rafaqat A, Sattar MI, Hafeez M, Shahzad MF (2017) The Effectiveness of Interferential Current on Overactive Bladder Syndrome. J Nov Physiother 7:351. doi:10.4172/2165-7025.1000351
Copyright: © 2017 Rafaqat A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Objectives: To determine the effectiveness of interferential current on overactive bladder syndrome. Methodology: It is a quasi-experimental study. The duration of the study is 8 weeks. Total 40 patients were selected for this experimental study from Benazir Bhutto Hospital (BBH) Rawalpindi Pakistan. Sample was drawn through non-probability sampling technique called simple convenient sampling. Standard questionnaire was used for measurement through which results were calculated. Complete information about the patients including their biodata, symptomatology was entered in a Performa and then data was entered on the basis of Overactive Bladder Symptom Score (OABSS) scoring system. A total of 40 patients between the age of 5 to 12 years of age with no gender, religion, or ethnic background differentiation and with the diagnosis of overactive bladder were included. Results: it showed that baseline Mean pyuria was 1.75 ± 0.493 SD and after treatment 1.25 ± 0.439 SD and dysuria baseline mean is 1.78 ± 0.474 SD and after treatment Mean is 1.32 ± 0.423 SD. Hematuria baseline mean is 1.98 ± 0.423 SD and after treatment mean is 1.78 ± 0.158 SD mean frequency of urination is 2.0 ± 0.234 and after treatment mean is 1.2 ± 0.342 bed wetting mean is 1.62 ± 0.423 SD and after treatment mean is 1.22 ± 0.490 SD OABSS Score mean is 2.125 ± 0.334 SD and after treatment mean is 1.55 ± 0.597 SD all values showed significant difference. Conclusion: Interferential Current (IFC) Therapy is a very effective and beneficial tool to improve the symptoms and quality of life of the patients with Hinman syndrome.
Keywords
Pyuria; Dysuria; Hematuria; Hinman syndrome
Introduction
Overactive bladder syndrome (OAB) is a urinary urgency, with or without urinary urgency, following by urinary frequency and nocturia as defined by the International continence society (ICS) [1]. Hinman syndrome (overactive bladder syndrome), also known as nonneurogenic neurogenic bladder syndrome, is a rare entity characterized by non-neurogenic urinary bladder dysfunction. The majority of patients are children in early infancy or in preschool age [2]. Diagnosis of this disorder is made by exclusion and is assigned to those children that have clinical, radiologic, and urodynamic characteristics of a neurogenic bladder with external sphincter dyssynergia, but with no evidence of a neurologic alteration or disorder. Patients with Hinman syndrome generally presents with recurrent urinary tract infections, urinary incontinence, vesicoureteral reflux, hydronephrosis, and acute and chronic renal failure. Due to the low incidence of the disease, there is s no consensus regarding the management and treatment [3]. In 1973, Hinman and Baumann were the first to report a case series of 14 patients with non-neurogenic neurogenic bladder syndrome and treated those patients with bladder training [3]. Some clinicians have established the effectiveness of bladder retraining and medical treatment for its management, while others have employed different treatments such as Botox application in the external sphincter with good results. However, when there is already damage to the upper urinary tract or risk for the same then more aggressive surgical treatment is preferred over conservative treatment in order to prevent chronic renal damage [4].
In a new study, it is estimated that OAB has a significant economic burden, total cost of OAB disease is up to 36.5 billion dollars in adults who sometimes complain of "OAB symptoms" [5].
Western countries (England, Canada, Germany, Sweden, Italy and Spain) used the results obtained from a large epidemiological study as an economic model to calculate the direct and indirect annual costs of OAB. It is estimated that the total annual direct cost of the OAB estimated as $3.9 billion among these countries due to diagnosis and treatment of the diseases, and almost 1.1 billion dollars indirect costs due to the performance decline at the work place and absenteeism. OAB is also associated with other costs such as urinary tract infections, falls, fractures, depression and skin infections [6].
A study published in 2006 by Reeves et al. [7] used a healthcare economic model to calculate the prevalence of OAB in 5 European countries. The model estimates that in 2000, 20.2 million people over age 40 suffered from OAB symptoms and 7 million were urgent with urgent incontinence. A projection using UN population statistics predicts that 25.5 million people will suffer by 2020, suffering from 920 million urgency incontinence. The authors estimate that the OAB total cost for the health system will reach 5.2 billion euros by 2020 [7]. The most recent epidemiological data suggests that OAB affects 68% of adult women in the United States and high anxiety and depression scores and impaired health-related quality of life [8].
OAB has a greater impact on the quality of life of diabetes [9] and more economical burden and cost than rheumatoid arthritis and asthma [10]. For this reason, OAB deserves more research resources and research effort. People who are affected by OAB symptoms tend to reduce their participation in social activities; they isolate themselves and predispose to depression [11]. Moreover, most patients are ashamed of making frequent medical treatments that are often seen and dismissive of the patient's ability to understand the social burden. Some of the symptoms of bladder dysfunction are estimated to occur in about 60% of all patients seeking help [12]. Hence, PAP is a major problem affecting many individuals. The underlying causes are unknown and the exact mode of action of pharmacological treatments remains uncertain. For this reason, new perspectives and new therapeutic methods are urgently needed [13].
Materials and Methods
Study hypothesis
Interferential current (IFC) therapy is beneficial in reducing symptoms of overactive bladder syndrome.
Null hypothesis
Interferential current (IFC) therapy is not beneficial in reducing symptoms of overactive bladder syndrome.
Study design
It is a Quasi-Experimental study. Total 40 patients were selected for this study. Data is collected by using OABSS questionnaire. In this study, interferential current (IFC) was used on S2 and S3 dermatome. And then data was collected before and after treatment.
Participants
Total 40 patients were selected for this interventional study from Benazir Bhutto Hospital (BBH) Rawalpindi Pakistan. Sample was drawn through non-probability convenient sampling technique. Regarding inclusion and exclusion criteria following point were followed for their selection.
Inclusion criteria
All patients of overactive bladder syndrome already diagnosed by urologist between the age of 5-12 years.
Exclusion criteria
Individuals with bladder syndrome due to following reasons:
• Spinal Trauma,
• Diseases that affect nervous system,
• Accidents,
• Spinal surgeries,
• Stroke,
• Parkinson’s disease,
• Spinal-cord injuries,
• Central nervous system tumors,
• Spinal congenital abnormalities,
• Infections of spine.
Instruments
A standard questionnaire was used for measurement was used through which results were calculated. Complete information about the patients including their bio-data, symptomatology was entered in a Performa and then data was entered on the basis of “Overactive Bladder Symptom Score (OABSS)” scoring system.
Data collection procedure
A total of 40 patients between the age of 5 to 12 years of age with no gender, religion, or ethnic background differentiation and with the diagnosis of overactive bladder were approached. All the patients with similar complaints of frequency, urgency or dribbling of urine but with any diagnosis other than bladder syndrome were excluded.
In all patients, the electrodes of IFC were placed on S2 and S3 dermatomes for 20 minutes with frequencies of 4000 Hz.
• S2 Dermatomes Buttock thigh and posterior leg
• S3 Dermatomes Groin, medial thigh to knee
A follow up chart were maintained after every three weeks regarding the symptoms of the patients. After 8 weeks of treatment, the patients were re-evaluated for their symptoms and graded again for the severity of the disease. A comparison was made between data obtained from one groups to check the significance and effectiveness of intervention before and after treatment.
Ethical concerns
All the patients included in the study were informed in detail about the Treatment plan and written consent was obtained.
Significance of study
This study might be potent tool in providing other professional the specific strength to treat overactive bladder syndrome by using Interferential Current (IFC) as this method is cheaper than other medical treatments. The study might also be used as benchmark for other Physical Therapy professional in developing countries to treat overactive bladder syndrome by using interferential current (IFC) which is cheap and easily available modality. This study stresses that the interferential current (IFC) is a potent modality in improving the symptoms of overactive bladder syndrome, thus should be regarded as one of the modality in the profession of physical therapy to treat urinary incontinence (UI).
Results
In this study there were 40 Patients. The analysis was done by the SPSS 16 version.
Age of patients
Out of total participants, as shown in Figure 1, where frequency is the number of patients, 1 (2.5%) participant was of 5 years, 5 (12.5%) were 6 years old, 9 having age of 7 (22.5%), 6 (15%) of 8 years old, 8 (20%) patient of 9 years old 4 (10%) were 10 year old. 6 (15%) of them were 11 years old and 1 (2.5) of them was of 12 year of age.
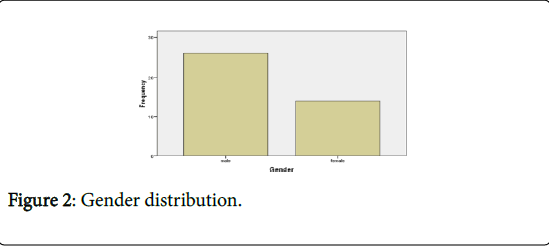
Gender of patients
As shown by Figure 2, In this study 26 (65%) participant were males and 14 (35%) of them were females.
Dysuria
Dysuria refers to painful urination. Table 1 shows that dysuria baseline mean is 1.78 ± 0.474 SD and after treatment Mean is 1.32 ± 0.423 SD the p value <0.05 which shows significant difference between baseline and after treatment mean dysuria.
Frequency of urination
In this quasi experimental study frequency of urination was assessed. Table 1 hows the baseline mean frequency of urination is 2.0 ± 0.234 and after treatment mean is 1.2 ± 0.342. The p value is less than 0.05 which shows significant decrease in frequency of urination after treatment.
Bed wetting
In this quasi experimental study 40 participants were included. Table 1 shows the baseline bed wetting mean is 1.62 ± 0.423 SD and after treatment mean is 1.22 ± 0.490 SD. the p value is less than 0.05 which shows significant difference in bed wetting before and after treatment.
Stools per day
Table 1 shows the baseline stools per day mean is 1.58 ± 0.844 SD and after treatment mean is 2.55 ± 0.749 SD the p value is less than 0.05 which shows significant difference in baseline and after treatment no of stools per day.
OABSS score
Table 1 shows that baseline OABSS Score mean is 2.125 ± 0.334 SD and after treatment mean is 1.55 ± 0.597 SD the p value is less than 0.05 which shows significant difference in OABSS Score before and after treatment. It rejects null hypothesis and accept alternate hypothesis that there is a significant difference in OABSS Score before and after treatment. Which means that Interferential current (IFC) therapy is very beneficial in reducing symptoms of overactive bladder syndrome.
| Variable | Baseline (Mean+S.D) | After treatment (Mean+SD) | P value |
| Dysuria | 1.78 ± 0.474 | 1.32 ± 0.423 | >0.05 |
| Frequency of urination | 2.0 ± 0.234 | 1.2 ± 0.342 | >0.05 |
| Bed wetting | 1.62 ± 0.423 | 1.22 ± 0.490 | >0.05 |
| Stools per day | 1.58 ± 0.844 | 2.55 ± 0.749 | >0.05 |
| OABSS Score | 2.125 ± 0.334 | 1.55 ± 0.597 | >0.05 |
Table 1: OABSS Score (A).
Discussions
In these study 40 patients with mild, moderate and severe categories according to overactive bladder symptoms score, (OABSS) scoring system were selected. The problems of urgency, and frequency were taken to collect data both before and after using Interferential Current (IFC) Therapy to observe the changes that occurred during the study group and controls. The data of the patient before and after Interferential Current (IFC) Therapy shows the significance changes which improve the functional activities of the patient.
Several results from the present study showed that an overall improvement in urinary symptoms after Interferential Current (IFC) Therapy. All change would be excepted to reduce the frequency, dribbling, urgency improved bladder function and reduce potential renal damage.
In O ‘Conor study [14], the objective was a correlation between voiding and quality of life. In that study the results confirm the statement that overactive bladder syndrome can strongly affects the patient quality of life. Various authors have confirmed the poor quality of life in patients with overactive bladder syndrome [14].
In literature, there is very limited data available in which OABSS scoring system is used with Interferential Current (IFC) therapy. Previous studies by various authors were done in which they used bladder diaries as a tool of observation. All these studies suggested that Interferential current (IFC) therapy is beneficial in the treatment of overactive bladder syndrome which is in accordance with our study. So, the results of our study are in accordance with previous study as for as effectiveness of Interferential Current (IFC) therapy is concerned but those studies were done mainly on the patients of neuropathic bladder.
Conclusion
Interferential Current (IFC) Therapy is a very effective and beneficial tool to improve the symptoms and quality of life of the patients with Hinman syndrome but still large scale studies with large number of patient and with longer follow up required to confirm the long-term efficacy of Interferential Current (IFC) therapy in such patients.
Although the use of electrical stimulation and neuromodulation to treat patients with OAB has been widely investigated, in many reports important information is not enough and good randomized, placebo controlled studies are rare. The advent of various techniques of neuro modulation causes paradigm shift of treatment strategies of patients with OAB and other lower urinary tract dysfunction. We should compare various techniques and evaluate placebo effects overcoming unsolved aspects of the current treatment including neuro modulation. And our better approaches based on further understanding of voiding function and action mechanism of neuro modulatory techniques might lead more various types of patients with urinary tract dysfunction to more satisfactorily clinical outcomes. In consideration of these problems, I personally expect potential clinical efficacy of IF as short-term electrical stimulation, that has few adverse event, and improving not only Quality of Life (QOL) but Activities of Daily Life (ADL).
References
- Haylen BT (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. NeurourolUrodyn 29: 4-20.
- Bauer SB (2017) The Hinman Syndrome. The Journal of Urology 197: S132-S133.
- Patil SB, KshitizR (2015) Hinman Syndrome-Diagnosis and Management: A Rare Case Report. IJSS Case Reports & Reviews 2: 26-28.
- Chaichanamongkol V, Ikeda M, Ishikura K, Hamasaki Y, Hataya H, et al. (2008) An infantile case of Hinman syndrome with severe acute renal failure. ClinExpNephrol 12: 309-311.
- Onukwugha EZI (2009) The total economic burden of overactive bladder in the United States: a disease specific approach. Am J Manag Care 15: S90-97.
- Irwin DE, Mungapen L, Milsom I, Kopp Z, Reeves P, et al. (2009) The economic impact of overactive bladder syndrome in six Western countries. BJU Int 103: 202-209.
- Reeves P, Irwin D, Kelleher C, Milsom I, Kopp Z, et al. (2006) The current and future burden and cost of overactive bladder in five European countries. EurUrol 1050-1057.
- Milsom I, Kaplan SA, Coyne KS, Sexton CC, Kopp ZS (2012) Effect of bothersome overactive bladder symptoms on health related quality of life, anxiety, depression and treatment seeking inthe United States: results from EpiLUTS. Urology 80: 90-96.
- Hashim HAP (2007) Overactive bladder: an update. CurrOpinUrol 17: 231-236.
- Coyne KS, Sexton CC, Thompson CL, Clemens JQ, Chen CI, et al. (2012) Impact of overactive bladder on work productivity. Urology 80: 97-103.
- G (2004) Management of overactive bladder. N Engl J Med 350: 786-799.
- Goepel M, Hoffmann JA, Piro M, Rubben H, Michel MC (2002) Prevalence and physician awareness of symptoms of urinary bladder dysfunction. EurUrol 41: 234-239.
- Al Mosawi JA (2007) Identification of non-neurogenic neurogenic bladder in infants. Urology 70: 355-356.
- O’Conor RM, Johanneson M, Hass SL, Kobelt-Nguyen G (2009) Urge incontinence Quality of life and patients valuation of symptoms reduction. Pharmacoeconomics 14: 531-539.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 3825
- [From(publication date):
June-2017 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 2978
- PDF downloads : 847