The Effectiveness of Achilles Lengthening Plus Intralesional Human Recombinant Epidermal Growth Factor to Prevent Recidivism of Neuropathic Diabetic Forefoot Ulceration
Received: 07-Sep-2017 / Accepted Date: 03-Oct-2017 / Published Date: 11-Oct-2017 DOI: 10.4172/2329-910X.1000248
Abstract
Objective: To assess the effectiveness and safety of the combination of z-plasty lengthening of Achilles tendon.
Study Design: Sixty-two neuropathic forefoot ulceration in fifty-four diabetic subjects were included on this prospective, Open, Uncontrolled, Non Randomized, Observational study. The eligibility criteria included normal physical activity with no antecedent of minor amputation, and an ankle dorsiflexion range of motion (DF-ROM) minor of 15 degrees measures with goniometer. Eligible patients were referred to the Vascular Surgery Service of the Clinic Surgical Hospital “José R. Lopez Tabrane” in Matanzas, Cuba from January 2009 to May 2015. The follow-up process ends in December 2016. Based on non-probability consecutive sampling thirty-one patients with thirty-five neuropathic forefoot ulcerations (NFU) were included in the treatment group and twenty-three patients with twentyseven NFU in the control. plus intralesional administration of human recombinant Epidermal Growth Factor in the reduction of the recidivism of neuropathic forefoot ulceration.
Results: Sixty-two neuropathic forefoot ulceration in fifty-four diabetic subjects who met the eligibility criteria (inclusion and exclusion) were included in this study. Groups were comparable according to demographic and baseline characteristics. The recidivism of showed a 9 times reduction and the rate of new lesson was reduced in 3.1 times. Both findings of clinical relevance. The most frequent complications were Local pain 5.7% (n=3) in the treatment group, and 14.8% (n=4) in the control group. There were not minor or major amputations reported as an outcome of treatment.
Conclusion: Combination of z-plasty lengthening of Achilles tendon plus intralesional administration of Human Recombinant Epidermal growth factor reduces the recidivism and the new lessons. This therapeutic association was considered effectiveness and safety for the prevention of the recidivism and new lessons in the neuropathic ulceration of the forefoot.
Keywords: Diabetic foot ulcer; Neuropathic ulceration; Diabetic foot surgery; Epidermal growth factor; Wound healing
8950Introduction
Diabetic foot ulcers (DFUs), is among the most significant complications of diabetes it involves approximately 15% of diabetic population and a leading cause of hospitalization and amputations Diabetic foot (DF) is one of the main complications of diabetes mellitus; and represents the main cause of amputation [1,2]. DF is a multifactorial disease, can either be associated with neuropathy (neuropathic ulcer), peripheral vascular disease (ischemic ulcer), or both (neuroischemic ulcer), although the final etiopathogenetic pathway may involve a combination of these primary risk factors and other causal factors such as trauma [3].
One of the most serious consequences of the Diabetic neuropathy is the associated loss of protective sensation with the development of recurrent ulcers on the plantar surface of the foot. 1–3 Limited ankle dorsiflexion (eg, equinus deformity) has been implicated as a contributing factor in recurrent ulceration, presumably because this deformity prevents the leg from rolling over the foot during the late stance phase of gait, resulting in excessive plantar pressures [4-7]. Excessive plantar pressures result in tissue breakdown and delayed wound healing [8]. Surgical Tendo-Achilles lengthening (TAL) will increase ankle dorsiflexion range of motion, cause a reduction of the plantar pressures, and prevent skin breakdown [9]. There is a risk reduction for short-term and long-term ulcer recurrence for subjects who received TAL [10].
Cutaneous wound healing is a multistep process requiring the interaction and coordination of many different cell types and molecules [11]. A series of multiple complex pathophysiological mechanisms, can contribute to lack of healing in persons with DFUs including decreased or impaired growth factor production, angiogenic response, quantity of granulation tissue, keratinocyte and fibroblast migration and proliferation, bone healing, and balance between the accumulation of ECM components and their remodelling by MMPs [12]. The adjunctive therapies target different stages of the healing process have been proposed because of the suboptimal healing rates often observed in practice, epidermal growth factor (EGF) stimulates the proliferation of fibroblasts, keratinocytes and vascular endothelial cells, which contribute to its scar tissue formation property [13]. Its action is launched by the interaction with specific receptors located on the cellular membrane, expressed on most human cell types including those which play critical roles for wound repair such as fibroblasts, endothelial cells and keratinocytes. The EGF-induced mitogenic, motogenic, and cyto-protective actions are instrumental for healing events that may be summarized as: (a) stimulation of productive cells migration toward the injured area, (b) stimulation of granulation tissue outgrowth–including extracellular matrix accumulation, maturation and de novo angiogenesis, (c) stimulation of wound contraction by myofibroblast activation and proliferation, (d) stimulation of the damaged area resurfacing by epithelial cells migration and proliferation [14]. EGF is also endowed with angiogenic activity thus promoting the growth of a vascular mesh within the wound bed. It seems as if the tissue treated with intralesional EGF keeps a sort of “memory” of the treatment received, which is not transferable to nontreated zones [15]. The purposes of this article is to assess the effectiveness and safety of the combination of z-plasty lengthening of Achilles tendon plus intralesional administration of human recombinant Epidermal Growth Factor in the reduction of the recidivism of neuropathic forefoot ulceration
Material and Methods
Study design
Sixty-two neuropathic forefoot ulceration in fifty-four diabetic subjects were included on this prospective, Open, Uncontrolled, Non Randomized, Observational study. The eligibility criteria it means patients with conditions that interfere with the evaluation, because of the modification of the weight bearing forces (conditioned shear stress), and by a non-probability consecutive sampling patients were included in treatment or control group. Eligible patients were referred to the Vascular Surgery Service of the Clinic Surgical Hospital “José R. Lopez Tabrane” in Matanzas, Cuba from January 2009 to May 2015. The follow-up process ends in December 2016. Based on nonprobability consecutive sampling thirty-one patients with thirty-five neuropathic forefoot ulcerations (NFU) were included in the treatment group (lengthening of Achilles tendon plus intralesional administration of Human Recombinant Epidermal growth factor) and twenty-three patients with twenty-seven DFU in the control (lengthening of Achilles tendon). To be eligible to participate, patients needed to provide its voluntariness through an informed consent previous to the surgical procedure, be older than 18 years old, and documented diagnosis of diabetes type 1 or 2 according to the criteria of the Latin-American association of Diabetes 2000 Guide, have a documented diagnosis of neuropathic ulceration of the forefoot, and lack of clinical evidence of ischemic (with ABI<0.7) or soft tissue infection. Patients were excluded if they had a history of chronic uncompensated diseases, including cardiopathy with miocardial infartion, unestable angina or cardiac insuficiency with edemas in the last 3 months; diabetic coma; hepatic insuficiency; moderate to grave or renal failure (creatinine>200 mmol/L and oligoanuria); Hemoglobin<100 g/L; antecedents or suspicion of malignant diseases; psychiatric diseases that compromise the treatment or the evaluations; pregnancy or current breastfeeding or hhypersensitivity to the product or any of this component.
In the assessment of the effectivenes, the main response variable: Proportion of patients with Recidivism (defined when there is reopening of a wound in the same place of the treated previous wound). The secondary variable of effectivenes is the Proportion of patients with new lessons (defined when there is opening of a wound in another place of the treated previous foot or in the contralateral foot). The safety variables include type, duration, intensity, seriousness as well as the adopted measure. The assessments on safety will include physical examination, interview and clinical laboratory parameters. The Severity of adverse events was classified as (i) mild, because no therapy was necessary; (ii)or moderate, if specific treatment was needed and (iii) severe, in case of death, life-threatening, hospitalization or its prolongation. The control variables includes age, gender, ethnicity, type of diabetes mellitus (type 1 or 2); Time of evolution of the diabetes mellitus, Current treatment for the diabetes (oral hypoglycemic drugs or insulin); Stage according to the Wagner’s classification, presence of unresolved osteomyelitis.
Treatment protocols
After patients were selected for enrollment in the study, they were fully informed of the nature of the study and provided a written informed consent. During the primary assessment a detailed past medical history was taken for the identification of the duration of diabetes mellitus, previous ulcers, treatments used and allergies to drugs. A comprehensive thorough physical examination of the lower extremities and the ulcers was carried out and photographs of the wounds were taken and the exact surface area of the wound was measured. Baseline laboratory tests were carried out for a complete blood count, erythrocyte sedimentation rate, fasting blood sugar, lipid profile, liver and renal function tests plus serum phosphorus, calcium, sodium, potassium and amylase. Goniometric and vascular evaluation was done.
After the evaluation, the methodology of treatment was
• Group A z-plasty lengthening of Achilles tendon plus intralesional administration of human recombinant Epidermal Growth Factor, for the standard method, from this product was used the lyophilized formulation of 75 μg; with a frequency of infiltration of 3 times per week until the healing (reepithelization) of the wound (defined like the absent of necessity of local dressing and bandages) or until 24 doses (8 weeks of treatment).
• Group B z-plasty lengthening of Achilles tendon (according the specific indication).
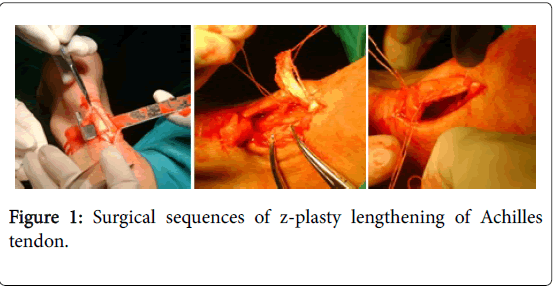
Surgical sequences of z-plasty lengthening of Achilles tendon are shown in Figure 1.
Statistical analyses
The Statistical analyses of the results were performed using SPSS version 19.0 for windows (IBM-SPSS, Inc, Armonk, NY), Exploratory analysis for each variable (main, secondary and control) were performed to evaluate their global behavior and evaluate the hypothesis applying proper statistical tests in the assessment stage. With the quantitative variables the measurements of the central tendency and dispersion were estimated.
For all variables (quantitative and qualitative), the logistic regression model was adjusted to study the influence of each variables and their interactions on the response to the treatment and occurrence of serious adverse events. The hypothesis that there is a difference between independent qualitative variable and dependent quantitative was established by calculation of the Odds ratio(OR), with a probability beta a priori for p<0.05.
Ethics
The protocol was approved by the institutional review board (IRBJLT 021/2008) of the Clinic Surgical Hospital “José R. Lopez
Tabrane” in Matanzas, Cuba and the IRB of the Matanzas University of Medical Sciences, Matanzas City, Cuba. Patients were fully informed about the aim of the study and they were told that their participation was optional. Written informed consent was obtained from each participant.
Results
Basic characteristics
Sixty-two neuropathic fore foot ulceration in fifty-four diabetic subjects who met the eligibility criteria (inclusion and exclusion) were included in this study (Table 1). The mean age of the participants was 54.6 ± 6.5 years in the treated and 54.7 ± 6.8 years in controls. In both groups predominate the female, and in the ethnicity the mestizo group, and for the clinical point of view the type 2 of diabetes with a time of evolution of 15.8 ± 3.5 years in group A and 14.9 ± 4.1 years in group B, according to the gradation by Wagner the grade 2 is the most prevalent. According to this finding is possible to establish that the Groups were comparable according to demographic and baseline characteristics.
| Variables | Group A Treatment (n=35) | Group B Control (n=27) | ||
|---|---|---|---|---|
| Age (median and standard deviation) | 54.6 ± 6.5 years | 54.7 ± 6.8 years | ||
| Gender | Female | n =19 (54.3%) | n=15 (55,5%) | |
| Male | n =16 (45.7%) | n= 12 (44,5%) | ||
| Ethnicity | Yellow | n=2 (5.7%) | n=1 (3.7%) | |
| White | n=10 (28.6%) | n=8 (29.6%) | ||
| Mestizo | n=17 (48.6%) | n=13 (48.1%) | ||
| African descent | n=6 (17.1%) | n=5 (18.6%) | ||
| Type of DM | Type 1 | n= 2 (5.7%) | n= 1 (3.7%) | |
| Type 2 | n= 33 (94.3%) | n=26 (96.3%) | ||
| Time of evolution of the diabetes mellitus (years) | 15.8 ± 3.5 years | 14.9 ± 4.1 years | ||
| Wagner´s grade | 2 | n=24 (68.6%) | n=18 (66.7%) | |
| 3 | n= 11 (31.4%) | n= 9 (33.3%) | ||
| Legend. DM: diabetes mellitus, DFU: diabetic foot ulcer. | ||||
Table 1: Demographic and baseline clinical findings in the patients includes in the study. Matanzas. 2009-2016.
Efficacy assessment
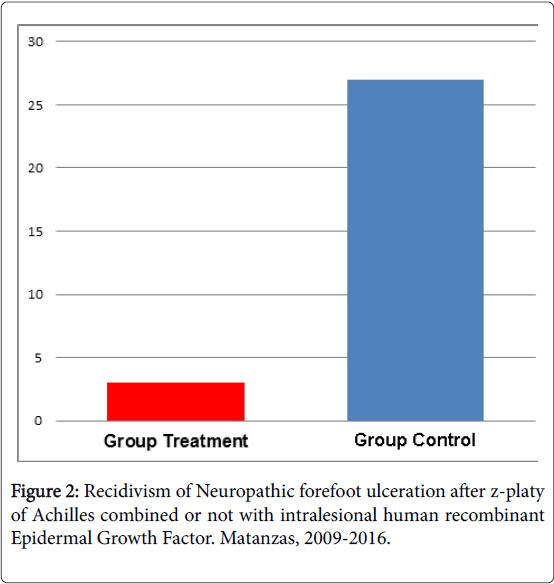
The recidivism of neuropathic forefoot ulceration after z-plasty lengthening of Achilles tendon plus intralesional administration of Human Recombinant Epidermal growth factor (Figure 2) showed a reduction from 27% in the Control group to 3% in the Treated group, it means 9 times less frequent, results that sustain the clinical relevance of this observation according to the existence of statistical significance for a confidence interval of <0.05. The logistic regression model, shows a bad prognosis for the presence of unresolved osteomyelitis (OR: 7.2), and protective factor were minor time of evolution of Diabetes Mellitus (OR: -0.712) and older people (OR:-0.615).
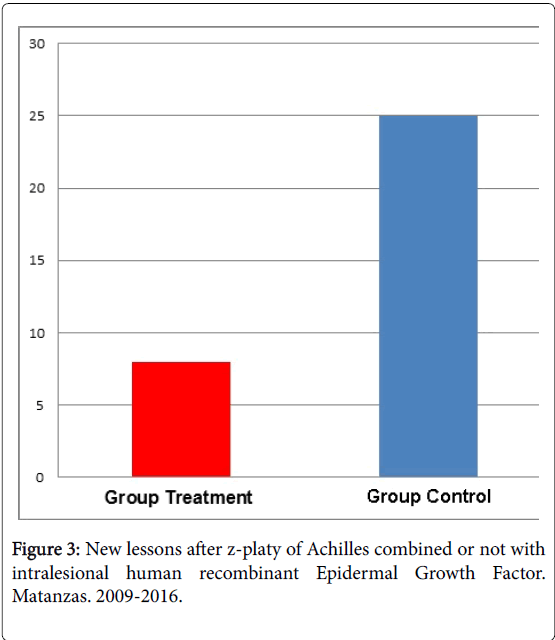
The rate of new lesson (Figure 3) is compared in both groups, and is reduced from 25 in Control group to 8 in the treated patients, it means 3.1 times of reduction. This finding of clinical relevance. The multivariate analysis establishes like risk factors the presence of unresolved osteomyelitis (OR: 5.7) and the minor time of evolution of the diabetes as protector (OR: -0.417).
Assessment of the safety results
Safety was monitored daily during treatment and during 6 months after the closure of the study. The most frequent complications (Table 2) in the treatment group was Local pain 5.7% (n=3), local infection of the surgical incision 2.8% (n=1) and shivering 2.8% (n=1). The control group had 14.8% (n=4) of local pain, 7.4% (n=2) of Local infections of the surgical incision and 3.7% (n=1) of border necrosis. The multivariate analysis show risk factors unresolved osteomyelitis (OR, 2.6) and protective factors, gender female (-0,972), insulin therapy (-0,876) and older patient (-0,542). There were not minor or major amputations reported as an outcome of treatment.
| Complications | Group A Treatment | Group B Control | ||
|---|---|---|---|---|
| No | % | No | % | |
| Local infections of the surgical incision | 1 | 2.80% | 2 | 7.40% |
| Local pain | 3 | 5.70% | 4 | 14.80% |
| Shivering | 1 | 2.80% | - | - |
| Border necrosis | - | - | 1 | 3.70% |
Table 2: Adverse events in both groups. Matanzas, Cuba. 2009-2016.
Discussions
Researchers have suggested that certain surgical interventions can reduce the risk of foot ulcer recurrence in patients with diabetes and peripheral neuropathy [16].
Healing diabetic toe ulcers can be a challenging and protracted process with high recurrence rates, negatively affecting the patients’ quality of life and potentially leading to amputation. It is therefore highly important to establish effective interventions to reduce these negative consequences [9,10].
Increased plantar pressures in conjunction with neuropathy have been implicated in the development of plantar foot ulceration in people with diabetes [17]. Limited ankle joint mobility, as seen clinically as a tight Achilles’-gastrocnemius-soleus complex, is a deforming force and a causative factor in plantar forefoot ulcerations [18-20]. During normal gait, 10° of dorsiflexion at the ankle is required, and anything less will increase plantar pressures in the forefoot and impede healing of the wound [17]. As a strategy to reduce the severity of recurrence and extend ulcer-free days of activity, investigators have explored a variety of approaches, the tendo-Achilles’ lengthening (TAL) has been demonstrated be effective, because of alleviate the pressure, with a temporary reduction in peak forefoot pressures which ultimately returned to baseline levels by 7 months [20-22].
Adjuvant therapies and advanced technologies can be used in addition to standard care as a second line of treatment when appropriate [22]. These include some topical drugs but are mostly medical devices: living skin equivalents, specialized dressings, hyperbaric oxygen therapy and negative pressure devices [6]. These interventions provide moderate improvement over standard treatments, generally only 15% to 20% healing in less than 20 weeks, and may be time consuming [21]. The fluid and exudate found in Diabetic chronic wounds contain typical factors that have a number of negative effects on the healing process; including the existence of a particular protease with insulin-degrading activity the susceptibility of the diabetic wounds to host an abnormal bacterial burden that reduce GFs availability, amplify the inflammatory response and prevent the storage of GFs within the extracellular matrix, as well as the inhibition of cell proliferation [23-25].
Growth factors brought hopes to scientists and clinicians involved in the field of wound repair [26]. The rationale confirm that Diabetic wounds exhibit other distinctive elements among the variety of chronic wounds [27,28]. The first to mention is the, which has been shown to correlate with the level of glycated haemoglobin, suggesting a direct relationship between glycaemia and the wound proteolytic profile. Locally injected hrEGF could stimulate the survival and repair of cutaneous and adjacent soft tissues in a context of circulatory neurogenic deterioration [14]. Such knowledge prompted the hypothesis that injecting hrEGF deep into the wound base and walls would allow for greater pharmacodynamic response in terms of granulation tissue growth and wound closure. In further studies, single or repeated hrEGF systemic or local injections produced clear-cut cytoprotective and proliferative responses, suggesting an intrinsic ability of hrEGF at supraphysiological concentrations to trigger biological events necessary for tissue repair [29]. The first clinical evidences on hrEGF infiltrative treatment involved diabetic foot ulcers and amputation residual bases. All the lesions were chronic, complex and recalcitrant to heal; staged as III and IV of the Wagner’s scale. The efficacy showed in this type of wounds paved the way for a solid clinical development [30]. Since then, hrEGF local injection has been used for complex diabetic wounds in various Cuban clinical trials, demonstrating a favourable risk–benefit balance by speeding healing, reducing recurrences and attenuating amputation risk. EGF infiltration increased and accelerated healing in poor-prognosis wounds toward a rapid and sustained response [29].
The historical reports had varying levels of implementation of “standard” foot care vs. insoles or footwear. A weighted average of these historical recurrence rates was calculated (range: 5-58%) resulting in a mean 20.4% (SD=0.17) [31-34]. In the clinical trials done in Cuba with hrEGF with a mean follow-up time was 2.9 years (maximum 8 years). The frequency of relapses at any moment was significantly lower (p<0.001) in patients that received rhEGF as compared to the control group of the confirmatory. This effect was obtained for both neuropathic and ischemic patients. On the contrary, no effect was seen on the appearance of new DFU on other locations (mainly on the contralateral limb). The rates were 8.8%, 8.2%, and 11.6% for patients treated with 75 μg rhEGF, 25 μg, and placebo, respectively [35]. It seems as if the tissue keeps a sort of “memory” of the treatment received, which is not transferable to non-treated zones. These results were confirmed in the postmarketing study where the relapse and new lesions rates were 5% and 9.5% person-years, respectively [36-39].
Conclusion
Combination of z-plasty lengthening of Achilles tendon plus intralesional administration of Human Recombinant Epidermal growth factor reduces the recidivism of neuropathic forefoot ulceration in 9 times and the new lessons in 3.1. The safety profile was appropriated according to the low frequency of complications, and the light or moderate characteristic of them; the most frequently was local pain. The logistic regression model shows the unresolved osteomyelitis like a risk factor for the development of recidivism, new lessons and complication. This therapeutic association is effectiveness and safety for the prevention of the recidivism and new lessons in the neuropathic ulceration of the forefoot.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
- GarcÃa Herrera ArÃstides L, Fernández M, José I, RodrÃguez Fernández, Raúl (2004) The diabetic foot Madrid Elsevier 38-69.
- Schaper NC, Van Netten JJ, Apelqvist J, Lipsky BA, Bakker K et al. (2016) Prevention and management of foot problems in diabetes: a summary guidance for daily practice 2015, based on the iwgdf guidance documents. Diabetes Metab Res Rev 32: 7-15.
- Nickerson DS, Rader AJ (2013) Low long-term risk of foot ulcer recurrence after nerve decompression in a diabetes neuropathy cohort. J Am Podiatr Med Assoc 103: 380-386.
- DiLiberto FE, Tome J, Baumhauer JF, Houck J, Nawoczenski DA (2015) Individual metatarsal and forefoot kinematics during walking in people with diabetes mellitus and peripheral neuropathy. Gait Posture 42: 435-441.
- Abu Obaid HA, Eljedi A (2015) Risk factors for the development of diabetic foot ulcers in Gaza Strip: a case-control study. Int J Diabetes Res 4: 1-6.
- Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Davignon DR, et al. A prospective study of risk factors for diabetic foot ulcer. The seattle diabetic foot study. Diabetes Care 22: 1036-1042.
- Mueller MJ, Maluf KS (2002) Tissue adaptation to physical stress: A proposed “Physical Stress Theory†to guide physical therapy practice, education, and research. Phys Ther 82: 383-403.
- Mohammed SI, Mikhael EM, Ahmed FT, Al-Tukmagi HF, Jasim AL, et al. (2016) Risk factors for occurrence and recurrence of diabetic foot ulcers among Iraqi diabetic patients. Diabetic Foot Ankle 7: 29605 – 29612.
- Yazdanpanah L, Nasiri M, Adarvishi S (2015) Literature review on the management of diabetic foot ulcer. World J Diabetes 6: 37-53.
- La Fontaine J, Lavery LA, Hunt NA, Murdoch DP (2014) The role of surgical off-loading to prevent recurrent ulcerations. Int J Low Extrem Wounds 13: 320–334.
- Giacomozzi C, Leardini A, Caravaggi P (2014) Correlates between kinematics and baropodometric measurements for an integrated in-vivo assessment of the segmental foot function in gait. J Biomech 47: 2654-2659.
- Shailesh KS, Ashok K, Sushil K (2012) Prevalence of diabetic foot ulcer and associated risk factors in diabetic patients from north India. J Diabet Foot Complic 4: 83-91.
- Novak AC, Mayich DJ, Perry SD, Daniels TR, Brodsky JW (2014) Gait analysis for foot and ankle surgeons— topical review, Part 2: approaches to multisegment modeling of the foot. Foot Ankle Int 35: 178-191.
- Bakker K, Apelqvist J, Lipsky BA, Van Netten JJ (2016) The 2015 IWGDF guidance documents on prevention and management of foot problems in diabetes: Development of an evidence-based global consensus. Diabetes Metab Res Rev 32: 2-6.
- van Netten JJ, Price PE, Lavery LA, Monteiro-Soares M, Rasmussen A, et al. Prevention of foot ulcers in the at-risk patient with diabetes: A systematic review. Diabetes Metab Res Rev 32: 84-98.
- Pound N, Chipchase S, Treece K, Game F, Jeffcoate W (2005) Ulcer-free survival following management of foot ulcers in diabetes. Diabet Med 22: 1306-1309.
- Colen LB, Kim CJ, Grant WP, Yeh JT, Hind B (2013) Achilles tendon lengthening: Friend or foe in the diabetic foot? Plast Reconstr Surg 131: 37–43.
- Dallimore SM, Kaminski MR (2015) Tendon lengthening and fascia release for healing and preventing diabetic foot ulcers: A systematic review and meta-analysis J Foot and Ankle Res 8: 85-86.
- Ledoux WR, Shofer JB, Cowley MS, Ahroni JH, Cohen V, et al. (2013) Diabetic foot ulcer incidence in relation to plantar pressure magnitude and measurement location. J Diabetes Complications 27: 621–626.
- Bohn B, Herbst A, Pfeifer M, Krakow D, Zimmy S, et al. (2015) Impact of physical activity on glycemic control and prevalence of cardiovascular risk factors in adults with Type 1 diabetes: A cross-sectional multicenter study of 18,028 patients. Diabetes Care 38: 1536-1543.
- Bus SA, van Deursen RW, Armstrong DG, Lewis JE, Caravaggi CF, et al. (2016) Footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in patients with diabetes: A systematic review. Diabetes Metab Res Rev 32: 99–118.
- Bus SA, van Netten JJ, Lavery LA, Monteiro-Soares M, Rasmussen A, et al. (2016) IWGDF guidance on the prevention of foot ulcers in at-risk patients with diabetes. Diabetes Metab Res Rev 32: 16–24.
- Tamir E, S. Finestone A, Avisar E, Agar G (2016) Mini-invasive floating metatarsal osteotomy for resistant or recurrent neuropathic plantar metatarsal head ulcers. J Orthop Surg Res 11: 414-418.
- Lavery LA, La Fontaine J, Kim PJ (2013) Preventing the first or recurrent ulcers. Med Clin North Am 97: 807-820.
- DiLiberto FE, Baumhauer JF, Nawoczenski DA (2016) The prevention of diabetic foot ulceration: How biomechanical research informs clinical practice. Braz J Phys Ther 20: 375-383.
- Francia P, Anichini R, De Bellis A, Seghieri G, Lazzeri R, et al. (2015) Diabetic foot prevention: the role of exercise therapy in the treatment of limited joint mobility, muscle weakness and reduced gait speed. Ital J Anat Embryol. 120: 21-32.
- Sacco IC, Sartor CD (2016) From treatment to preventive actions: improving function in patients with diabetic polyneuropathy. Diabetes Metab Res Rev 32: 206-212.
- Cavanagh PR, Bus SA (2010) Off-loading the diabetic foot for ulcer prevention and healing. J Vasc Surg 52: 37–43.
- Game FL, Attinger C, Hartemann A, Hinchliffe RJ, Löndahl M, et al. (2016) IWGDF guidance on use of interventions to enhance the healing of chronic ulcers of the foot in diabetes. Diabetes Metab Res Rev 32: 75-83.
- Berlanga J (2011) Diabetic lower extremity wounds: the rationale for growth factors-based infiltration treatment. Int Wound J 8: 612–620.
- Berlanga J, Ms DVM, Fernández JI, Ms EL, López PA, del RÃo A, et al. (2013) Heberprot-P: A Novel Product for Treating Advanced Diabetic Foot Ulcer. Medicc Rev 15: 11–15.
- Fernández-MontequÃn JI, Valenzuela-Silva CM, González-DÃaz O, Savigne W, Sancho-Soutelo N, et al. (2009) Intralesional injections of recombinant human epidermal growth factor promote granulation and healing in advanced diabetic foot ulcers. Multicenter, randomized, placebo-controlled, double blind study. Int Wound J 6: 432- 443.
- López-Saura PA, Yera-Alos IB, Valenzuela-Silva C, González-DÃaz O, RÃo-MartÃn Ad, et al. (2013) Medical Practice Confirms Clinical Trial Results of the Use of Intralesional Human Recombinant Epidermal Growth Factor in AdvancedDiabetic Foot Ulcers. Adv Pharmacoepidem Drug Safety 2: 128.
- Yera-Alos I, Alonso-Carbonell L, Valenzuela-Silva CM, Tuero-Iglesias AD, Moreira-MartÃnez M, et al. Active post-marketing surveillance of the intralesional administration of human recombinant epidermal growth factor in diabetic foot ulcers. BMC Pharmacol Toxicol 14: 44.
- GarcÃa Herrera AL, RodrÃguez Fernández R, Ruiz VM, RodrÃguez Hernández L, Acosta Cabadilla L, et al (2011) Reduction in the amputation rate with Heberprot P in the local treatment of diabetic foot. Spanish J Surg Res 14: 21–26.
- GarcÃa Herrera AL, Febles Sanabria R, Cabadilla Acosta L, Moliner Cartaya M (2015) Tratamiento quirúrgico curativo combinado con Heberprot-P® en las úlceras neuropáticas del antepié. Rev Cubana Angiol Cir Vasc 16: 125-138.
Citation: Herrera AIG, Sanabria RDJF, Cartaya MM (2017) The Effectiveness of Achilles Lengthening Plus Intralesional Human Recombinant Epidermal Growth Factor to Prevent Recidivism of Neuropathic Diabetic Forefoot Ulceration. Clin Res Foot Ankle 5: 248. DOI: 10.4172/2329-910X.1000248
Copyright: © 2017 Herrera AIG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3997
- [From(publication date): 0-2017 - Jul 03, 2025]
- Breakdown by view type
- HTML page views: 3089
- PDF downloads: 908