The Effectiveness of a Family-Centered Childhood Obesity Intervention at the YMCA: A Pilot Study
Received: 13-Feb-2018 / Accepted Date: 21-Feb-2018 / Published Date: 23-Feb-2018 DOI: 10.4172/2161-0711.1000591
Abstract
Objective: Community-based, family-centered obesity prevention/treatment initiatives have been shown to be effective in reducing body mass index (BMI) and improving healthy habits in children if implemented with high intensity and sufficient duration. Let's Go! 5-2-1-0 Program (5-2-1-0) was incorporated into family-centered, monthly physical activity classes and cooking classes over six months delivered by Young Men's Christian Association (YMCA) staff. We hypothesized that implementation of this intervention would improve 5-2-1-0 knowledge attainment, increase healthy behavior (based on 5- 2-1-0 curriculum), and improve BMI and waist circumference measurements in children.
Methods: Children attending YMCA summer camps in Rochester, MN, during 2016 were recruited via study packets mailed to their families. Height, weight, and waist circumference measurements as well as the results of the Modified Healthy Habits Survey and the 5-2-1-0 Knowledge Acquisition Survey were recorded for each participating child at baseline and 6-month follow-up. The intervention group received monthly healthy habit reminder emails, and was invited to monthly evening cooking and physical activity classes for 7 sessions over a 6-month period.
Results: Fifteen families in the intervention group attended classes. Of those, 13 families regularly participated in (attended at least 5 out of 7) both the monthly physical activity and cooking classes. The children in the intervention group had a significant improvement in the number of Knowledge Acquisition Survey questions answered correctly (p<0.001), while there was no improvement in the control group. As compared to children in the control group, there was no significant change in BMI or waist circumference or healthy habits in the intervention group.
Conclusion: Our study findings indicate that our intervention resulted in improved knowledge about healthy habits, but did not significantly impact healthy habits or BMI. Potential reasons for this were the small sample size and the attenuated length and/or intensity of the intervention.
Keywords: Cooking; Exercise; Family; Healthy lifestyle; Obesity; Overweight; Pediatric obesity
Introduction
Childhood obesity is a public health crisis in the United States. According to the National Center for Health Statistics data brief, the prevalence of obesity in children in 2015-16 was at 18.5% [1]. Obese children have an increased risk of developing obesity-related chronic diseases into adulthood [2,3]. Community-based, family-centered obesity prevention/treatment initiatives have been shown to be effective in reducing body mass index (BMI) and improving healthy habits in children if implemented with high intensity and sufficient duration [4,5].
Families that eat and cook together do better with healthy habits such as eating more fruits and vegetables and drinking less sugary beverages [6-10]. Multiple organizations, including the American Dietetic Association, Young Men’s Christian Association (YMCA), American Academy of Pediatricians, and National Academy of Medicine support family-based programs which encourage healthy nutrition and parent education/modeling [11-14].
There is evidence supporting the benefits of involving the family as a whole, as opposed to children alone, in prevention of childhood obesity as this allows for breaking of barriers that families face in adopting healthier lifestyles [15-18]. For instance, a study by Robson et al had parents and children participate in a 10-week cooking class program in hopes it would encourage less eating outside the home. The study demonstrated that the proportion of dinners consumed outside the home by families decreased significantly from 56% at baseline to 25% post-intervention. They concluded that a cooking intervention with behavior modification may be a successful way to help families be healthier [19].
The Let’s Go! 5-2-1-0 Program (5-2-1-0) has been implemented and found to be feasible in many school and community settings in the United States to prevent and treat obesity [20-23]. The daily goals of the program are for children to eat at least 5 servings of fruits and vegetables, limit recreational screen time to 2 or fewer hours, participate in at least 1 hour of physical activity, and to ingest 0 sugary beverages. A recent study in our community evaluated an obesity intervention involving weekly 5-2-1-0 education followed by health coaching from nursing students to 4th and 5th grade children [24]. After four months, the children demonstrated significant decreases in BMI percentile and sugar-containing beverage intake, as well as24 increases in fruit/vegetable intake and daily steps compared to baseline assessment. Another local cluster randomized controlled study, implementing 5-2-1-0 teaching into the regular school curriculum, demonstrated feasibility of such an intervention; however, BMI did not change [25].
The YMCA is an organization with a national program that offers families physical activity and healthy habit class options shown to be effective in treating childhood obesity [13,26]. Focus group interviews for a YMCA family weight management program for elementary school age children, as well as for weight management programs in other settings, show that families prefer interactive sessions including exercise and cooking demonstrations [9,27,28]. Most YMCAs in the United States, including the Rochester Area Family YMCA in Rochester, MN, have adopted a set of Healthy Eating and Physical Activity (HEPA) standards [29].
The implementation of 5-2-1-0 programming into YMCA familybased obesity intervention classes has not been studied. Herein, we undertook a controlled pilot study in conjunction with our local YMCA to evaluate the impact of family-centered health education incorporating 5-2-1-0 principles with cooking and physical activities. We hypothesized that implementation of this intervention would improve 5-2-1-0 knowledge attainment, healthy behavior (regarding self-reported fruit/vegetable intake, sugar containing beverage intake, physical activity level, and reduced screen viewing time), and BMI and waist circumference measurements in children.
Methods
Study participants
Study participants, including both children and their caregivers, were recruited from children entering first through sixth grade (ages 5-13 years) from the 2016 YMCA summer day camp program at the Rochester Area Family YMCA in Rochester, MN.
Recruitment of participants
The summer day camps were advertised using standard communication from the YMCA which did not mention this study. Children could be a biological, adoptive, foster child or ward of the state. They were excluded if parents or legal guardians did not provide consent, the child did not provide assent, or if the families were not fluent in English. This study was approved by the Mayo Clinic Institutional Review Board (IRB).
For the non-intervention (control) arm of the study, YMCA personnel sent a recruitment packet to families of the children enrolled in either Clay Sculpting (n=44) or Sports Camp (n=59) during May and June 2016 which included the invitation letter, a Health Insurance Portability and Accountability Act (HIPAA) form, a demographic survey, and a Modified Healthy Habits survey. Participants returned the form to study staff at Mayo Clinic in the provided envelope. For children whose parents agreed to let their child participate, study staff also obtained assent from the children.
For the intervention arm of the study, subjects were recruited between September and October 2016 from children who participated in YMCA 2016 summer camps other than those from which control participants were recruited. Families were informed of the potential opportunity to participate in evening cooking and physical activity classes using standard communication from the YMCA’s newsletter and email communication. Using a random number technique, packets with study information were then mailed to families (n=415) in waves of up to 100 packets at a time initially and then in smaller waves until we were able to elicit initial interest from 20 families. The goal of 20 families was chosen for feasibility of running this program given the small size of our meeting space. Families provided consent to participate by either mailing completed forms back or bringing them to a study class where study staff collected them. For those children whose parents agreed to let their child participate, study staff also obtained assent from the children.
Study instruments and interventions
Knowledge acquisition survey: This survey was created by the study team and included questions regarding each piece of the 5-2-1-0 messaging described earlier along with a question related to the minimum number of hours of sleep the child should get each night (See addendum).
Modified healthy habits survey: The Healthy Habits Survey was originally designed as a 10-question survey for children ages 2-9 years which assesses physical activity time, screen time, takeout food intake, fruit and vegetable intake, and sugar containing beverage intake [20]. We modified the survey to contain multiple-choice instead of openended responses. We also added a question that elicited the number of hours a night the child sleeps. This survey has been utilized in previous studies [23] but its psychometric properties are not known (See addendum).
Demographic survey: This survey was developed by the study team to provide information on the child’s socio-demographics (See addendum).
BMI measurement: A SECA model 220 scale was utilized to obtain weights and an attached stadiometer was used to obtain heights. Height, weight and waist circumference were measured twice at each assessment period using the same calibrated instruments and then averaged. Age- and sex-specific percentiles for BMI were calculated using the 2000 CDC growth charts [30]. Age- and sex-specific percentiles for waist circumference were calculated using estimates derived from a US National Health and Nutritional Survey [31].
Cooking classes: Each cooking class (lasting 1-2 hours) included a demonstration of food selection, preparation and cooking, followed by eating a healthy meal prepared and served by study staff. A specific 5-2-1-0 health message was delivered by study staff while the participants were eating. These classes introduced families to a variety of foods and also encouraged cooking at home.
Physical activity classes: Each physical activity class, led by YMCA staff, consisted of 1 hour of various exercises or games that involved the participant and family members. During the class session, a specific 5-2-1-0 health message was delivered to the group by study staff.
Study procedures
Height/weight measurements, waist circumference, a knowledge acquisition survey and a Modified Healthy Habits survey were collected in both arms of the study at baseline (November 2016 through first week of February 2017) and at the end of the study (May through July 2017). A variety of day and time options were offered to families to meet with a member of the study team at the YMCA to collect these study measurements. The children had their measurements taken and completed the knowledge acquisition survey; their parent/legal guardian caregivers filled out the study demographics form and Healthy Habits surveys.
The intervention group received invitations to the monthly family cooking classes, family physical activity classes, and 5-2-1-0 healthy habits messaging by monthly email or postal mail from the time of their initial enrollment (October 2016) to the end of the study period (May 2017). The physical activity classes were scheduled twice per month during each of the seven months (November through May); the cooking classes were offered once per month during each of the seven months.
In order to recruit and maximize retention of participants, children received $20 cash cards at baseline and follow-up visits upon completion of the height/weight and waist circumference measurements, the knowledge acquisition survey, and parent/legal guardian completion of the Modified Healthy Habits survey. In addition, the physical activity classes and cooking classes (with meals) were offered free-of-charge. Child participants received an additional $50 cash card if they attended at least 6 of the 7 family cooking classes and an additional $30 if they attended 6 of the 7 physical activity classes (they needed to attend at least one of the two class offerings each month).
Data collection
Data was entered into the Research Electronic Data Capture application tool (REDCap) and stored within a password protected, secure database [32]. The data was only accessible to authorized study team members.
Statistical analysis
Baseline characteristics and outcome measures were compared between the intervention and control groups using the Fisher’s exact test or chi-square test for categorical variables, the two-sample t-test for age, and the Wilcoxon rank sum test for all other continuous or ordinal variables.
Within-group comparisons of measurements at baseline versus post-intervention were evaluated using the Wilcoxon signed rank test. All calculated p-values were two-sided and p-values less than 0.05 were considered statistically significant. Statistical analysis was performed using the SAS version 9.3 software package.
Results
Table 1 summarizes the baseline demographic characteristics of the children and their caregivers in the intervention (n=15) and control (n=27) groups. The caregivers in the two groups were comparable in terms of age, race, and marital status; however, the level of education was significantly higher for the caregivers of the children in the intervention group compared to control group (p=0.004). Specifically, the percentage of caregivers with a post-baccalaureate degree was 86.7% vs. 40.7% in the two groups. Compared to the children in the control group, those in the intervention group were less likely to be Caucasian (40% vs . 81.5%, p=0.006) and an average of 1 year older (mean age, 9.8 vs. 8.7 p=0.044).
| Characteristic | Intervention group (N=15) | Control group (N=15) |
|---|---|---|
| Caregiver characteristics | ||
| Gender, N (%) | 15(100.0%) | 26(96.3%) |
| Mother | 0(0.0%) | 1(3.7%) |
| Father | 39.1(5.4) | 41.3(4.9) |
| Age (years), Mean (SD), Marital Status, N (%) | ||
| Single | 2(13.3%) | 2(7.4%) |
| Married | 11(73.3%) | 21(77.8%) |
| Divorced | 1(6.7%) | 3(11.1%) |
| Live with a partner | 1(6.7%) | 0(0.0%) |
| Not reported | 0(0.0%) | 1(3.7%) |
| Race/Ethnicity, N (%) | ||
| Caucasian | 11(73.3%) | 23(85.2%) |
| Asian | 3(20.0%) | 2(7.4%) |
| Hispanic/Latino | 0(0.0%) | 2(7.4%) |
| Multi-ethnicity | 1(6.7%) | 0(0.0%) |
| Education, N (%) | ||
| Some college or vocational training | 0(0.0%) | 1(3.7%) |
| Two-year college degree | 0(0.0%) | 2(7.4%) |
| Fouryear college degree | 2(13.3%) | 13(48.1%) |
| Post-Baccalaureat eeducation/degree | 13(86.7%) | 11(40.7%) |
| Employment, N (%) | ||
| Fulltime | 12(80.0%) | 22(81.5%) |
| Parttime | 2(13.3%) | 4(14.8%) |
| Not employed outside of home | 1(6.7%) | 1(3.7%) |
| Child characteristics | ||
| Gender, N (%) | ||
| Female | 7(46.7%) | 18(66.7%) |
| Male | 8(53.3%) | 9(33.3%) |
| Race/Ethnicity, N (%) | ||
| Caucasian | 6(40.0%) | 22(81.5%) |
| Asian | 3(20.0%) | 2(7.4%) |
| Black | 1(6.7%) | 2(7.4%) |
| Hispanic/Latino | 1(6.7%) | 0(0.0%) |
| Multi-ethnicity | 4(26.7%) | 1(3.7%) |
| Age (years), Mean (SD) | 9.8(1.7) | 8.7(1.5) |
Table 1: Baseline demographic characteristics of the children and their caregivers, by study group.
Twenty-six of the 27 children in the control group had a follow-up assessment 4.6 months later on average (range 3.2-5.9 months). Ten (66.7%) of the 15 families in the intervention group attended 6-7 physical activity classes and 6-7 cooking classes, 3 (20.0%) attended 5 physical activity classes and 5-6 cooking classes, 1 attended just 1 physical activity class, and 1 family did not attend any classes and did not complete the follow-up assessment. Among the 15 families in the intervention group, 14 had a follow-up assessment at a mean of 5.7 months later (range 5.4-6.0 months).
The baseline and change in anthropometric measurements pre- and post-intervention are summarized in (Table 2) for the children who participated at both time points. At baseline, the children in the intervention group had a significantly greater median age- and sexspecific BMI percentile compared to the children in the control group [81.5 (IQR: 54.0, 95.0) vs. 54.0 (IQR: 24.0, 80.0), respectively, p=0.04]. The median age- and sex-specific waist circumference percentile at baseline was also higher for the intervention group, but the difference was not significantly different [77.5 (IQR: 59.4, 93.5) vs. 64.3 (IQR: 48.6, 81.9), respectively, p=0.11]. At the final assessment period, the median change (post-pre) in the age- and sex-specific BMI percentile was 0 (IQR: -2.0, 4.0) in the intervention group and -2.5 (IQR: -8.0, 2.0) in the control group and this difference was not significantly different between groups (p=0.20). Although the median change in age- and sex-specific waist circumference percentile was -2.0 (IQR: -5.0, 0.5) in the intervention group, this was not significantly different from the median change of -0.2 (IQR: -6.5, 2.7) in the control group (p=0.49).
| Measure, Median (IQR) | Intervention group (N=15) | Control group (N=15) | p-value‡ |
|---|---|---|---|
| BMI (kg/m2) | |||
| Baseline | 18.7 (16.8, 23.0) | 16.2 (15.2, 18.6) | 0.007 |
| Change | 0.5 (-0.2, 0.8) | -0.1 (-0.3, 0.4) | 0.18 |
| BMI percentile (%) | |||
| Baseline | 81.5 (54.0, 95.0) | 54.0 (24.0, 80.0) | 0.04 |
| Change | 0 (-2.0, 4.0) | -2.5 (-8.0, 2.0) | 0.2 |
| Waist circumference (cm) | |||
| Baseline | 68.9 (62.3,. 75.3) | 63.6 (58.5, 67.6) | 0.018 |
| Change | 0.3 (-1.1, 1.7) | 0.8 (-0.5, 2.0) | 0.46 |
| Waist circumference percentile (%) | |||
| Baseline | 77.5 (59.4, 93.5) | 64.3 (48.6, 81.9) | 0.11 |
| Change | -2.0 (-5.0, 0.5) | -0.2 (-6.5,2.7) | 0.49 |
| Abbreviations: BMI, body mass index; IQR, interquartile range (25th and 75thpercentiles) †Change calculated as follow-up – baseline ‡ The measures were compared between the two groups using the Wilcoxon rank sum test. |
|||
Table 2: Comparison of anthropometric measurements between the two study groups.
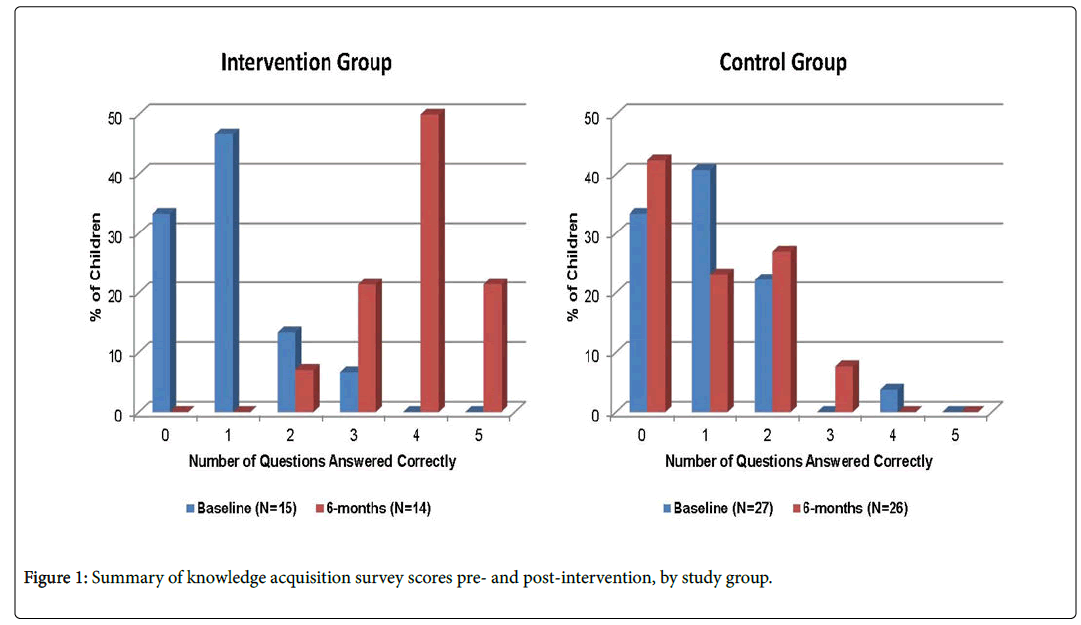
There was a large increase in the knowledge acquisition survey score in the intervention group compared to the control group (Figure 1). The median knowledge acquisition score (i.e. percent correct out of 5 questions) at baseline in both groups was 20% (intervention group IQR: 0, 20; control group IQR: 0, 30). The median follow-up score in the intervention group improved to 80% (IQR: 60, 80; p<0.001 compared to baseline), while the median follow-up score in the control group remained at 20% (IQR: 0, 40).
The changes in responses to the healthy habits questionnaire are summarized in (Table 3). There were no significant changes in 5-2-1-0 habits between the intervention and control groups. However, a higher proportion of the children in the intervention group (compared to the control group) reported an improvement in their number of servings of fruit or vegetables per day (42.9% vs. 19.2%) and an improvement in their consumption of sugary drinks (consumed less 100% juice) at follow-up (21.4% vs. 7.7%).
| Healthy Habit item | Intervention group (N=14) | Non-intervention group (N=26) | ||
|---|---|---|---|---|
| N (%) based on all N=14 | N (%) based on those who didn’t meet the target at baseline | N (%) based on all N=26 | N (%) based on those who didn’t meet the target at baseline | |
| Fruit and vegetable servings (Target=5 or more servings each day) | ||||
| Met target at both baseline and follow-up | 0 (0.0%) | - | 4 (15.4%) | - |
| Met target at baseline, but worsened at follow-up | 2 (14.3%) | - | 2 (7.7%) | - |
| Worsened at follow-up | 1 (7.1%) | 1 (8.3%) | 2 (7.7%) | 2 (10.0%) |
| No change | 5 (35.7%) | 5 (41.7%) | 13 (50.0%) | 13 (65.0%) |
| Improved at follow-up | 6 (42.9%) | 6 (50.0%) | 5 (19.2%) | 5 (25.0%) |
| Eat dinner at table with family (Target=7 or more times each week) | ||||
| Met target at both baseline and follow-up | 4 (28.6%) | - | 9 (34.6%) | - |
| Met target at baseline, but worsened at follow-up | 2 (14.3%) | - | 2 (7.7%) | - |
| Worsened at follow-up | 4 (28.6%) | 4 (50.0%) | 2 (7.7%) | 2 (13.3%) |
| No change | 2 (14.3%) | 2 (25.0%) | 4 (15.4%) | 4 (26.7%) |
| Improved at follow-up | 2 (14.3%) | 2 (25.0%) | 9 (34.6%) | 9 (60.0%) |
| Eat breakfast (Target=7 times each week) | ||||
| Met target at both baseline and follow-up | 11 (78.6%) | - | 21 (80.8%) | - |
| Met target at baseline, but worsened at follow-up | 1 (7.1%) | - | 2 (7.7%) | - |
| No change | 1 (7.1%) | 1 (50.0%) | 0 (0.0%) | 0 (0.0%) |
| Improved at follow-up | 1 (7.1%) | 1 (50.0%) | 3 (11.5%) | 3 (100.0%) |
| Eat takeout or fast food (Target=0 times each week) | ||||
| Met target at both baseline and follow-up | 1 (7.1%) | - | 6 (23.1%) | - |
| Met target at baseline, but worsened at follow-up | 0 (0.0%) | - | 2 (7.7%) | - |
| Worsened at follow-up | 1 (7.1%) | 1 (7.7%) | 0 (0.0%) | 0 (0.0%) |
| No change | 9 (64.3%) | 9 (69.2%) | 13 (50.0%) | 13 (72.2%) |
| Improved at follow-up | 3 (21.4%) | 3 (23.1%) | 5 (19.2%) | 5 (27.8%) |
| Drink 8-ounce servings of sugary drinks, including 100% juice (Target = 0 servings each week) | ||||
| Met target at both baseline and follow-up | 6 (42.9%) | - | 12 (46.2%) | - |
| Met target at baseline, but worsened at follow-up | 0 (0.0%) | - | 3 (11.5%) | - |
| Worsened at follow-up | 1 (7.1%) | 1 (12.5%) | 1 (3.8%) | 1 (9.1%) |
| No change | 4 (28.6%) | 4 (50.0%) | 8 (30.8%) | 8 (72.7%) |
| Improved at follow-up | 3 (21.4%) | 3 (37.5%) | 2 (7.7%) | 2 (18.2%) |
| Drink 8-ounce servings of sugary drinks, not including 100% juice (Target = 0 servings each week) | ||||
| Met target at both baseline and follow-up | 8 (57.1%) | - | 20 (76.9%) | - |
| Met target at baseline, but worsened at follow-up | 1 (7.1%) | - | 4 (15.4%) | - |
| No change | 1 (7.1%) | 1 (20.0%) | 0 (0.0%) | 0 (0.0%) |
| Improved at follow-up | 4 (28.6%) | 4 (80.0%) | 2 (7.7%) | 2 (100.0%) |
| Drink 8-ounce servings of water (Target =5 or more servings each week) | ||||
| Met target at both baseline and follow-up | 1 (7.1%) | - | 2 (7.7%) | - |
| Met target at baseline, but worsened at follow-up | 2 (14.3%) | - | 2 (7.7%) | - |
| Worsened at follow-up | 2 (14.3%) | 2 (18.2%) | 1 (3.8%) | 1 (4.5%) |
| No change | 3 (21.4%) | 3 (27.3%) | 9 (34.6%) | 9 (40.9%) |
| Improved at follow-up | 6 (42.9%) | 6 (54.5%) | 12 (46.2%) | 12 (54.5%) |
Table 3: Changes in responses to the healthy habits questionnaire, by study group.
Discussion
The current study aimed to assess the impact of family-centered health education incorporating 5-2-1-0 principles with cooking and physical activities. Our study findings indicate that our pilot intervention resulted in improved knowledge about healthy habits, but did not significantly impact healthy habits or BMI. Although improvement in fruit and vegetable intake and decreased consumption of sugary drinks was present, this was not statistically significant with our small sample size.
We did not observe improvements in BMI in our study, but other obesity intervention programs within the YMCA have. One YMCA study of overweight and obese children ages 6-11 years found that physical activity sessions three times per week for three months (one of these sessions each week was for families), along with 10 weekly nutrition education classes for parents using a standard Eat Smart and Move More Curriculum, resulted in significant reductions in BMI and improvements in healthy diet and activity behaviors at 3, 5, and 12 months [26]. This intervention was higher powered with a total of 42 participants and was more intensive than our current study with more frequent visits with participants; however, children were not included in the nutrition education component of the program, just the adults. Further, 44% of participants in this study had an initial BMI>99th percentile, which was higher than that of our participants.
An obesity intervention used by many YMCA sites in the United States is the evidence-based Mind, Exercise, Nutrition, Do It (MEND) program, which has been implemented to teach overweight and obese children and their families about healthy lifestyle [33-36]. This program has resulted in statistically significant reductions in waist circumference, recovery heart rate, BMI, and increased self-esteem. The curriculum is similar to 5-2-1-0, with discussion about screen time targets, limiting sugar intake, appropriate servings of foods, and activity goals. MEND is more comprehensive than our program as it teaches children and their families through local grocery store trips, nutrition label reading, and availability of bilingual materials. The MEND program also emphasizes collaboration with community partners including schools, recreation centers, churches, and clinics. The program, though, is more cost and time intensive as compared to our 5-2-1-0 family-centered obesity program.
One important goal of our obesity intervention was to make it feasible and sustainable. One major concern with grant-funded short term community-based obesity interventions is if they can be sustained in long-term in settings like the YMCA. A partnership between the Seattle Children’s Hospital and YMCA of Greater Seattle found that, even after initial grant funding ended for a program that involved 30 sessions over 18 weeks, the program could be expanded and enhanced and still demonstrate promising results in improving healthy habits and decreasing BMI [37]. This intervention was similar to ours with involvement of families, learning about healthy cooking habits, and participating in physical activity. However, to participate in this program, it was required that the participants be referred from a health care provider [37]. Involving a healthcare provider theoretically may add accountability and sustainability to the changes enforced during this program. In addition, community-based interventions for obesity should follow the Reach, Effectiveness, Adoption, Implementation and Maintenance (RE-AIM) framework [38]. Based on this framework, our pilot program had several strengths to potentially overcome barriers to success, such as including parents in skill-building sessions, using a control group, and using an evidencebased curriculum [38].
One limitation of our pilot study was the low number of children, which limited our ability to detect significant differences in health behaviors between the groups. Additionally, the participants were not randomized into study arms, making intervention vs. control groups less comparable at baseline. The higher education of parents in the intervention group may have limited the impact of the education interventions. The higher initial BMI in the intervention group may have also made it more difficult to detect BMI and waist circumference differences as compared to children in the control group. The children in the control group may have received indirect messaging about healthy habits from the YMCA HEPA standards through conversation with the camp counselors, but no intentional or direct HEPA messaging was delivered to these children.
Future obesity intervention studies should compare obesity education curriculums, ideally with randomized populations. Programs that demonstrate effectiveness could then be sustained through the YMCA. We propose further evaluation of the 5-2-1-0 curriculum in the YMCA setting to establish evidence of their effectiveness in improving BMI percentile and healthy habits over a longer duration. Further, our 5-2-1-0 intervention could be improved by increasing the frequency of intervention visits, offering bilingual materials, and tracking adoption of recommended behaviors in the home setting.
Conclusion
Our study findings demonstrated the feasibility of incorporating 5-2-1-0 education into family-based physical activity and cooking classes within the YMCA setting to improve knowledge attainment in children. This intervention shows promise in improving health habits in children and should be evaluated in future larger scale, larger duration, and comparative trials in community settings like the YMCA.
Acknowledgements
Funding for this study was supported by grants from the Mayo Clinic Center for Translational Science Activities (funded by the National Center for Advancing Translational Sciences), grant number UL1TR002377, and the Minnesota Academy of Family Physicians Foundation. We acknowledge the YMCA staff who have helped organize the project and complete study activities including Jaimie Richards and Dawn Lubahn. We thank Zumbro Lutheran Church in Rochester, MN, for hosting the cooking classes. We also thank Alicia Woodward, University of MN undergraduate student, for her help with study procedures.
References
- Hales CM, Carroll MD, Fryar CD, Ogden CL (2017) Prevalence of obesity among adults and youth: United States, 2015-2016. National Center for Health Statistics.
- Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, et al. (2005) Overweight in children and adolescents: Pathophysiology, consequences, prevention, and treatment. Circulation 111: 1999-2012.
- Lakshman R, Elks CE, Ong KK (2012) Childhood obesity. Circulation 126: 1770-1779.
- Gonzalez-Suarez C, Worley A, Somers KG, Dones V (2009) School-based interventions on childhood obesity: A meta-analysis. Am J Prev Med 37: 418-427.
- Krishnaswami J, Martinson M, Wakimoto P, Anglemeyer A (2012) Community-engaged interventions on diet, activity, and weight outcomes in U.S. schools: A systematic review. Am J Prev Med 43: 81-91.
- May C, Chai LK, Burrows T (2017) Parent, partner, co-parent or partnership? The need for clarity as family systems thinking takes hold in the quest to motivate behavioural change. Children (Basel) 4: 29.
- Rajjo T, Mohammed K, Alsawas M, Ahmed AT, Farah W, et al. (2017) Treatment of Pediatric Obesity: An Umbrella Systematic Review. J Clin Endocrinol Metab 102: 763-775.
- Saelens BE, Scholz K, Walters K, Simoni JM, Wright DR (2017) Two pilot randomized trials to examine feasibility and impact of treated parents as peer interventionists in family-based pediatric weight management. Child Obes 13: 314-323.
- Anderson JD, Newby R, Kehm R, Barland P, Hearst MO (2015) Taking steps together: A family and community-based obesity intervention for urban, multiethnic children. Health Educ Behav 42: 194-201.
- Gillman MW, Rifas-Shiman SL, Frazier AL, Rockett HR, Camargo CA, et al. (2000) Family dinner and diet quality among older children and adolescents. Arch Fam Med 9: 235-240.
- American Dietetic A (2006) Position of the American dietetic association: Nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders. J Am Diet Assoc 106: 2073-2082.
- Daniels SR, Hassink SG, Committee on Nutrition (2015) The role of the pediatrician in primary prevention of obesity. Pediatrics 136: e275-292.
- McCormick DP, Ramirez M, Caldwell S, Ripley AW, Wilkey D (2008) YMCA program for childhood obesity: A case series. Clin Pediatr (Phila) 47: 693-697.
- Dietzn WH, Belay B, Bradley D, Kahan S, Muth ND, et al. (2017) A model framework that integrates community and clinical systems for the prevention and management of obesity and other chronic diseases.
- Ling J,L Robbins BL, Martin VH (2015) Perceived parental barriers to and strategies for supporting physical activity and healthy eating among head start children. J Community Health 41: 593-602.
- Norman A, Berlin A, Sundblom E, Elinder LS, Nyberg G (2015) Stuck in a vicious circle of stress. Parental concerns and barriers to changing children's dietary and physical activity habits. Appetite 87: 137-142.
- Kitzman-Ulrich H, Wilson DK, St George SM, Lawman H, Segal M, et al. (2010) The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clin Child Fam Psychol Rev 13: 231-253.
- Nelson SA, Corbin MA, Nickols-Richardson SN (2013) A call for culinary skills education in childhood obesity-prevention interventions: Current status and peer influences. J Acad Nutr Diet 113: 1031-1036.
- Robson SM, Stough CO, Stark LJ (2016) The impact of a pilot cooking intervention for parent-child dyads on the consumption of foods prepared away from home. Appetite 99: 177-184.
- Florida Health (2000) 5-2-1-0 is a healthy lifestyle campaign to help palm beach county residents attain optimal health.
- Polacsek M, Orr J, Letourneau L, Rogers V, Holmberg R, et al. (2009) Impact of a primary care intervention on physician practice and patient and family behavior: Keep ME healthy---the maine youth overweight collaborative. Pediatrics 5: S258-266.
- Rogers VW, Motyka E (2009) 5-2-1-0 goes to school: A pilot project testing the feasibility of schools adopting and delivering healthy messages during the school day. Pediatrics 5: S272-276.
- Tucker S, Murphy J, Olsen G, Orth K, Voss J, et al. (2011) A school based community partnership for promoting healthy habits for life. J Community Health 36: 414-422.
- Tucker S, Lanningham-Foster LM (2015) Nurse-led school-based child obesity prevention. J Sch Nurs 31: 450-466.
- Lynch BA, Gentile N, Maxson J, Quigg S, Swenson L, et al. (2016) Elementary school-based obesity intervention using an educational curriculum. J Prim Care Community Health 7: 265-271.
- Schwartz RP, Vitolins MZ, Case LD, Armstrong SC, Perrin EM, et al. (2012) The YMCA healthy, fit, and strong program: A community-based, family-centered, low-cost obesity prevention/treatment pilot study. Child Obes 8: 577-582.
- Sallinen, BJ, Schaffer S, Woolford SJ (2013) In their own words: Learning from families attending a multidisciplinary pediatric weight management program at the YMCA. Childhood obesity 9: 200-207.
- Teevale T, Taufa S, Percival T (2015) Acceptability and non-compliance in a family-led weight-management programme for obese Pacific children. Public health nutrition 18: 2625-2633.
- Centers for Disease Contral and prevention (2000) Clinical growth charts.
- Sharma AK, Metzger DL, Daymont C, Hadjiyannakis S, Rodd CJ (2015) LMS tables for waist-circumference and waist-height ratio Z-scores in children aged 5-19 y in NHANES III: Association with cardio-metabolic risks. Pediatr Res 78: 23-29.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, et al. (2009) Research electronic data capture (REDCap)--A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42: 377-381.
- Butte NF, Hoelscher DM, Barlow SE, Pont S, Durand C, et al. (2017) Efficacy of a community- versus primary care-centered program for childhood obesity: TX CORD RCT. Obesity (Silver Spring) 25: 1584-1593.
- Kolotourou M, Radley D, Gammon C, Smith L, Chadwick P, et al. (2015) Long-term outcomes following the MEND 7-13 child weight management program. Child Obes 11: 325-330.
- Law C, Cole T, Cummins S, Fagg J, Morris S, et al. (2014) In A pragmatic evaluation of a family-based intervention for childhood overweight and obesity. 2014: Southampton (UK).
- Grow HM, Hencz P, Verbovski MJ, Gregerson L, Liu LL, et al. (2014) Partnering for success and sustainability in community-based child obesity intervention: Seeking to help families ACT! Fam Community Health 37: 45-59.
- Burke SM, Shapiro S, Petrella RJ, Irwin JD, Jackman M, et al. (2015) Using the RE-AIM framework to evaluate a community-based summer camp for children with obesity: A prospective feasibility study. BMC Obes 2: 21.
Citation: Gentile N, Kaufman T, Maxson J, Merten S, Price M, et al. (2018) The Effectiveness of a Family-Centered Childhood Obesity Intervention at the YMCA: A Pilot Study. J Community Med Health Educ 8: 591. DOI: 10.4172/2161-0711.1000591
Copyright: © 2018 Gentile N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5622
- [From(publication date): 0-2018 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 4882
- PDF downloads: 740