The effect of heat treatment on Meibomian Gland Dysfunction
Received: 15-Jul-2022 / Manuscript No. omoa-22- 69266 / Editor assigned: 18-Jul-2022 / PreQC No. omoa-22- 69266 / Reviewed: 01-Aug-2022 / QC No. omoa-22- 69266 / Revised: 05-Aug-2022 / Manuscript No. omoa-22- 69266 (R) / Published Date: 10-Aug-2022 DOI: 10.4172/2476-2075.1000168
Abstract
Objective: Meibomian gland dysfunction (MGD) is the most common cause of dry eye disease (DED). Though manual warm compresses (WC) are the backbone of managing MGD, poor compliance makes an office-based procedure desirable. This paper compares WC to MiBoFlo and the heated eye pad. MiBoFlo uses a thermoelectric heat pump to deliver a constant level of heat through an ultrasound gel. Digital Heat Inc developed an electric powered Heated Eye Pad (HEP) designed to warm the Meibomian sebum. The HEP resembles a spectacle frame.
Methods: Sixty subjects with MGD were randomly divided into three treatment groups after collection of baseline data. Baseline data included Ocular Surface Disease Index (OSDI), Tear Break-up time (TBUT) and Efron grading of MGD and blepharitis. The same data were collected 4 weeks after treatment. The first group was the warm compress group, the second group the MiBoFlo group and the third group the heated eye pad.
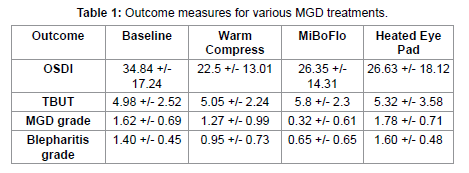
Results: Only the warm compress group showed statistically significant reduction in dry eye symptoms by OSDI (p=0.015) but the other two techniques did reduce symptoms from baseline. None of the techniques improved TBUT from baseline in a statistically significant manner. The MiBoFlo was the only treatment that resulted in a statistically significant change from baseline in Efron grading of both MGD (p=0.01) and blepharitis (p=0.01).
Conclusion: Our data suggests that MiBoFlo and the heated eye pad may be suitable alternatives to WC to achieve greater patient compliance.
Introduction
Introduction
Meibomian gland disease (MGD) is a chronic, progressive disorder. MGD is the leading cause of dry eye [1]. Warm compresses (WC) are commonly used as therapy for MGD as well as several other conditions of the eyelid. WCs used to heat the eyelids leads to softening of the waxy meibum. Partially melting the meibum obstructing the meibomian glands will make the meibum more fluid so it will blend into the tear film retarding tear evaporation. Dr. Korb and colleagues showed significant improvement in tear film lipid layer thickness following treatment with warm compresses in a series of 20 patients with MGD [2]. There is little controversy in using WCs to manage conditions like MGD and evaporative dry eye.
MGD is a chronic condition and therefore requires ongoing management. While the utility of WC maybe obvious for MGD, most patients performing WCs find themselves apathetic since the therapeutic efficacy of conventional WC is variable and this treatment must be continued over a prolonged period to achieve satisfactory reduction of symptoms. Due to these reasons, patients often discontinue treatment. Therefore, a more convenient method of performing warm compression is necessary to improve patient compliance [3].
LipiFlow (vectored thermal pulsation) is a treatment device specifically designed for effectively removing blockages from the meibomian glands. Despite the effectiveness of LipiFlow in treating MGD, it may be cost prohibitive in many cases for patients [4]. MiBoFlo Thermoflo (MiBo Medical Group, Dallas, TX, USA) was developed as a less costly alternative to the LipiFlow. MiBoFlo does not heat the inside of the eyelid. MiBoFlo uses a thermoelectric heat pump to deliver a constant level of heat through an ultrasound gel. Gentle manual pressure is applied to the anterior surface of the eyelid by the tip of the hand piece, which is maintained at 108° Fahrenheit. In contrast to LipiFlow, both the pressure and the heat applied to the lids may be partially transmitted to the globe and cornea. This procedure takes 5 minutes per eye, may be repeated, and could be used to treat MGD. A series of 3 treatments with MiBoFlo are recommended by the manufacturer [5]. Digital Heat Inc developed a powered Heated Eye Pad (HEP) designed to warm the Meibomian sebum. The HEP resembles a spectacle frame and delivers 40° Centigrade heat to the external eyelids. The present study compares the efficacy of two inoffice devices (MiBoFlo and HEP) to WCs for the treatment of MGD.
Material and Methods
This study was approved by the Institutional Review Board of the University of the Incarnate Word, San Antonio, Texas. Informed consent was obtained from all study subjects prior to the commencement of the study.
Sixty subjects with MGD confirmed by eye exam were enrolled. They were randomly divided into three treatment groups after collection of baseline data. Baseline data included the Ocular Surface Disease Index (OSDI) [6], tear break-up time (TBUT) and evaluation of MGD and blepharitis based on the Efron scale [7]. The first group was the warm compress group. This group was supplied with a washcloth and instructed to warm the washcloth and apply it to the eyes for about 30 seconds twice daily for 4 weeks. The second group, the MiBoFlo group had a small amount of ultrasound gel applied to the instrument's heated tip prior to gently massaging the outer skin of the upper and lower eyelids for a period of 12 minutes, as per the recommendation of the manufacturer. The patient's eyes remained closed throughout the treatment period. They received this treatment only once before they were assessed 4 weeks later. The last group, the heated eye pad group wore the device for 10 minutes at first visit baseline and returned for another 10-minute treatment 2 weeks later. Four weeks after treatment the same test used at baseline was repeated. Data was analyzed by ANOVA.
Results
[Table 1]: Lists the results of this study. Only the warm compress showed statistically significant reduction in dry eye symptoms by OSDI (p=0.015) but the other two techniques did reduce symptoms from baseline. None of the techniques improved TBUT from baseline in a statistically significant manner. The MiBoFlo was the only treatment that resulted in a statistically significant change from baseline in both MGD (p=0.01) and blepharitis (p=0.01) grades. The improvement in MGD grading was also statistically different (p=0.01) from both the warm compresses and heated eye pad. The improvement in blepharitis grading was not statistically different from the warm compresses but was statistically different than the heated eye pad (p=0.01).
Discussion
The warm compress was the only treatment to result in a statistically significant reduction in dry eye symptoms. We suspect this could be the result of the treatment being used twice daily rather the once or twice in 4 weeks like the other treatments. The symptom improvement data is consistent with Sim et al that found lid warming improved symptoms by 50% [8]. Although all three treatments reduced dry eye symptoms the tear breakup time was not significantly improved by any of three treatments. This could reflect the observation by Murakami et al who reported that not all WCs are equally effective [9]. They suggest the efficacy of heat retention and heat transference to lid structures accounts for this WC variability. It is worth noting that it takes at least 4 minutes of treatment with warm compresses is required to achieve an eyelid temperature of 40°Centigrade to cause the meibum to melt [10]. It is likely the warm compresses, heated eye pad and the MiBoFlo did not achieve this temperature for the desired time.
The MiBoFlo was the only treatment that changed the signs of blepharitis and MGD. The major difference between the treatments tested was MiBoFlo employs an ocular surface massage while the heat is applied. This is most likely reason that MiBoFlo resulted in significant improvement of the signs of blepharitis and MGD. Pult found no significant changes were observed in ocular signs after treatment with warm compresses [11]. Blackie et al showed that WC used for lid warming, even when only minimal contact pressure is applied, also transfers ksignificant heat to the cornea and may risk corneal deformation [12]. Corneal temperatures reach a peak temperature after about 8 minutes of WC application. Based on the association between keratoconus and rubbing-related corneal trauma, keratoconus patients with MGD should exercise caution when performing treatments involving WC and massage to avoid mechanical trauma to the cornea. In conclusion, warmth-based treatments offer value in the management of MGD. Our data suggests that MiBoFlo and the heated eye pad may be suitable alternatives to WC to achieve greater patient compliance. Practitioners and patients have choices in this modality of MGD management.
Acknowledgments
The study was partially funded by a Faculty Research Development Grant awarded to the first author (SN) by the University of the Incarnate Word Rosenberg School of Optometry, San Antonio, Texas, USA.
Disclosures
The authors of this study do not have any conflicts of interest in this work.
References
- Nichols KK, Foulks GN, Bron AJ, Glasgow BJ, Dogru M et al. (2011) The International Workshop on Meibomian Gland Dysfunction: Executive Summary. Invest Ophthalmol Vis Sci. 52: 1922-1929.
- Olson MC, Korb DR, Greiner JV (2003) Increase in tear film lipid layer thickness following treatment with warm compresses in patients with meibomian gland dysfunction. Eye Contact Lens. 29: 96-99.
- Goto E, Monden Y, Takano Y, Mori A, Shimmura S et al. (2002) Treatment of non-inflamed obstructive meibomian gland dysfunction by an infrared warm compression device. Br J Ophthalmol 86: 1403-1407.
- Greiner JV (2013) Long-term (12-month) improvement in meibomian gland functions and reduced dry eye symptoms with a single thermal pulsation treatment. Clin Exp Ophthalmol. 41: 524–530.
- Thode AR, Latkany RA (2015) Current and Emerging Therapeutic Strategies for the Treatment of Meibomian Gland Dysfunction (MGD). Drugs 75: 1177–1185.
- Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL (2000). Reliability and Validity of the Ocular Surface Disease Index. Arch Ophthalmol. 118: 615-621.
- Efron,N (2018) Contact Lens Complications. 4th edn Elsevier, USA.
- Sim HS, Petznick A, Barbier S, Tan JH, Acharya UR et al. (2014) Randomized, Controlled Treatment Trial of Eyelid-Warming Therapies in Meibomian Gland Dysfunction. Ophthalmol Ther 3: 37–48.
- Murakami DK, Blackie CA, Korb DR (2015) All Warm Compresses Are Not Equally Efficacious. Optom Vis Sci 92: 327- 333.
- Blackie CA, Solomon JD, Greiner JV, Holmes M, Korb DR (2008) Inner eyelid surface temperature as a function of warm compress methodology. Optom Vis Sci. 85: 675–683.
- Pult H, Riede-Pult BH, Purslow C (2012) A Comparison of an Eyelid-Warming Device to Traditional Compress Therapy. Optom Vis Sci. 89: 1035–1041.
- Blackie CA, McMonnies CW, Korb DR (2013) Warm Compresses and the Risks of Elevated Corneal Temperature with Massage. Cornea 32: 146–149.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Narayanan S, Fortenberry S, Kasraie N, Connor CG (2022) The effect of heat treatment on Meibomian Gland Dysfunction. Optom Open Access 7: 168. DOI: 10.4172/2476-2075.1000168
Copyright: © 2022 Narayanan S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2516
- [From(publication date): 0-2022 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 2102
- PDF downloads: 414