The Dynamic Changes of Paradoxical IRIS of an AIDS Patient with Cytomegalovirus Encephalitis and Pulmonary Tuberculosis: A Case Report
Received: 16-May-2023 / Manuscript No. JIDT-23-98959 / Editor assigned: 18-May-2023 / PreQC No. JIDT-23-98959(PQ) / Reviewed: 01-Jun-2023 / QC No. JIDT-23-98959 / Revised: 08-Jun-2023 / Manuscript No. JIDT-23-98959(R) / Published Date: 15-Jun-2023 DOI: 10.4172/2332-0877.S3.004
Abstract
Background: This study describes an AIDS patient with CNS tuberculosis and cytomegalovirus infection that experienced IRIS associated with cytomegalovirus encephalitis and PTB while receiving ART.
Case presentation: A 59-year-old male was referred to our hospital with a fever of unknown origin and paroxysmal cough as the main symptoms for three days. CSF examination revealed a cytomegaloviral load of 3.4 ×103 copies/mL and a positive MTB recombination test. CSF gene X-pert MTB/RIF test revealed MTB infection without rifampicin resistance. Anti-tuberculosis treatment and anti-cytomegalovirus therapy were administered, improving clinical and laboratory abnormalities. ART was initiated 24 days after starting anti-tuberculosis treatment, with a baseline CD4+ T lymphocyte count of 70 cells/μL. Clinical symptoms reappeared on day 33 after starting ART. Paradoxical IRIS was considered the most likely diagnosis. After adding dexamethasone to continue antituberculosis and anti-CMV therapy, the patient’s symptoms disappeared, and imaging showed a reduction in scope. There was no recurrence of clinical symptoms during a two-year outpatient follow-up.
Conclusion: It is crucial to consider the emergence of multiple infections and the associated IRIS in AIDS. Once IRIS manifests, proper diagnosis and continual treatment are imperative for patient recovery.
Keywords: Immune reconstitution inflammatory syndrome; Cytomegalovirus; Tuberculosis; AIDS
Abbreviations
IRIS: Immune Reconstitution Inflammatory Syndrome; ART: Antiretroviral Therapy; CMV: Cytomegalovirus; PTB: Pulmonary Tuberculosis; HIV: Human Immunodeficiency Virus; CSF: Cerebrospinal Fluid; MTB: Mycobacterium Tuberculosis; CNS: Central Nervous System
Introduction
AIDS patients with low CD4+ T-cell counts are susceptible to immunological reconstitution inflammatory syndrome (IRIS) within the first three months of initiating antiretroviral therapy (ART) [1]. There are two types of IRIS: paradoxical IRIS, characterized by the recurrence or significant worsening of a pre-existing opportunistic infection and its symptoms, and unmasked IRIS, defined as the discovery of a previously unrecognized latent infection [2].
The most frequent clinical agents of IRIS are tuberculosis and Cytomegalovirus (CMV) [3]. The gastrointestinal tract and eyes are particularly vulnerable to CMV infection [4,5]. There are few reports of CMV involving the brain and causing the corresponding IRIS. We present the dynamic changes in paradoxical IRIS in an AIDS patient with CMV encephalitis and Pulmonary Tuberculosis (PTB).
Case Presentation
HSV A 59-year-old man with an unexplained fever was admitted to the hospital, presenting with dizziness, fatigue, loss of appetite, fear of cold, afternoon fever, occasional babbling during fever, paroxysmal cough, and cough with a small amount of white sputum. Upon admission, his vital signs were as follows: 92 beats/min, 39°C axillary temperature, 132/91 mmHg blood pressure, and 22 breaths per minute. He tested positive for Human Immunodeficiency Virus (HIV) in an outpatient setting but did not undergo HIV-Viral load testing.
Cerebrospinal fluid (CSF) examination was conducted after admission, revealing CSF protein quantification of 2360 mg/L, blood glucose 1.58 mmol/L, lactate dehydrogenase 52 U/L, CMV viral load 3.4 × 103 copies/mL, and positive CSF mycobacterium tuberculosis (MTB) recombination assay. All other CSF tests were negative. Brain MRI showed an aberrant signal in the knee of the corpus callosum with low T1WI, high T2WI, high FLAIR, high DWI, and low ADC signals, and no enhancement was observed. Chest CT depicted few lung lesions, enlarged mediastinal lymph nodes, and a small amount of bilateral pleural effusion.
The patient received antituberculosis treatment with isoniazid, pyrazinamide, levofloxacin, and amikacin, and the chest CT revealed a reduction in the pulmonary lesions and pleural effusion 15 days later. The CMV viral load in CSF increased to 24.7 × 103 copies/mL, prompting intravenous injection of 0.25 g/dose of ganciclovir twice daily for 11 days. After nine days of treatment, CMV load in CSF decreased to 4.89 × 103 copies/mL, and clinical symptoms disappeared. The patient was discharged after 26 days of antituberculosis treatment and 11 days of anti-CMV treatment, followed by antiviral therapy (ART) in an outpatient setting with tenofovir fumarate, lamivudine, and efavirenz with baseline CD4+ T lymphocytes of 70 cells/μL. The patient continued antituberculosis treatment and took oral ganciclovir 1 g/dose three times daily for two weeks.
On day 33 after starting ART, the patient was readmitted to the hospital due to chills, fever, cough, sputum, low fever, cough, a small amount of white mucus sputum, loss of appetite, nausea, vomiting, fatigue, and numbness in both legs for three days. CMV viral load in CSF was 22.6 × 103 copies/mL, and MTB recombination assay was negative. CD4+T lymphocyte count increased to 105 cells/μL. MRI revealed an enlarged lesion in the corpus callosum of the knee and a decreased diffusion-weighted image signal. Compared to the previous CT of the chest, lung segment lesions were larger. The patient reported continuing medication after discharge. No further infections were observed during hospitalization. Paradoxical IRIS was considered the most likely diagnosis. The original anti-tuberculosis treatment was supplemented with a small amount of dexamethasone. Five days later, CMV viral load dropped to 4.37 × 103 copies/mL. The patient did not cooperate with treatment, CMV viral load increased to 22.7 × 103 copies/mL 10 days later, and the patient was discharged automatically.
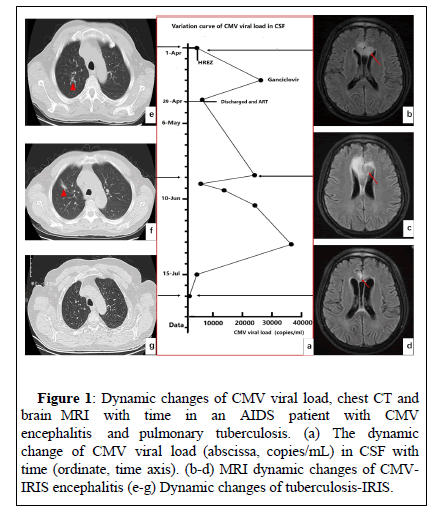
The patient was hospitalized for a third time 19 days later with a CMV viral load of 35 × 103 copies/mL. The CMV viral load was reduced to 0.54 × 103 copies/mL after receiving anti-tuberculosis medication and continuing ganciclovir treatment for 24 days. MRI and chest CT scans showed fewer brain and chest lesions than before, and HIV-RNA viral load was below 20 copies/μL. Figures 1a-1g displays the dynamic changes in CMV viral load, chest CT, and brain MRI with time. The two-year outpatient follow-up did not depict any consequences or recurrence of CMV infection.
Figure 1: Dynamic changes of CMV viral load, chest CT and brain MRI with time in an AIDS patient with CMV encephalitis and pulmonary tuberculosis. (a) The dynamic change of CMV viral load (abscissa, copies/mL) in CSF with time (ordinate, time axis). (b-d) MRI dynamic changes of CMVIRIS encephalitis (e-g) Dynamic changes of tuberculosis-IRIS.
Results and Discussion
This study presents the dynamic changes in paradoxical IRIS in an AIDS patient with CMV encephalitis and PTB. Despite the absence of a specific diagnostic basis, paradoxical IRIS was established by comprehensively considering clinical symptoms, laboratory tests, and imaging findings during treatment according to the criteria published by the International Network for the Study of HIV-associated IRIS (INSHI) [6].
Recent research indicates that CMV infection increases the likelihood of developing tuberculosis, especially those with latent tuberculosis infection [7,8]. The primary diagnostic criteria for opportunistic infections of central nervous system (CNS) include clinical features, CSF, radiographic characteristics, and temporal evolution [9]. Quantitative PCR results can also help assess disease severity and monitor response to antiviral therapy [9]. In our case, the patient had an elevated CMV viral load and positive MTB recombination assay, indicating a combined CNS tuberculosis and CMV infection. Anderson, et al., reported that typical MRI findings of AIDS-associated CMV encephalitis revealed a slightly low signal on T1WI, a high signal on T2WI and FLAIR, a slightly high signal on DWI, and a low signal on ADC [10]. Restricted diffusion MRI lesions are one of the specific manifestations of CMV encephalitis and may persist for a long time [11-13]. Dynamic enhancement scans of the lesion exhibited minimal to no enhancement and revealed tiny internal vessels, distinguishing it from the perifocal edema and ring-like enhancement of tuberculous encephalitis [14]. Vascular infarction, regarded as a type of CMV-associated IRIS, is a rare clinical and radiological presentation of CNS CMV infection [15,16]. Our case began with a similar MRI appearance to acute cerebral infarction but lacked the symptoms of cerebral infarction. The viral load decreased, and clinical symptoms improved after administering ganciclovir, indicating an intracranial lesion of CMV encephalitis.
The patient reappeared 33 days after ART with clinical signs and elevated CD4+ T-cell counts but with an increased CMV viral load and intracranial and pulmonary lesions. Clinical deterioration due to drug resistance and new infections was excluded.
Conclusion
The patient experienced a significant treatment effect by adding a small amount of dexamethasone. There was no recurrence after a 2- year follow-up, confirming IRIS diagnosis. This is crucial for IRIS diagnosis, demonstrating that a better curative effect can be obtained without excessive additional treatment, thus reducing patient burden.
Clinical manifestations, CSF, radiological features, and temporal evolution contribute to CNS diagnosis and the possible presence of IRIS. It is crucial to be aware of the emergence of multiple infections and the associated IRIS in AIDS patients.
Acknowledgements
This material is the result of research funded by the University of the Incarnate Word School of Osteopathic Medicine Office of Research and Innovation.
Disclosures
All authors declare no conflict of interest.
References
- Eleftheriotis G, Skopelitis E (2022) Concurrence of cat-scratch disease and paradoxical tuberculosis-IRIS lymphadenopathy: A case report. BMC Infect Dis 22: 213.
- Ramos De Sá NB, Ribeiro-alves M, Da Silva TP, Pilotto JH, Rolla VC, et al. (2020) Clinical and genetic markers associated with tuberculosis, HIV-1 infection, and TB/HIV-immune reconstitution inflammatory syndrome outcomes. BMC Infect Dis 20: 59.
[Crossref] [Google Scholar] [PubMed]
- Novak RM, Richardson JT, Buchacz K, Chmiel JS, Durham MD, et al. (2012) Immune reconstitution inflammatory syndrome: incidence and implications for mortality. AIDS 26: 721-730.
[Crossref] [Google Scholar] [PubMed]
- Belo F, Mendes I, Calha M, Mendonca C (2012) Cytomegalovirus encephalitis in an immunocompetent child: a sceptic diagnosis. BMJ Case Rep 2012.
[Crossref] [Google Scholar] [PubMed]
- Ude IN, Yeh S, Shantha JG (2022) Cytomegalovirus retinitis in the highly active anti-retroviral therapy era. Ann Eye Sci 7.
[Crossref] [Google Scholar] [PubMed]
- Reddy T, Bajwa R, Burke A (2022) The IRIS paradox: Imaging findings in a case of PJP-IRIS. Respirol Case Rep 10: e01014.
[Crossref] [Google Scholar] [PubMed]
- Stockdale L, Nash S, Farmer R, Raynes J, Mallikaarjun S, Newton R, et al. (2020) Cytomegalovirus antibody responses associated with increased risk of tuberculosis disease in ugandan adults. J Infect Dis 221: 1127-1134.
[Crossref] [Google Scholar] [PubMed]
- Heijden YF, Zhang B, Chougnet CA, Huaman MA (2021) Cytomegalovirus infection is associated with increased prevalence of latent tuberculosis infection. Open Forum Infect Dis 8: ofab539.
[Crossref] [Google Scholar] [PubMed]
- Tan IL, Smith BR, Von Geldern G, Mateen FJ, McArthur JC (2012) HIV-associated opportunistic infections of the CNS. Lancet Neurol 11: 605-617.
[Crossref] [Google Scholar] [PubMed]
- Anderson AM, Mosunjac MB, Corey AS, et al. (2011) Simultaneous typical and extraordinary imaging findings of AIDS-associated cytomegalovirus encephalitis. J Neurol Sci 307: 174-177.
[Crossref] [Google Scholar] [PubMed]
- Cho SM, Mays M (2018) Restricted diffusion MRI lesions in HIV-associated CMV encephalitis. Neurohospitalist 8: Np3-Np4.
[Crossref] [Google Scholar] [PubMed]
- Renard T, Daumas-Duport B, Auffray-Calvier E, Bourcier R, Desal H (2016) Cytomegalovirus encephalitis: Undescribed diffusion-weighted imaging characteristics. Original aspects of cases extracted from a retrospective study, and from literature review. J Neuroradiol 43: 371-377.
[Crossref] [Google Scholar] [PubMed]
- Li D, Van Gaal S (2018) Cytomegalovirus encephalitis radiographically mimicking lateral medullary stroke. Neurol Clin Pract 8: e37-e39.
[Crossref] [Google Scholar] [PubMed]
- Krishnaraj R, Chokkalingam C, Krishnarajasekhar OR, Narayanan R, Sadagopan K, et al. (2014) Recurrent immune reconstitution inflammatory syndrome of tuberculous brain infection in people living with HIV/AIDS: A case report. J Int Assoc Provid AIDS Care 13: 15-17.
[Crossref] [Google Scholar] [PubMed]
- Anderson AM, Fountain JA, Green SB, et al. Human immunodeficiency virus-associated cytomegalovirus infection with multiple small vessel cerebral infarcts in the setting of early immune reconstitution. J Neurovirol 16: 179-184. [Crossref]
[Google Scholar] [PubMed]
- Kieburtz KD, Eskin TA, Ketonen L, et al. (1993) Opportunistic cerebral vasculopathy and stroke in patients with the acquired immunodeficiency syndrome. Arch Neurol 50: 430-432.
[Crossref] [Google Scholar] [PubMed]
Citation: Song S, Jiang C, Gan D, Lu Y (2023) The Dynamic Changes of Paradoxical IRIS of an AIDS Patient with Cytomegalovirus Encephalitis and Pulmonary Tuberculosis: A Case Report. J Infect Dis Ther S3: 004. DOI: 10.4172/2332-0877.S3.004
Copyright: © 2023 Song S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1042
- [From(publication date): 0-2023 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 821
- PDF downloads: 221