Case Report Open Access
The Duplicated Pancreas: Imaging Evaluation of a Rare Anomaly Presenting as Acute Pancreatitis
Rohr A1*, Best S1, Sugumar A2 and Ash A11Department of Radiology, University of Kansas Medical Center, Kansas City, Kansas, USA
2Department of Gastroenterology, University of Kansas Medical Center, Kansas City, Kansas, USA
- Corresponding Author:
- Aaron Rohr
Department of Radiology
University of Kansas Medical Center
3901 Rainbow Boulevard, Mail Stop 4032
Kansas City, Kansas 66160, Kansa, USA
Tel: 316-258-9505
Fax: 913-945-6470
E-mail: arohr@kumc.edu
Received Date: November 01, 2016; Accepted Date: November 21, 2016; Published Date: November 25, 2016
Citation: Rohr A, Best S, Sugumar A, Ash A (2016) The Duplicated Pancreas: Imaging Evaluation of a Rare Anomaly Presenting as Acute Pancreatitis. OMICS J Radiol 5:240. doi: 10.4172/2167-7964.1000240
Copyright: © 2016 Rohr A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
There are multiple variants of normal anatomy involving multiple organ systems, many of which are well documented throughout the medical community. Specifically, the pancreas can demonstrate a wide range of variants that include divisum, ectopic tissue, annular pancreas, ductal variation, and pancreatic rests. However, upon literature review, a complete duplication of the pancreas resulting in two separate pancreases is rarely documented. This case provides an interesting diagnosis of two individual pancreases in a patient whom initially presented clinically with recurrent bouts of acute pancreatitis and weight loss status post prior cholecystectomy. Dedicated CT, MRI, MRCP, and endoscopic ultrasound were able to delineate pertinent anatomy and acute findings. The resultant patient course is difficult to predict secondary to limited documentation of duplicated pancreases in the medical literature. Additionally, the case helps provide insight into complications that may arise from this embryologic anomaly, the best imaging techniques for evaluation, and future management of this patient.
Keywords
Duplicated pancreas; Anomaly; Variant; Pancreatitis
Case
Throughout the history of medicine, and specifically radiology, there is documentation of extensive anatomical variations involving multiple organ systems, which range from person to person. In regard to the pancreas, there are numerous descriptions of variant anatomy that include divisum, ectopic tissue, annular pancreas, ductal variations, and pancreatic rests [1-3]. These anatomical variants are largely related to embryologic development and associated congenital anomalies [3,4]. Additionally, certain malformations such as a circumportal pancreas can result in vascular manifestations including encasement of the portal vein or superior mesenteric vein [5]. Postsurgical, post-traumatic, and post-inflammatory conditions are additional etiologies that can result in varying anatomy of the pancreas [6,7]. Many of these anomalies have been described, though current literature briefly expands upon a complete duplication of the pancreatic system, resulting in two fully developed, adjacent pancreases.
This case presents a 26 year old female initially presented with upper abdominal pain during her first pregnancy and was diagnosed with acute pancreatitis by laboratory evaluation. Two months following delivery of this first pregnancy, the patient again presented with upper abdominal pain and was again diagnosed with acute pancreatitis by laboratory evaluation. Lipases at these times were greater than 10,000 U/L on one occasion and 2,117 U/L on another. It wasn’t until two years later that the patient presented with her third episode of acute pancreatitis that imaging was performed.
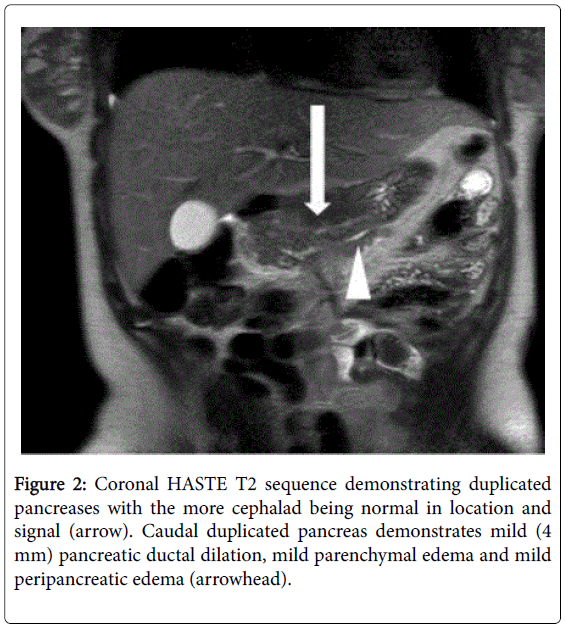
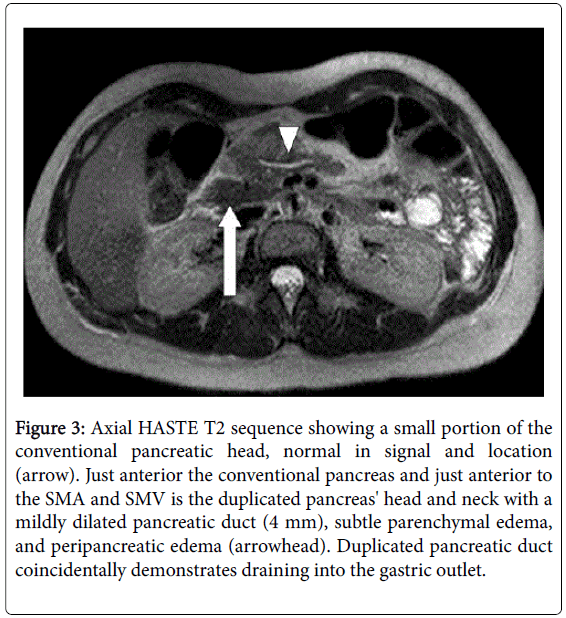
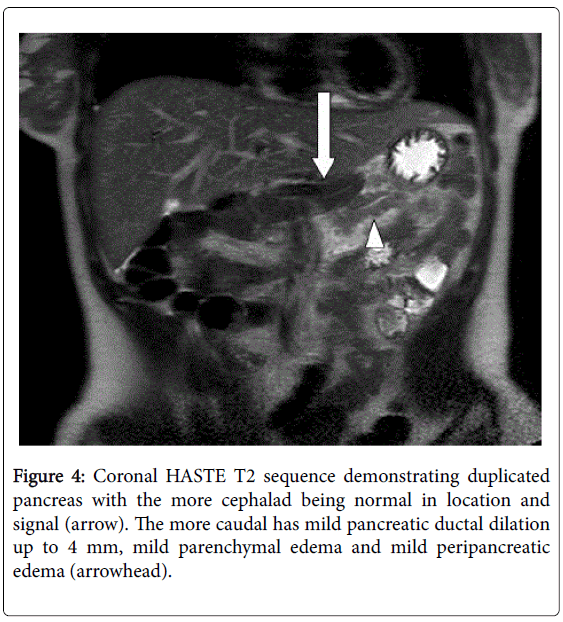
The initial imaging evaluation during this third acute episode was by CT and then subsequent MRI/MRCP. The studies demonstrated two separate pancreases, as well as edema within and adjacent to the more anterior pancreas, consistent with acute pancreatitis. The second, more anterior pancreas appears to drain to the gastric outlet with its main pancreatic duct mildly dilated up to 4 mm. The patient was also imaged two years later during another acute episode of pancreatitis that included a CT, MRI/MRCP, and an endoscopic ultrasound.
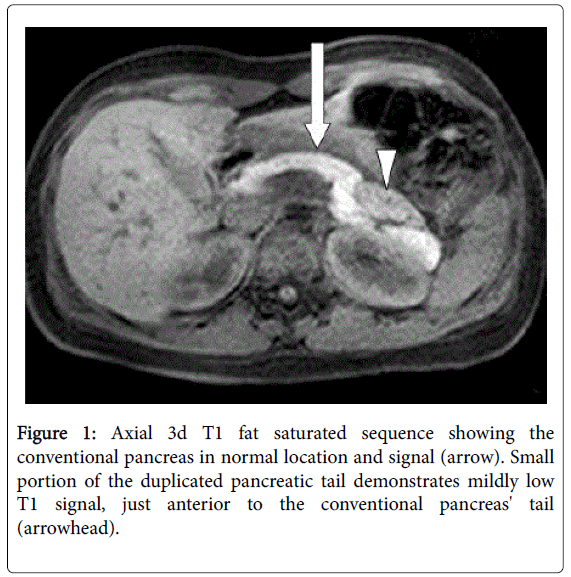
The CT and MRI/MRCP were first performed, showing acute pancreatitis of the more anterior pancreas, as well as development of a small adjacent pseudocyst. An endoscopic ultrasound was performed with the report describing heterogeneity of the pancreatic parenchyma, consistent with acute pancreatitis. However, the report did not describe the two separate pancreases. Also, the pancreatic duct was not able to be evaluated or cannulated on that exam. The duplicated pancreases are best demonstrated on MRI findings from the aforementioned two year intervals (Figures 1-4).
Figure 3: Axial HASTE T2 sequence showing a small portion of the conventional pancreatic head, normal in signal and location (arrow). Just anterior the conventional pancreas and just anterior to the SMA and SMV is the duplicated pancreas' head and neck with a mildly dilated pancreatic duct (4 mm), subtle parenchymal edema, and peripancreatic edema (arrowhead). Duplicated pancreatic duct coincidentally demonstrates draining into the gastric outlet.
Discussion
This case study elucidates an incompletely understood pancreatic anomaly manifesting as complete pancreatic duplication. The primary diagnosis of recurring acute pancreatitis is interesting, and provides a vast differential for underlying etiology, even in the setting of dual pancreases. This variant anatomy is the presumable leading consideration for etiology of pancreatitis, which may result from incomplete pancreatic ductal draining or redundant pancreatic ductal system. However, various other hypotheses may attribute to the onset of pancreatitis. Moreover, this case provides inquiry to what radiologic studies are the most appropriate to evaluate this abnormality, and what imaging would be most suitable for continued follow-up. With regard to evaluation of the abnormality; pre- and post-contrast T1-weighted MRI images, as well as axial and coronal T2 single shot fast spin echo (SSFSE) with or without fat saturation images would provide appropriate anatomical evaluation of the duplicated pancreas. If an experienced abdominal radiologist is available at that institution, heavily T2-weighted magnetic resonance cholangiopancreatography (MRCP) images with attention to the pancreatic duct could also be obtained in order to detail the ductal anatomy. After the diagnosis is made, follow-up imaging would largely be unnecessary in an asymptomatic patient, as the etiology is likely due to congenital variance. However, in the setting of acute abdominal pain, a routine Computed Tomography (CT) of the abdomen and pelvis should suffice for evaluation of acute pancreatitis and its possible manifestations.
Patient management is not limited to radiologic monitoring, and the ensuing medical direction is a very convoluted picture. Laboratory monitoring is essential for acute bouts of pancreatitis, and the lab tests would presumably follow in a similar fashion as those of general pancreatitis. Whether or not tissue sampling is required remains unknown. Also, any additional risk for development of neoplastic disease is not clearly defined in this setting. Surgery is well documented as added value for correction of pancreas anomalies [5,6], and surgical correction is a consideration in this case. Though, no current literature is available to determine appropriateness. Questions remain with regard to patient management, but this case provides definitive radiographic findings of a previously unknown pancreatic anomaly and some of the associated complications.
This case report elaborates on the unusual anatomic variant of a duplicated pancreas presenting as acute pancreatitis, as well as exploring techniques for evaluation and future management of this condition.
References
- Yu J, Turner MA, Fulcher AS, Halvorsen RA (2006) Congenital anomalies and normal variants of the pancreaticobiliary tract and the pancreas in adults: part 2, Pancreatic duct and pancreas. Am J Roentgenol 187: 1544-1553.
- Adda G, Hannoun L, Loygue J (1984) Development of the human pancreas: variations and pathology: A tentative classification. AnatomiaClinica 5: 275-283.
- Yuan Z, Chen J, Zheng Q, Huang XY, Yang Z, et al. (2009) Heterotopic pancreas in the gastrointestinal tract. World J Gastroenterol 15: 3701-3703.
- Borghei P, Sokhandon F, Shirkhoda A, Morgan DE (2013) Anomalies, anatomic variants, and sources of diagnostic pitfalls in pancreatic imaging. Radiology 266: 28-36.
- Connelly TM, Sakala M, Tappouni R (2015) Circumportal pancreas: a review of the literature and image findings. SurgRadiolAnat 37: 431-437.
- Weledji EP, Ngowe MN, Mokake DM, Verla V (2015) Post-traumatic pancreatic pseudocyst managed by Roux-en-Y drainage. J Surg Case Rep2015: rjv094.
- Freeny PC (1990) Imaging of chronic pancreatitis: A synopsis. In Chronic Pancreatitis, Springer Berlin Heidelberg, pp: 330-341.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 13637
- [From(publication date):
December-2016 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 12687
- PDF downloads : 950