The Dilemma of Rhinitis
Received: 28-Jun-2016 / Accepted Date: 05-Jul-2016 / Published Date: 12-Jul-2016 DOI: 10.4172/2161-119X.1000e112
253853Introduction
Rhinitis is a widespread condition that causes significant morbidity worldwide and profoundly affects patients' quality of life. Given its prevalence and relative chronicity, the economic impact of rhinitis is significant. It has been demonstrated that allergic rhinitis is a strong risk factor for the onset of asthma in adults. This led to the development of the United Airways Concept [1]. Despite this prevalence, rhinitis is still an ill-defined disease that is associated with many controversial entities and few proven facts. The term “rhinitis’’ is, in itself, controversial as it implies an inflammatory disease of the nasal mucous membrane. Clinical experience however has showed that the common symptoms of itching, sneezing, discharge, and blockage may exist without actual inflammation. Therefore, strictly speaking, the term “rhinopathy” is a more correct term, but it is rarely used [2].
There is no universally accepted system for the definition, classification, or the terminology of rhinitis. Use of the different terms for the same disease and of the same term for different diseases has, in part, made reports of rhinitis confusing to read and difficult to compare. The issue was further complicated by the introduction of the term “rhinosinusitis”, since the sinuses may be involved in many, but not all, cases of rhinitis.
Rhinitis is usually, and broadly, classified into infectious and noninfectious categories. The infectious category is the better-defined type, but may occasionally be confused with non-infectious rhinitis. As a matter of clinical routine, the diagnosis of viral or bacterial rhinitis is not based on identification of specific organisms. The diagnosis is usually based on clinical grounds including the duration of the disease and the presence of purulent discharge.
Non-infectious rhinitis including allergic (AR) non-allergic (NAR), occupational, hormonal, drug-induced, and some other less common types. The term “vasomotor” rhinitis (VMR) is often used for noninfectious, non-allergic rhinitis, in spite of lack of existing vasomotor pathogenesis in some cases [3]. Allergic and non-allergic rhinitis are the two bigger groups of non-infectious rhinitis, and the distinction between allergic rhinitis and allergic-like non-allergic rhinitis is not always clinically easy. Generally speaking allergic rhinitis has a younger age of onset, a more positive family history, and a higher incidence of ocular symptoms [4]. Female gender may be a risk factor for NAR [5]. Since NAR is not IgE mediated, its diagnosis is usually is based on either negative skin tests for allergens or a negative RAST test.
Allergic rhinitis is an IgE response to an antigen and occurs in genetically predisposed persons. Antigen exposure results in the production of IgE antibodies, which bind to receptor sites on circulating basophils and mast cells. With further contact and reexposure to the offensive allergen, degranulation of mast cells residing in the nasal mucosa result in a proliferation of chemical mediators including histamine, leukotrienes and prostaglandins. The appearance of acute symptoms such as sneezing, pruritus, rhinorrhea and wheezing are known as an early-phase response. Following the allergen insult, 50% of patients experience a secondary late phase reaction occurring four to eight hours later increased congestion. An increase in inflammatory cytokine cells–eosinophils, basophils, neutrophils and lymphocytes–characterizes this late phase reaction. In 2008 ARIA recommended a classification of allergic rhinitis (intermittent, persistent, mild, and moderate), and also provided guidelines for its management [6]. ARIA classification has been found to be a valid tool also in children from 6 to 12 yr old [7].
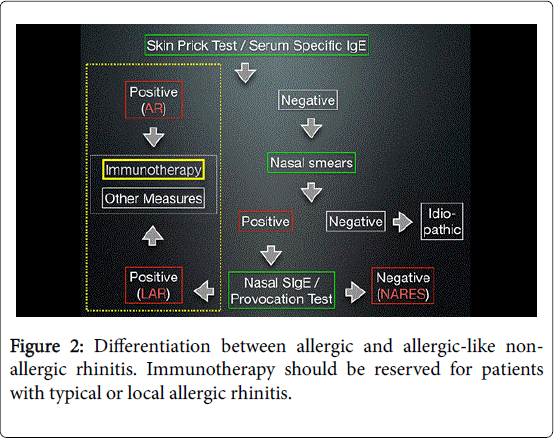
Another recently defined subtype of allergic rhinitis is “local allergic rhinitis”(LAR). LAR is defined as: rhinitis due to nasal production of specific immunoglobulins (sIgE) in the absence of atopy (negative skin prick test, negative RAST test) [8]. This is called “entopy”. LAR is frequently misdiagnosed as NAR and this may prevent the patient from benefiting from immunotherapy that can be useful for patients with LAR.
Non-allergic rhinitis (NAR) refers to a broad group of diverse nasal diseases that are not allergic in origin. Unlike allergic rhinitis, which is IgE- mediated, NAR syndromes are elicited by a variety of environmental changes. VMR symptoms typically occur in reaction to environmental triggers, which may include weather changes, cold dry air, perfumes, paint fumes or other strong odors and cigarette smoke, among others. Changes in temperature or relative humidity may also exacerbate VMR, as may alcohol, odors (such as bleach, solvents or fragrances), bright lights, spicy foods or irritants such as smoke, dust and automotive fumes. Emotional factors, including stress and sexual arousal, may also affect nasal symptoms probably due to stimulation of the autonomic nervous system [9].
Non-allergic rhinitis is usually an under-estimated entity. However, it is reported that at least half of all patients presenting with rhinitis may have a non-allergic form [10]. Most recently, a national survey of allergists conducted by the National Rhinitis Classification Task Force (NRCTF) found that a total of 57% of patients presenting with chronic rhinitis had either pure or mixed NAR. Of particular note was the finding that 44% of patients with allergic rhinitis were classified as also having some component of NAR [11].
The major type of NAR is vasomotor rhinitis (VMR), which is sometimes called perennial non-allergic rhinitis. Unfortunately, the term is frequently and erroneously used to describe entities without vasomotor pathogenesis. Settipane and Klein found that VMR affects about two-thirds of NAR patients [12]. The other important form of NAR that may mimic allergic rhinitis is non-allergic rhinitis with eosinophilia syndrome (NARES) [13]. NARES is characteristically associated with eosinophilia (>20%) in nasal smears. Generally speaking, patients with NARES have a higher tendency for nasal polyposis and aspirin sensitivity, and a better response to topical steroids and second-generation antihistamines than patients with VMR.
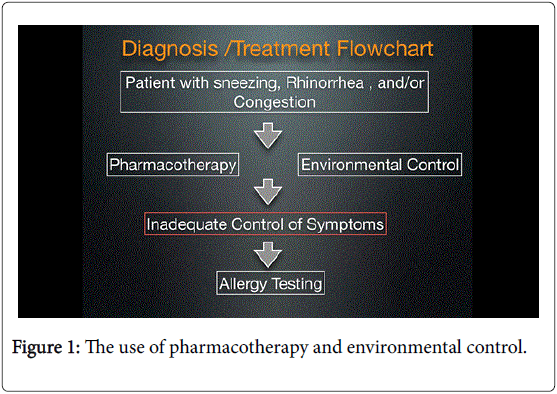
The ARIA taskforce has provided evidence-based guidelines for management of allergic rhinitis [5]. However, in practice, many clinicians empirically treat non-infectious rhinitis without paying enough attention to the differences between AR and NAR. This definitely degrades the outcome of treatment sincet research has not shown oral antihistamines to be beneficial in relieving symptoms of non-allergic rhinitis. This, also, may be the reason why only about onefourth of allergy sufferers report that their symptoms are well controlled or completely controlled [14]. The flowcharts shown in Figures 1 and 2 show a proposed strategy for management of patients of non-infectious rhinitis. This strategy, in my opinion, maximizes the outcome of treatment and, at the same time, reserves the use of immunotherapy to the patients who will actually benefit from it.
References
- BraunstahlGJ (2009) United airways concept: what does it teach us about systemic inflammation in airways disease?Proc Am ThoracSoc 6: 652-654.
- Mygind N, Naclerio R (1993) In allergic and non-allergic rhinitis: Clinical aspects. Munksgaard,Copenhagen.
- Connell JT (1983) Nasal disease: mechanisms and classification.Ann Allergy 50: 227-235.
- Togias A (1990) Age relationships and clinical features of nonallergic rhinitis [abstract]. J Allergy ClinImmunol 85: 182.
- Settipane RA, Settipane GA (2000) Nonallergic rhinitis. In: Kaliner MA, ed. Current Review of Allergic Diseases. Pa: Current Medicine Inc. Philadelphia, pp: 111-124.
- Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, et al. (2008) Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen).Allergy 63 Suppl 86: 8-160.
- Jáuregui I, Dávila I, Sastre J, Bartra J, del Cuvillo A, et al. (2011) Validation of ARIA (Allergic Rhinitis and its Impact on Asthma) classification in a pediatric population: the PEDRIAL study. Pediatr Allergy Immunol 22:388-92
- Rondón C, Canto G, Blanca M (2010) Local allergic rhinitis: a new entity, characterization and further studies.CurrOpin Allergy ClinImmunol 10: 1-7.
- Eiser N (1990) The hitch-hikers guide to nasal airway patency.Respir Med 84: 179-183.
- Dykewicz MS, Fineman S, Skoner DP, et al. (1998) Diagnosis and management of rhinitis: complete guidelines of the Joint Task Force on Practice Parameters in Allergy, Asthma and Immunology. American Academy of Allergy, Asthma and Immunology. Ann Allergy Asthma Immunol81:478- 518
- Kaliner MA, Lieberman P (2000) Incidence of allergic, nonallergic and mixed rhinitis in clinical practice. Paper presented at: Annual Meeting of the American Academy of Otolaryngology-Head and Neck Surgery Foundation.
- Settipane GA, Klein DE (1985) Non allergic rhinitis: demography of eosinophils in nasal smear, blood total eosinophil counts and IgE levels.N EnglReg Allergy Proc 6: 363-366.
- Moneret-Vautrin DA, Hsieh V, Wayoff M, Guyot JL, Mouton C, et al. (1990) Nonallergic rhinitis with eosinophilia syndrome a precursor of the triad: nasal polyposis, intrinsic asthma, and intolerance to aspirin.Ann Allergy 64: 513-518.
- Meltzer EO (1997) The prevalence and medical and economic impact of allergic rhinitis in the United States.J Allergy ClinImmunol 99: S805-828.
Citation: Elwany S (2016) The Dilemma of Rhinitis. Otolaryngol (Sunnyvale) 6:e112. DOI: 10.4172/2161-119X.1000e112
Copyright: © 2016 Elwany S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11520
- [From(publication date): 8-2016 - Jul 12, 2025]
- Breakdown by view type
- HTML page views: 10653
- PDF downloads: 867