Review Article Open Access
The Dental Surgeons in the Hospital and their Professional Areas in Brazil: Hospitalization Units, Surgical Centers and Intensive Care Units
Miranda AF*Department of Dentistry for Special Patients and Geriatric Dentistry, Catholic University of Brasília, Brazil
- Corresponding Author:
- Alexandre Franco Miranda, PhD
Department of Dentistry for Special Patients and Geriatric Dentistry
Catholic University of Brasília, Brazil
Tel: + 55 (61) 3356-9612
E-mail: alexandrefmiranda@hotmail.com
Received Date: February 07, 2017; Accepted Date: February 17, 2017; Published Date: February 27, 2017
Citation: Miranda AF (2017) The Dental Surgeons in the Hospital and their Professional Areas in Brazil: Hospitalization Units, Surgical Centers and Intensive Care Units. J Community Med Health Educ 7:505. doi:10.4172/2161-0711.1000505
Copyright: © 2017 Miranda AF. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
The lack of effective policies regarding the maintenance of oral health in hospitals helps increasing systemic diseases and damages to the patients’ health. The dentist plays a key role in diagnosing, planning and conducting clinical interdisciplinary approaches focused on the quality of life of these patients. The aim of the current study is to discuss the hospital dentistry context by emphasizing the regulation of this practice and its action field, the oral/ systemic health relation, the preventive clinical procedures, as well as the clinical difficulties and the brief guidelines, through a literature review. Scientific articles linked to hospital dentistry practices were searched in bibliographic databases and analyzed. The inclusion criteria comprised articles published in Portuguese and English indexed at the LiLACS, SciELO and PubMed databases between 2007 and 2016, the legislation about the theme and clinical experience. The search gathered 35 references. It was concluded that it is demanding to train all hospital staff and the dental surgeon on how to promote oral health, as well as to know the impact of these oral issues on the patients’ systemic health and to implement specific protocols about the herein described theme in every hospital.
Keywords
Dental service; Hospital; Dental staff; Oral health, Quality of life; Comprehensive health care
Introduction
Dentistry is of paramount importance in preventive actions, as well as in the elimination of inflammatory, infectious and painful symptomatological processes that may contribute to losses for hospitalized patients. It is associated with systemic conditions in hospital environments and overcomes the barriers and prejudices faced by those involved in this specific type of health service [1-3].
It is possible seeing the increased number of patients who require dental conducts in hospital environments, fact that demands the effective presence of the dental surgeon in multi-disciplinary activities and favors an important review concerning professional opportunities and performance areas [2-5].
Hospital dentistry can be defined as a practice that aims to care for oral changes that require multidisciplinary team procedures, the working with health professionals involved in the treatment and the approach to patients in an integral manner [1,3,4].
The health care service in hospital environments requires multidisciplinary teamwork, and it demands introducing dental practices in this work environment, wherein responsibilities are shared by doctors, dentists and the entire hospital staff [3,5].
The main issues dental surgeons deal with in most hospitals are the lack of training to the hospital staff and the little interaction among professionals when it comes to oral health. They also deal with issues derived from the prejudice shown by other health professionals and from the lack of knowledge about the activities performed by trained dental surgeons in hospital environments, as well as about their performance areas [1,2,6].
The lack of minimum preventive dental interventions may lead to serious complications and systemic impairments, which may directly affect the recovery of hospitalized patients and their quality of life, mainly of cardiac patients subjected to cardiac valve replacement, since they require dental actions aimed at suiting the oral environment in order to avoid developing bacterial endocarditis [2,3].
The resources available in hospitals to rule out complications derived from dental issues are few. There is small investment in the implementation of effective hospital systems directed to take measures aimed at promoting oral health [7-10].
The legislation concerning the practice of dental surgeons in hospital environments is in force in the Code of Dental Ethics published by the Federal Council of Dentistry (CFO - Conselho Federal de Odontologia) in 2012. According to such legislation, the trained professional can hospitalize and treat patients hospitalized in the public and private systems by always respecting the current norms and the organization of each hospital and sector [7].
It is demanding to integrate the dental surgeon to the hospital system in order to improve patients’ general health, as well as to enable the overall assessment of individuals who need special care [1-7,9].
The aim of the current study is to use a literature review to address the hospital dentistry context by emphasizing the regulation of such practice, the performance areas, the oral-systemic health relation, the clinical procedures and difficulties, as well as brief guidelines.
Methods
A search for published studies about hospital dental practice was carried out. The bibliographic search used a strategy based on the following meshes: hospital dentistry, pneumonia, intensive care unit, oral biofilms, oral hygiene, periodontitis and hospital dentistry. The abstracts of the articles found in the search were analyzed to check their compliance with the inclusion and exclusion criteria.
The inclusion criteria comprised articles published in Portuguese and English, indexed in the LILACS, SciELO and PubMed databases; articles published from 2007 to 2016; and the legislation on the subject. The following exclusion criteria were adopted: studies lacking information about sampling and analysis; theses and dissertations. Based on the analyzed scientific bases, 35 out of 42 articles related to the subject “hospital dentistry” met the herein established selection criteria.
The 35 articles included in the study comprised experience reports, literature reviews, current legislation on the subject, clinical research and randomized controlled clinical trials.
Nine (9) articles were excluded from the study due to lack of structural organization in the text, as well as to the repetition of actions and to the performance of clinical conducts in the hospital dental practice that did not meet the inclusion criteria.
Based on the literature about the specific subject and clinical experience in Brazil, it was possible addressing some conducts related to the effective participation of dental surgeons in all hospital sectors in an interdisciplinary way.
History and regulation
The development of hospital dentistry in America began in the midnineteenth century. Later, the hospital dentistry got some support from the American Dental Association, as well as the respect of the medical community. Dental surgeons proved their importance in the hospital practice, in the integral care provided to patients and in the relationship with the medical team [2,3,9-11].
According to Article 18 of the Code of Dental Ethics, which deals with hospital dentistry, the dental surgeon has the duty of hospitalizing and treating patients in public and private hospitals, with and without philanthropic nature, by respecting the technical and administrative norms of the institutions, through intersectoral actions. According to Articles 19 and 20 of the Code of Dental Ethics, dental activities performed in hospitals shall comply with the norms of the Federal Council of Dentistry [7,11].
Dental surgeons required to perform procedures that demand general anesthesia under hospital regime should follow the CFM Resolution No. 1363/1993, which addresses safety conditions in surgical environments. They should also perform in accordance with Article 44 of the Consolidation of Norms for Procedures in Dentistry Councils, which was approved by CFO Resolution No. 185/1993 [8,12].
Oral health is an integral and inseparable part of the general health of individuals, according to the First National Oral Health Conference held in 1986, as well as to Article 196 of the 1988 Constitution, which acknowledges that health is a right of all and a duty of the State; the insertion of dentistry into the hospital team is a right of every citizen [5-7].
The official regulation of the habilitation in hospital dentistry, as well as the regulation of courses, was published by the Federal Council of Dentistry in November 2015, and it emphasizes the guidelines and competencies of dental surgeons working in hospitals [8,11,12].
Hospital dentistry
The dental practice at hospitals requires professional preparation in aspects related to oral cavity care, as well as improved commitment to comprehensive and humanized care based on actions aimed at providing biopsychosocial welfare to patients [2,4].
Hospital dental activities are generally focused on assisting patients with severe systemic diseases, non-cooperating disabled people, and neurologically compromised individuals. Dental actions can be safely and comfortably performed in a way to present less risk to patients, dental surgeons and health care teams [9,10].
The request for complementary examinations enables better diagnosis and follow-ups, as well as planning with other health professionals. These are advantages that dental surgeons can have in the performance of their clinical activities in the hospital [5,11].
The dental surgeon working in the hospital system should be able to make a detailed anamnesis by assessing the interdisciplinary health context to properly plan the oral health actions. Health education activities for patients and health professionals, preventive conducts, minimal intervention actions directed to the adequacy of the oral environment, medium and great-complexity conducts aiming at eliminating inflammatory and infectious processes, as well as measures aiming at preventing patients from suffering due to oral issues that may affect their quality of life and recovery, are the dental surgeon’s competencies in the hospital [2,5].
Another convenience concerns the availability of more resources directed to emergency situations, i.e., the proper hospital physical structure and the availability of an auxiliary team trained to act in the most diverse situations, as well as to work as a team to provide the proper care to patients with specific diseases [1,4,9].
Most hospitalized patients have isolated and/or associated (more often) systemic diseases, and it makes it difficult developing a proper oral health plan. It is necessary assessing the systemic health repercussions on oral health and vice versa, so that the dental conducts can be successfully done [3,6,10].
The dental surgeon working in the hospital environment
Dental surgeons can work as health consultants and service providers in hospitals through the implementation of training, qualification, preventive guidelines and assisted practice instructions, which must be followed by the qualitative assessment of these conducts to improve services and direct specific needs [5,7,12].
The assessment of both the oral condition and the need of dental treatment in hospitalized patients requires the follow-up to be conducted by a qualified dental surgeon with hospital experience. Preventive clinical conducts, as well as conducts to assess oral health, oral lesions and other oral changes that may represent some risk or discomfort to patients, are part of the dental surgeon’s responsibility [9,10,12-14].
The presence of bacterial plaque (dental biofilm – tongue coating) in the oral cavity may influence the planned medical interventions due to microorganisms found in the mouth. The virulence factors of such microorganisms contribute to the accumulation of bacteria associated with nosocomial pneumonia, ventilator-associated pneumonia (VAP) and bacterial endocarditis, which are the most common systemic and infectious diseases related to the hospital dental context [15,16].
As an attempt to reduce and eliminate the increased rate of systemic diseases related to oral health issues, the presence of the dental surgeon in the hospital’s most diverse sectors is necessary in order to support the diagnosis of oral issues. Dental surgeons may also work as partners in medical therapies comprising either emergency and preventive procedures, in the treatment of worsened systemic conditions or hospital infections, in curative treatments, as well as in oral environment restorative and adjustment treatments as ways to provide greater comfort to patients [1,9,17,18].
Inpatient units: Dental surgeons can work as oral health consultants and as service providers in outpatient and inpatient units, knowing that the oral condition changes the evolution of and the response to the medical treatment, as well as that the oral health is compromised by factors such as stress, difficulty to perform oral hygiene, human relations, uncomfortable environment and drug interactions [3,6,10].
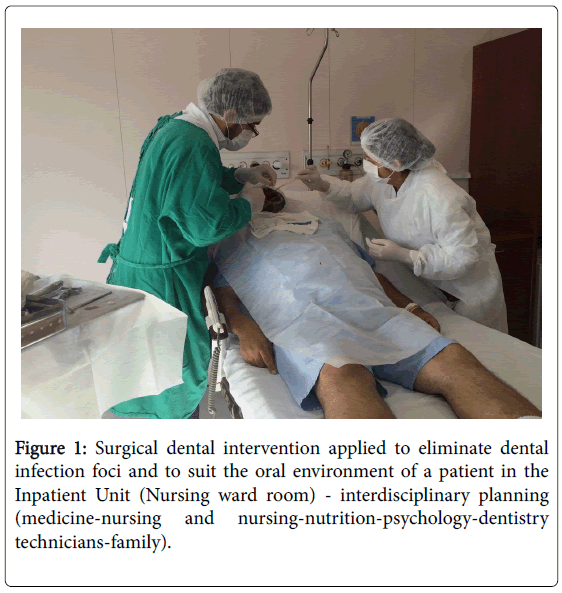
Dental conducts aim at adjusting the oral environment through the elimination of inflammatory and infectious processes, as well as of painful symptoms that may compromise the general health of hospitalized patients, based on interdisciplinary clinical planning and execution (Figure 1) [2,4,15,19].
Surgery center (General anesthesia): Unlike the ambulatory or preventive treatment, the emergency dental service is broad when it comes to oral and maxillofacial trauma emergencies. The concentration of severe diagnosis cases such as fractures and injuries is higher than that of superficial traumas. It is the most often type of provided service and it has preventive and curative dental service routines defined in the hospital environment [1,7,8,12].
The aforementioned group of services includes surgical procedures such as large bone grafts to enable dental implant fixation, facial bone fracture treatment, orthognathic surgeries, the treatment of large pathological lesions, reconstruction after tumor removal, as well as dental procedures in non-collaborating special patients (aggressive), which characterizes dental procedures performed at the hospital [4,9,17].
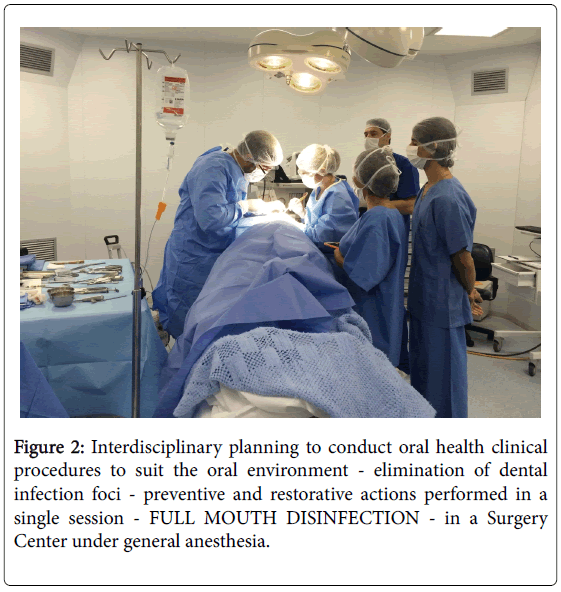
Whenever it is necessary performing dental procedures in hospital environments, the responsibility must be shared between the medical and dental teams. In case of need to perform surgical interventions and fulfill all the clinical needs of the patient in a single session (Figure 2), the clinician or specialist must perform the adequate preoperative assessment of the patient, whereas the anesthesiologist is responsible for the entire anesthetic procedure and risk in the surgical activity control [3,5,9].
Intensive Care Unit–ICU: Unsatisfactory oral hygiene is a typical finding in patients hospitalized in intensive care units and these factors may change local and systemic immunity through the selection of bacterial species, mainly of species related to nosocomial pneumonia [12,13,19-21].
ICU patients often show poor oral hygiene due to the significantly increased amount of biofilm and increased colonization by respiratory pathogens (gram-negative bacteria). In addition, the biofilm amount and complexity increase according to the hospitalization time [13,20,22].
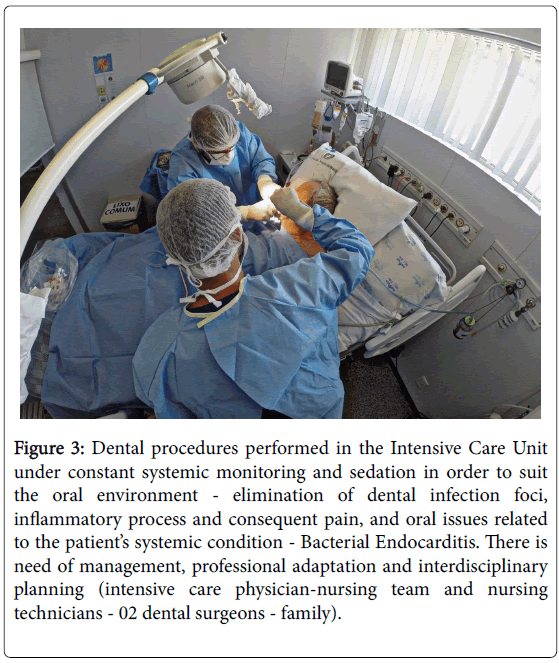
The hospital dental practice is able to co-relate oral diseases and the etiopathogenesis of several systemic diseases such as coronary heart diseases, strokes, bacterial endocarditis, diabetes mellitus and respiratory infections. Thus, the dental surgeon should participate in clinical and educational activities to promote oral health in intensive care units (Figure 3) [17,23,24].
Figure 3: Dental procedures performed in the Intensive Care Unit under constant systemic monitoring and sedation in order to suit the oral environment - elimination of dental infection foci, inflammatory process and consequent pain, and oral issues related to the patient’s systemic condition - Bacterial Endocarditis. There is need of management, professional adaptation and interdisciplinary planning (intensive care physician-nursing team and nursing technicians - 02 dental surgeons - family).
The periodontal disease stands out among oral diseases due to deficient oral health maintenance and incorrect oral hygiene in orotracheally intubated, tracheostomized and non-collaborating patients who present gram-negative microorganisms similar to those found in several chronic and respiratory infections [11,18,20,22].
Main oral issues in hospitalized patients
Caries and periodontium (dental support tissues) diseases are more prevalent and not limited to damages to the oral cavity. They may generate issues in other organic systems and in the human body. Oral health is an important and primary factor that must be related to general health, since it compromises the quality of life of individuals, mainly in hospital environments, whenever there is organic imbalance and decompensation [23,25,26].
There is permanent need of having a dental surgeon conducting patient follow-up in the hospitals, as well as of training the health professionals working in them, since the oral cavity houses microorganisms and presents several bacterial niches able to easily access the bloodstream and expose the patient to great risk of developing infection and inflammatory processes [4,5,13,14,16].
Preventing infections and inflammatory processes through oral hygiene is essential in hospital environments. The oral microbiota is influenced by extrinsic factors such as nutritional status, oral hygiene, as well as the use of medications that lead to salivary flow decrease and favor bacterial resistance. Age is a relevant intrinsic factor [27-30].
Systemic diseases and their possible relation with oral issues in hospital environments
Nosocomial pneumonia - Ventilator-Associated Pneumonia (VAP): The systemic respiratory diseases are the ones that most accumulate scientific evidence of their relation with periodontal diseases. Several studies have indicated that periodontal diseases may influence the course of respiratory infections, mainly of pneumonia [15,16,22,26,28].
The nosocomial pneumonia onsets when bacteria, mainly gramnegative rods, invade the lower respiratory tract through the aspiration of secretion from the oropharynx, through the inhalation of contaminated aerosols or, less often, through the hematogenous dissemination that may take place due to the large number of bacteria derived from periodontal infections originated from a distant focus [20,29].
The dental biofilm may work as the permanent reservoir of gramnegative microorganisms. Nosocomial pneumonia results from the aspiration of the contents found in the mouth and pharynx and it accounts for high morbidity rates and increased hospital costs [21-23,26].
Patients with depressed level of consciousness may present oropharyngeal secretion aspiration during sleep. Whenever mechanical ventilation (orotracheal intubation) is applied to patients, the oropharynx is colonized by gram-negative microorganisms in the first 48 to 72 hours after hospitalization in the ICU. These microorganisms reach the lungs through oral secretions, which are externalized through the sides of the tracheal tube cuff [11,15,18,21,29].
Prevention, health education actions and periodontal interventions may improve patients’ systemic condition, mainly in patients unable to perform their own oral hygiene [17,27,28].
Bacterial endocarditis: The bacteremia resulting from dental procedures, even from dental brushing, may cause bacterial endocarditis in certain patients. The periodontal disease is considered a risk factor for cardiovascular diseases. Thus, it is demanding to diagnose and treat it rapidly, since oral infections may have negative impact on the general health of patients [4,10,16,25].
Bacteremia may happen and when it does, it has negative impact on the patient’s health because bacteria get into the bloodstream and end up occupying the patient’s heart, mainly the heart valves. Almost 50% of the endocarditis derive from oral diseases [25,30,31].
When it comes to patients at risk of developing bacterial endocarditis, with evidence of periodontitis and poor oral hygiene, the prophylactic antibiotic therapy should be performed prior to invasive procedures performed at the hospital and even before probing the gingival sulcus [2,25,31].
Patients unable to perform the proper oral hygiene
Patients unable to brush their teeth should be cared for by family members and/or guardians, caregivers, nurses or nursing technicians guided by the dental surgeon about the correct procedures to provide the proper oral hygiene, according to their individuality [11,17,32].
It is known that these patients may present functional dependence, cognitive impairments, altered level of consciousness, as well as lack of conditions to clean their own dentures or teeth. Therefore, the dentures should be removed during hospitalization in order to reduce the niche of possible infectious, inflammatory and fungal foci such as candidiasis [1,9,10].
It is essential having dental surgeons participating in educational, preventive and minimal intervention activities, mainly guiding the specific care with the oral health of patients in each hospital sector in order to improve the quality of life of hospitalized patients, as well as to prevent them from developing health issues [18,32].
Tooth brushing should use little or no toothpaste on a toothbrush with soft and extra-soft bristles when the patient lies on the hospital bed. It is essential cleaning the patient’s tongue using tongue cleaners [10,12,15].
The mucosa, cheeks and lips should also be properly cleaned. Whenever tongue cleaners are not available, the oral hygiene can be performed using a soft toothbrush or gauze wrapped around the finger and soaked in 0.12% chlorhexidine solution. Such solution has bactericidal and bacteriostatic properties; thus, it is able to reduce the number of bacteria in the mouth without posing any risk to the patient’s health [11,12,18,24,28].
It is worth highlighting that the prolonged use of 0.12% chlorhexidine may lead to tooth staining and loss of taste, as well as affect the bacterial flora in the mouth. Thus, the use of such substance must be controlled and guided by trained dental surgeons working in the hospital [19,22,26].
Oral assessment and hygiene: brief guidelines
The minimum dental hygiene procedures and guidelines are often neglected by health professionals in hospital environments. The lack of knowledge about specific techniques and handling, the difficulty to access the patients’ oral cavity and the other tasks to be daily performed in the hospital help reducing the actions directed to oral health maintenance [29,32,33].
Therefore, it is of paramount importance having dental surgeons working in hospitals to demystify the dental conducts that must be routinely performed as an important activity directed to the specificity of the patient's case and complexity [1,3,12,18].
The initial approach should investigate main issues such as the patient’s oral health conditions, as well as classify the patient's risk to develop systemic complications based on conversations and detailed anamnesis. Subsequently, it is essential to clinically assess the patient, as well as to investigate oral issues requiring treatment, mainly in case of risk and dental emergencies [4,5,14,15].
The oral examination should be performed while the patient lies on his/her bed and should respect his/her integrity and systemic condition. The health professionals’ position is determined by the patients’ physical condition, i.e., health professionals must adapt themselves using technical and management resources in order to provide proper care to patients [18,31,34].
Several medical protocols include the need of assessment and intervention by dental surgeons previously trained in certain hospital medical procedures such as cardiac surgeries [19,22,25].
The assessment, adequacy of the oral environment and the dental surgeon performance positively affect the patient’s clinical condition and minimize factors that may negatively influence the systemic treatment. This fact gives credit to the broad concept of health due to the effective participation of dental surgeons in hospital environments [3,9,14,24].
The oral hygiene helps reducing halitosis and improving self-esteem. It also helps removing food debris and disorganizing the dental biofilm. Thus, it contributes to the adequacy of the oral environment and reduces the risks for patients to develop health issues [29,34].
The daily removal of dental biofilm and tongue coating helps improving the oral health and, consequently, the systemic health of hospitalized patients. This measure should be performed at least three times a day, after meals. Dental floss should be used on a daily basis since it helps eliminating the plaque found between the teeth. The dentist should assess the need of adjusting the indication of such measure, mainly when it is related to the systemic factor [15,18,26].
The tongue should be cleaned once a day using wooden spatulas, specific tongue scrapers, or the toothbrush itself without toothpaste in the dorsal/ventral direction, in order to avoid or hinder the development of tongue coating [11,14,16].
The most effective mouthwashes are based on 0.12% chlorhexidine and they work in the chemical control of the plaque. They are complementary to brushing and essential in several cases due to their effectiveness and rapid action [28-30,32,35].
The hygiene of dentures used by elderly patients is as important as the hygiene of the teeth. The dentures should be removed and cleaned according to protocols specific to each hospital [1,14,10].
The patients should be instructed to remove their dentures before they go to sleep or to remove them for 3 to 4 hours a day. However, some patients do not follow this recommendation due to shame, habit or lack of information [15,29].
Interdisciplinarity, prevention and health education in the hospital
Health care must be based on the sum of knowledge and focused on preventive and interdisciplinary procedures. There should be sensitivity to the social and hospital system realities [4,6,12,34].
The dentist and the working team should prioritize self-care techniques through the development of preventive and educational activities [23-25].
Oral health education activities should use models to demonstrate the correct oral hygiene techniques, and include orientation and instruction, lectures, specific courses, clarification of doubts about the frequency and how these techniques should be performed by patients, caregivers, partners and nursing professionals, mainly by nursing technicians, according to the patient's reality and dental profile [5,14,29].
It is of utmost importance that dental surgeons guide the auxiliary and multidisciplinary team in order to help promoting health and developing oral hygiene practices in the hospital, as well as eliminating harmful habits and increasing the patients’ awareness about their diets. Dental surgeons should also search for preventive measures and help adopting them in order to influence hospitalized patients to change their behavior. By doing it, these professionals help improving the patients’ clinical condition, provide well-fare, prevent systemic diseases and help them heal [18,24,26,27].
It is essential having interaction and respect between health sectors in the hospital environment as a way to assist patients in all manners through a multidisciplinary team. Such team must continuously play the fundamental role of changing pre-established paradigms and protocols [2,10,11].
Humanization in hospital care
The critical analysis, creativity, competence and technique to deal with the issue should be discussed and analyzed in order to help finding the best solution to assist hospitalized patients in their individuality and needs, as well as to characterize an inter and multidisciplinary team aimed at humanizing the relationships in this specific environment and at respecting the individual based on the bond and trust developed through the ethical and professional relationship [33-35].
The dental surgeon working in the hospital environment must know how to communicate and talk as simply and directly as possible. The explanation of all conducts and procedure stages allow the patient and the health professional to develop a trust-based relationship. In addition, the respect for the patient’s decisions and autonomy is essential to the development of a professional bond based on ethical and legal activities such as the signing of the informed consent form [1,5,18,35].
Insecurity and anxiety lead patients to fragility and concern due to the impersonality of the environment and the fear of the unknown. Thus, using positive and comforting words with hospitalized patients is fundamental to achieve the comprehensive and psychological care provided in hospital environments [4,14,17].
Health should be fully provided in hospital systems, non-dissociated from the oral cavity and its implications, and based on preventive and minimal intervention procedures that may lead to direct systemic impairment in individuals. The dental conducts must excel the technical and professional contexts. The valuation of the fragile human being, as well as of his/her anguishes and individualities, even in his/her last moments, determines the qualification of dental surgeons working in hospital environments [22,23,33,35].
Conclusions
It is necessary training and qualifying the entire hospital staff and the dental surgeon in order to provide oral health to patients, as well as to know the impact caused by oral issues on patients’ systemic health, and to implement specific protocols on this subject in all hospitals.
The dental surgeon should promote the general health of the hospitalized individual based on interdisciplinary planning developed together with other health professionals, as well as asses the patients' main needs and contribute to the quality of life of these individuals.
Acknowledgement
We would like to thank the dental surgeons Rafaela Prado, Taiane Antonelli and Felipe Moura for their effective clinical participation as assistants in the activities carried out at the Inpatient Unit, Surgical Center and Intensive Care Unit, respectively.
References
- Aguiar ASW, Guimarães MV, Morais RMP, Saraiva JLA (2010) Oral health care at the hospital level: report of experience teaching/service integration in dentistry. Rev Eletr de Extensão 7: 100-110.
- Godoi APT, Francesco AR, Duarte A, Kemp APT, Silva-Lovato CH (2010) Hospital odontology in Brazil. A general vision. Rev Odontol UNESP 38: 105-109.
- Aranega AM, Bassi APF, Ponzoni D, Wayama MT, Esteves JC, et al. (2012) How important is hospital dentistry? Rev Bras Odontol 69: 90-93.
- Carcereri DL, Amante CJ, Reibnitz MT, Mattevi GS, Da Silva GG, et al. (2011) Training in dentistry and interdisciplinarity. Rev ABENO 11: 62-70.
- Mattevi GS, Figueiredo DR, Patrício ZM, Rath IBS (2011) The participation of the dental surgeon in a multidisciplinary health team in the health care of the child in the hospital context. CienSaude Colet 16: 4229-4236.
- Saintrain MVL (2007) Proposal for a Community Indicator of Oral Health.Rev Bras Prom Saúde 3: 199-204.
- Brazil Federal Council of Dentistry – CFO (2012) Code of Ethical Dentistry. pp: 10.
- Brazil Federal Council of Dentistry – CFO (2015) Habilitation in Hospital Dentistry.
- Porto AN, Segundo AS, Borges AH, Semenoff TADV, Miranda FP (2010) Hospital Dentistry: a proposal of new discipline. RSBO 9: 119-122.
- Gaetti-Jardim E, Setti JS, Cheade MFM, De Mendonça JCG (2013) Dental care for hospitalized patients: review of the literature and proposal of oral hygiene protocol. Rev Bras Ciências da Saúde 11: 31-36.
- Gomes SF, Esteves MCL (2012) Acting of the dental surgeon in the ICU: a new paradigm. Rev Bras Odontol 69: 67-70.
- Miranda AF (2016) Oral health and care at intensive care units. J Nurs Care 5: 1-6.
- Drinka P (2010) Preventing aspiration in the nursing home: the role of biofilm and data from the ICU. J Am Med DirAssoc 11: 70-77.
- Schneid JL, Berzoini LP, Flores O, Cordon GAP (2007) Nursing practices in the promotion of oral health in the hospital of the municipality of Dianópolis-TO. ComunicaçãoCiências da Saúde 18: 297-306.
- Pobo A, Lisboa T, Rodriguez A, Sole R, Magret M, et al. (2009) A randomized trial of dental brushing for preventive ventilator-associated pneumonia. Chest 136: 433-439.
- Lockhart PB, Brennan MT, Thornhill M, Michalowicz BS, Noll J, et al. (2009) Poor oral hygiene as a risk factor for infective endocarditis–related bacteremia. J Am Dent Assoc 140: 1238-1244.
- Lima DC, Saliba NA, Fernandes LA, Garbin CAS (2011) The importance of oral health from the perspective of hospitalized patients.Ciência&SaúdeColetiva 16: 1173-1180.
- Barnes CM (2014) Dental hygiene intervention to prevent nosocomial pneumonias. J Evid Based Dent Pract 14: 103-114.
- Ames NJ, Sulima P, Yates JM, McCullagh L, Gollins SL, Soeken K, et al. (2011) Effects of systematic oral care in critically ill patients: a multicenter study. Am J Crit Care 20: e103-e114.
- Amaral SM, Cortês AQ, Pires FR (2009) Nosocomial pneumonia: importance of the oral microenvironment. J Bras Pneumol 35: 1116-1124.
- Barbosa JCS, Lobato OS, Menezes SAF, Menezes TOA, Pinheiro HHC (2010) Patients profile under intensive care with nosocomial pneumonia: key etiological agents. Rev Odontol UNESP 39: 201-206.
- Bellissimo-Rodrigues WT, Menegueti MG, Gaspar GG, Nicolini EA, et al. (2014) Effectiveness of a dental care intervention in the prevention of lower respiratory tract nosocomial infections among intensive care patients: a randomized clinical trial. Infect Control HospEpidemiol 35: 1342-1348.
- Kahn S, Garcia CH, Júnior JG, Namen FM, Machado WAS, et al. (2008) Evaluation of the existence of oral infection control in patients admitted to hospitals in the state of Rio de Janeiro. Ciência and SaúdeColetiva 13: 1825-1831.
- Miranda AF, Costa PP, Bezerra ACB (2016) Oral care practices for patients in Intensive Care Units: A pilot survey. Indian J Crit Care Med 20: 267.
- Miranda AF, De Araújo IA, De Araújo HBM, De Araújo EC, Bezerra ACB (2015) Oral health promotion in Intensive Care Unit patients: management and adaptations. GloAdv Res J Med MedSci 4: 509-513.
- El-Rabbany M, Zaghol N, Bhandari M, Azarpazhooh A (2015) Prophylactic oral health procedures to prevent hospital-acquired and ventilator-associated pneumonia: a systematic review. In J Nurs Stud 52: 452-464.
- Santos PSS, Mello WR, Wakim RCS, Paschoal MAG (2008) Use of oral solution with enzymatic system in patients totally dependent on care in an intensive care unit. RBTI 20:154-159.
- Liao YM, Tsai JR, Chou FH (2015) The effectiveness of an oral health care program for preventing ventilator-associated pneumonia. NursCrit Care 20: 89-97.
- Kiyoshi-Teo H, Blegen M (2015) Influence of institutional guidelines on oral hygiene practices in intensive care units. Am J Crit Care 24: 309-318.
- Cavezzi JO (2010) Infectious endocarditis and antibiotic prophylaxis: a subject that remains controversial for dentistry. RSBO 7: 372-376.
- Duval X, Delahaye F, Alla F, Tattevin P, Obadia JF, et al. T (2012) Temporal trends in infective endocarditis in the contexto of phrophylaxis guideline modifications. J Am CollCardiol 59: 1968-1976.
- Araújo RJG, Oliveira RCG, Hanna LMO, CorrêaAM, Carvalho LHV, et al. (2009) Analysis of perceptions and actions of oral care performed by nursing teams in intensive care units RBTI 1: 38-44.
- Marques IR, Souza AR (2010) Technology and humanization in intensive environments.Rev Bras Enferm 63: 141-144.
- Fertonani HP, de Pires DE, Biff D, Scherer MD (2015) The health care model: concepts and challenges for primary health care in Brazil. CienSaude Colet 20: 1869-1878.
- Oliva A, Miranda AF (2015) Palliative care and odontogeriatrics: brief considerations. Rev Portal de Divulgação 44: 63-69.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 8035
- [From(publication date):
February-2017 - Nov 23, 2024] - Breakdown by view type
- HTML page views : 7110
- PDF downloads : 925