Review Article Open Access
The Dental Architect
Carlson R*Carlson Bridge Technologies, Inc. Pvt Ltd, Hawaiia, USA
- *Corresponding Author:
- Ron Carlson
Carlson Bridge Technologies, Inc. —
Private Enterprise, Hawaiia, USA
Tel: 01-808-735-0282
E-mail: ddscarlson@hawaiiantel.net
Received date: February 13, 2017; Accepted date: February 17, 2017; Published date: February 28, 2017
Citation: Carlson R (2017) The Dental Architect. Dent Implants Dentures 2:115. doi:10.4172/2572-4835.1000115
Copyright: © 2017 Carlson R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Dental Science and Medicine
Abstract
The systematic and simple replacement of missing teeth without radical manipulation of existing sound structure— over preparation, utilizing scaffolding, or a matrix the “Winged Pontic” of prefabricated filled composite resin, may correctly be characterized as bio-synthetic tissue engineering. A new conversation regarding one of the direction of prosthetic dentistry for the 21st Century is offered in Stephan C. Bayne’s review of the state of the art for restorative biomaterials titled Dental Biomaterials: Where Are We and Where Are We Going? The non-invasive, uncomplicated, artistically and professionally rewarding “Winged Pontic” approach is one such arts, synthetic tissue engineering. The case report offered in this manuscript demonstrates the concept of direct and immediate tooth replacement in a step by step methodology that may easily be adapted by the dental surgeon. Fiber reinforcement is unnecessary based upon 25 years of research since it is cumbersome, ineffectual, and disruptive to the filled composite resin matrix. In any instance, the “Winged Pontic” fixed prosthesis may be viewed as a short term, medium term, or definitive restoration. It may also serve as a pediatric tooth space maintainer or as a implant stabilization prosthesis during osseointegration of dental implants by hollowing out the tissue side core of the “Winged Pontic” and placing it over the healing abutment of the dental implant
Historical Foundations
The founding of the first dental school in the world was in 1840 at Baltimore, Maryland—Baltimore College of Dental Surgery. This formalization of educational training was the necessary next first step in the evolvement of the dental surgeon, the specialist of the orthopedic surgeons, the “medical men” known of in those early years of American history. Most all practitioners of the art and science of dental surgery at that time were first trained in medicine first holding a MD degree or the equivalent.
Until 1840 and the institution of the first dental school for dental surgery, there were two modes of training; the first, as a “self-made” method attracting those who felt they were “prepared and ready to do all that dental art and skill could accomplish;” and the second called the “preceptor” method, for those who were nurtured, trained and taught by an existing practitioner in the art and science of dental surgery.
The advent and reasoning behind establishing a dental college independent of the existing medical college in Baltimore is contentious and convoluted by historical speculations. Some historians say Drs. Hayden and Harris—only two, but the most prominent, of many of the founders of the college of dental surgery at Baltimore—wished first for a “chair” in the medical school, thus making it specialty of medicine like otology, rhinology, neurology—i.e. odontology chair. However, other historians speculate that a movement for an independent school from the medical school was based upon the unique needs presented by the art and science of dental surgery—that of dealing with a highly specialize area of the body requiring one skilled in all the sciences of medical practice—physiology, chemistry, anatomy, pathology—and the art of dealing with the hardest structures of the body, the odontoncomplex.
Suffice it to say that regardless of the reasoning behind separate colleges of medicine and dental surgery we find in our world now today, the college of dental surgery was incorporated in Baltimore and became over time an outstandingly respectfully successful institution, stating a trend in all states of having independent medical schools and dental schools at universities that shared the scientific knowledge of the various disciplines found in biological sciences.
The medical faculties and dental faculties were highly cooperative and collaborative in the ultimate goal of providing society with trained people who could treat illnesses of humanity as seen in this 21st Century and at inception in 1840. But, it must be recognized that the attraction to dentistry as a profession was motivated by (and still is in our view) an underlying and often unknown desire to express the beauty, harmony of the human form in its healthy state. Both the key founders Hayden and Harris were artist in their own lives as revealed by their deep interest in art—they were both elected to the Maryland Academy of Fine Arts, an organization for artists, amateur artists, and lovers of art.
Hayden at the age of sixteen years was a carpenter and later in life a practicing architect. In time he became, through his self-education and devoted work, a licensed doctor by the Medical and Chirurgical (surgical) faculty of Maryland in 1810. Dr. Harris became a pupil of Dr. Hayden in the 1830s and in 1839 published his book The Dental Art. Both men were MDs, close friends as well as professional colleagues and later the key founders of the first dental college in the United States—Baltimore College of Dental Surgeons.
Progress in the Art and Science of Dental Surgery
From these humble beginnings we now find a highly developed art and science traced from the founding of formalized training through the work of G.V. Black in 1891, father of modern dentistry of the 20th Century, who crystalized the term “extension for prevention” that was also considered by some authorities of the 20th Century as a form of prophylactic odontotomy. Black’s later characterization of “lines of immunity” became a vague term of art and seemingly leading to unnecessary tooth destruction. As quoted in the Dental Cosmos in 1923 regarding Black’s philosophy of dentistry: “So far did the pendulum swing toward extension for prevention that one critic summarized the situation: ‘If they keep on extending, after a while there will be nothing to prevent.’”
In 1925 Dr. Sayre of Chicago’s Northwestern School of Dentistry, head of prosthetics, published his comprehensive textbook “Present Trend of Crown and Bridgework, with Special Attention to Conservation of Pulps.
The Richmond Crown—post and crown—required the intentional destruction of vital pulps of teeth prior to crown or bridge construction. The post core if done, theoretically, offered greater retention intracornally. Dr. Sayre notes in his textbook, “Ten years ago we were devitalizing the pulps of anterior teeth to use dowel crowns for bridge abutments or replacing a decayed tooth with a porcelain crown with a dowel; the pulps of the teeth were devitalized with arsenical preparations … we still have infected apices of roots in too great a number and a variety of methods treating pulpless and pathological roots resulting in indifferent success.” (Author note: I surmise “indifferent success” means failure.). Further, regarding abutment failures in crown and bridges at this time Dr. Sayre pens, “There are so many sources of failures (pointing to intentional “devitalizations” practiced in that time)…that too often the patient will be almost as well off without the product of our efforts as with it, for it is very easy in trying to eradicate one bad condition to replace it with a new one almost or quite as harmful.”
Another event took place in dentistry’s evolution in the 1880s that is noteworthy and essential to our discussion in respect today’s dental surgery relative to dental implants and our case study presented below. In their proceeding the American Dental Association, as reported and recorded in The Dental Cosmos, they held rigorous debates about “electricity” generated in the oral cavity. Although the status quo outright denied or accepted at that time the idea of the “electrochemical theory,” an in depth discussion on the subject was held [1].
Within that volume of 1880 Dr. Palmer, MDS, of Syracuse, N.Y. proposed, based upon the “electro-chemical theory,” that “Secondary” Decay—the title of his scientific paper—was a result of said electrical action upon the gold or silver restorations in the human and their demise [1].
Again, important for our purposes is the fact that dental surgery had recognized, and does today, this potential “electro-chemical” issue and its actions upon our implants, screw posts, other metals like amalgams, and crown and bridge metal restoration and its effect upon the oral cavity[2,3]. Related to this issue we present our Case Study.
Future Options in Adhesive Dentistry: Case Study
For over one hundred years, since the 1920s, we have progressed to the stage where composite adhesive dentistry—the new art and science of 21st Century dentistry and dental materials—has great options for our future. With only implant abutments available one can reconstruct a direct replacement fixed composite resin prosthesis as dielectric (non-conductive) option to ameliorate or avoid, possibly, the 1) post treatment symptoms related to electrical discharges from dissimilar metals of the dental implant; and 2) a more costly and complex systems of restoration while only employing the art and architecture of modern dental materials. (1)
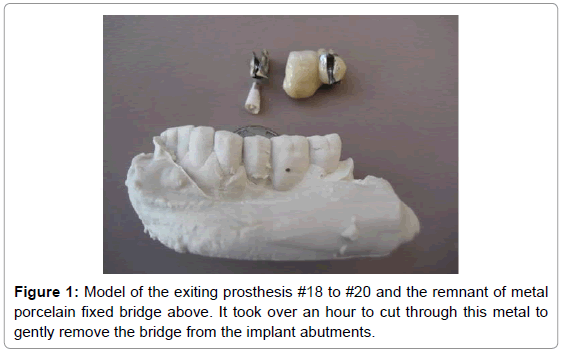
We present a case study of such a reconstruction of in a fifty three year old female who has had two implants, #20 and #18, for about two years as of her initial visit. After six months of osseointeration, a fixed metal bridge was constructed, finished and cemented in Israel (Figure 1).
She sought out our assistance and a possible solution to her lower left lip numbness—following the distribution of the mental nerve—and sever general facial drawing pressure/pain from her nose, lips, chin, forehead, and eyes, over her skull to the occipital region. The symptoms began after the metal fixed bridge was installed, worsened in the year and a half after its insertion, and persisted until her appearance and treatment in our office.
We felt that the condition of lip numbness may have been be due, more than likely, to the original surgery or the electro-galvanic dynamics of titanium post implants, their metal abutments attached to the titanium screw posts, and the metal of the porcelain to metal three tooth fixed prosthesis. We offer patients in our practice neurological assessments for various facial non-specific pain by measuring the electrical dc output of metals with a potentiometer (multi-meter: measuring mV=millivolts, and uA=micro – amperage [1-3] (EAV assessment and acupuncture may be useful tools also.).
Dissimilar metals in the oral cavity bathed in saliva (salt solution) will generate electric dc currents (uA)—corrosive forces. Normal tissues of the oral cavity do not create micro-amperages, but have voltage. These dc currents may impact human tissue cells and bacteria cells adversely or beneficially by the rust components of the metal in question [2].
We measured the uA from the implant to implant and to the metal bridges from a low at 14 uA to the high of 38 uA. We discussed options and she chose to remove the porcelain to metal bride first to see what may happen.
Two days after the removal of the metal to Porcelain Bridge see in Figure 1, the patient reported the numbness was still present but the facial to occipital symptoms had disappeared completely—that it had done so immediately, after the anesthesia disappeared. We suspect the mental nerve numbness was due to a surgical issue when implant #20 was placed (surgical damage or pressure anesthesia) and that the facial symptoms were due to very high dc electrical currents impacting facial, temporary and occipital nerve transmission.
We speculate that the aberrant uA disrupted normal electrical conduction flow along nerve, lymphatic, or blood vascular pathways thus producing the symptoms at issue. At one-week post treatment she reported that the vermillion portion of her lower left was only slightly numb, where it had been the entire lower left lip to her chin. For us this indicated more a pressure anesthesia than surgical damage to the mental nerve, since sensation was returning.
Redesigning and Rebuilding the Fixed Composite Bridge
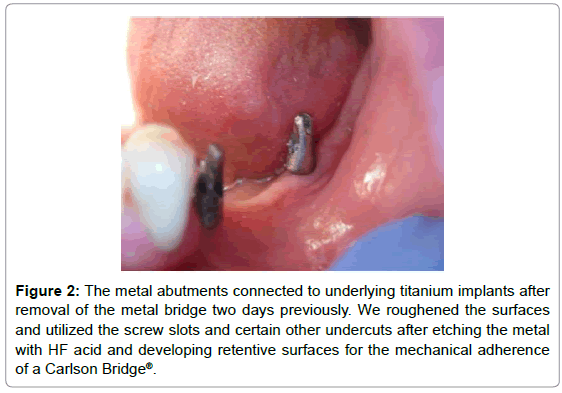
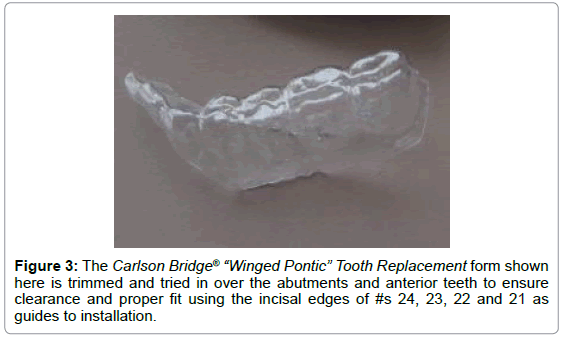
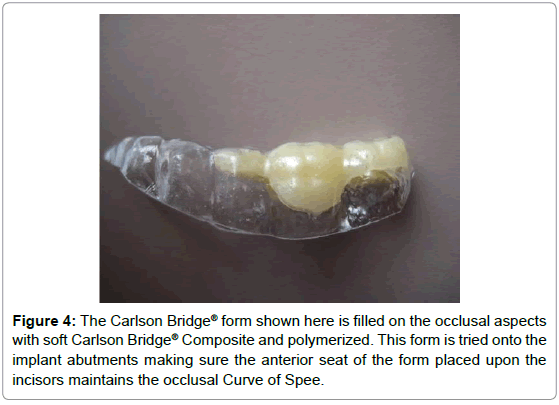
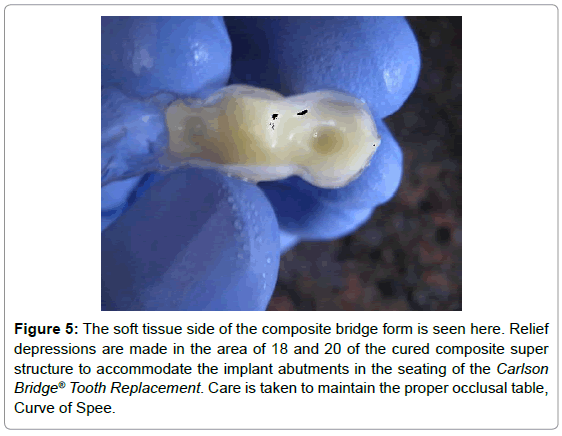
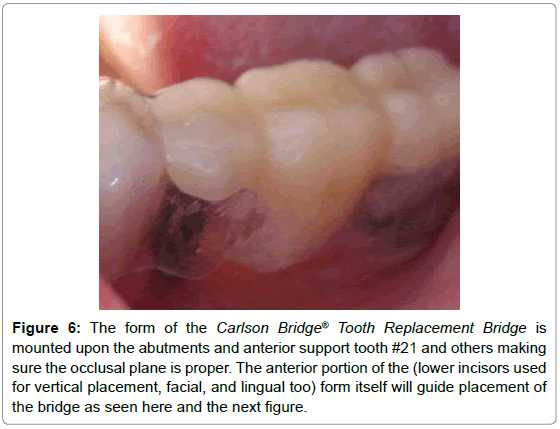
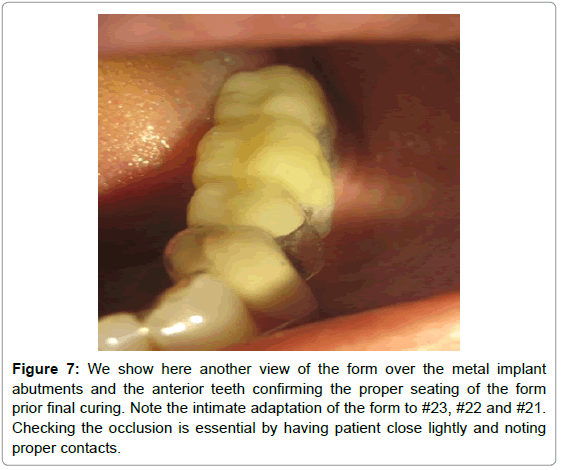
In Figure 2 we view the abutments of the implants. We developed a Carlson Bridge® Form seen in Figure 3 and constructed a cured super structure seen in Figure 4. The tissue side of the super structure bridge portion was bored out to fit easily over the implant abutments for 20 and 18, seen in Figure 5. The super structure of the composite fixed bridge fit perfectly as noted in Figures 6 and 7.
Figure 2: The metal abutments connected to underlying titanium implants after removal of the metal bridge two days previously. We roughened the surfaces and utilized the screw slots and certain other undercuts after etching the metal with HF acid and developing retentive surfaces for the mechanical adherence of a Carlson Bridge®.
Figure 5: The soft tissue side of the composite bridge form is seen here. Relief depressions are made in the area of 18 and 20 of the cured composite super structure to accommodate the implant abutments in the seating of the Carlson Bridge® Tooth Replacement. Care is taken to maintain the proper occlusal table, Curve of Spee.
Figure 6: The form of the Carlson Bridge® Tooth Replacement Bridge is mounted upon the abutments and anterior support tooth #21 and others making sure the occlusal plane is proper. The anterior portion of the (lower incisors used for vertical placement, facial, and lingual too) form itself will guide placement of the bridge as seen here and the next figure.
Figure 7: We show here another view of the form over the metal implant abutments and the anterior teeth confirming the proper seating of the form prior final curing. Note the intimate adaptation of the form to #23, #22 and #21. Checking the occlusion is essential by having patient close lightly and noting proper contacts.
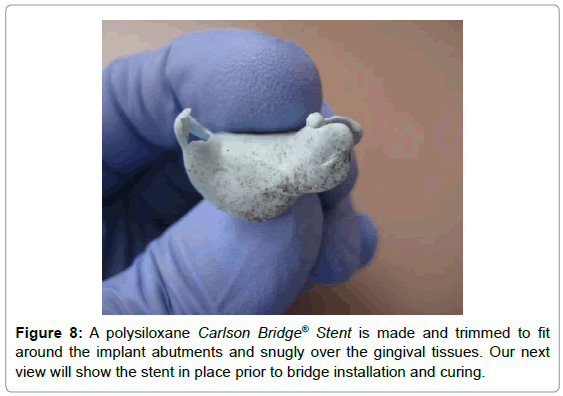
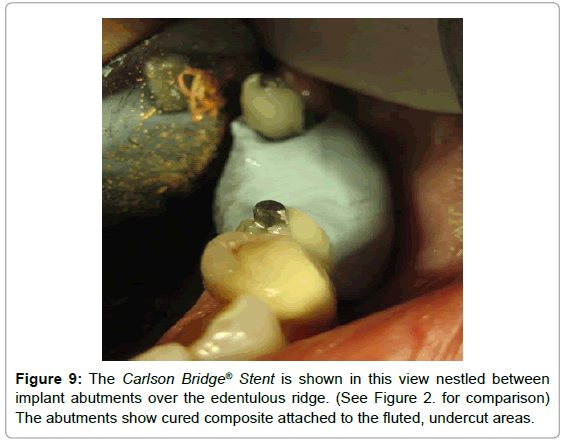
To ensure gingival tissue health we created a Carlson Bridge® Stent to cradle the soft composite applied to the tissue side of the super structure composite fixed bridge seen in Figures 8 and 9 when placed over the metal implant abutments for final adhesion to the implants and crown #21.
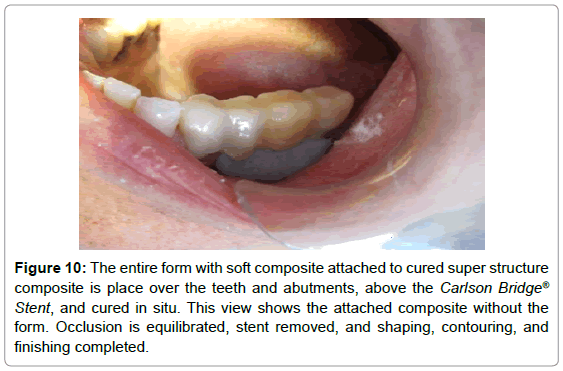
Prior to fusing the super structure and soft under composite to the implant abutments, we scored, roughened with course diamond burrs, and etched the metal, after which we layered composite into the flutes and undercut areas of the metal abutments see in Figure 9 in preparation for adhesion in situ. In Figure 10 we see the completed Carlson Bridge© that is adhered not only to the implant abutments but also the distal, facial, lingual, and occulsal of exiting porcelain veneer crown #21.
Figure 10: The entire form with soft composite attached to cured super structure composite is place over the teeth and abutments, above the Carlson Bridge® Stent, and cured in situ. This view shows the attached composite without the form. Occlusion is equilibrated, stent removed, and shaping, contouring, and finishing completed.
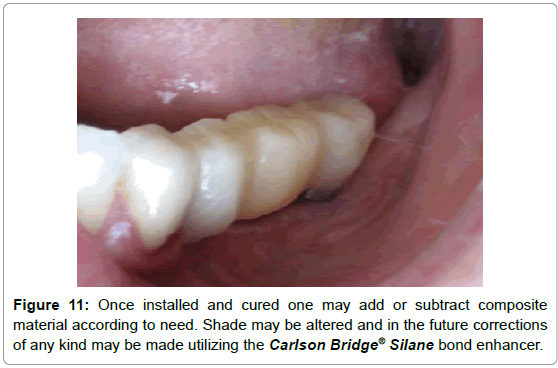
Occlusal equilibration and final finishing are done next after the Stent is removed as seen in Figure 11.
Is Fiber Reinforcement Necessary
Fiber reinforcement is thought to increase strength of composites, but is contentious—particularly used in direct dental fixed bridges— and is at best equivocal [4,5]. Fiber reinforcement procedures do not— contrary to conventional wisdom and opinion—lend to strengthening the composite composing the Carlson Bridge® [4-9].
The contrary has been shown in allegedly making the composites “stronger” (Strength=greater flexure without breaking—known as tensional integrity=“tensegrity”) by our research and the researchdemonstrations of Knight and Whttaker in 2003 reported in the journal of the Academy of General Dentistry [9-11]. Additionally, fiber reinforcement has been implicated in the premature failure of composites in clinical settings and is cumbersome and difficult to handle in its applications.
Thus, it may be understood that fibers may “hold together” the fractured composite to some degree, if it does fracture, but do not in fact prevent composite from fracturing or make it stronger by addition. The evidence presented challenges the assumption that fiberreinforcement makes the composite material “stronger,” which most clinicians presume and accept as indisputable.
Knight and Whittaker’s results are as follows: Group 1 fiber-less composite had the highest bend strength. Fibers may be used more often to hold a restoration together than for strengthening. From the Knight/Whittaker study it is suggested, and one may conclude, that fibers of this nature inserted within stock composite may weaken, not strengthen [9] (Table 1).
| Groups | Bend Strength (Mpa) | Standard deviation |
|---|---|---|
| Group 1 (Control) | 157.8 | 16.17 |
| Group 2 (Ribbond) | 140.5 | 14.92 |
| Group 3 (Nylon mesh) | 107.5 | 21.53 |
Table 1: Bend strength values of three groups.
Summation
This process, the Carlson Bridge® “Winged Pontic” tooth replacement system may open doors to new possibilities in the way dentists practice. Bio-synthetic tissue engineering [11] (Biomimetic) seems to be the leading edge in dentistry today; but only as an adjunct to other technical procedures carried out in the dental office, such as implants, flippers, or traditional porcelain veneer bridges, or the new directly placed prefabricated Componeers.
With this new methodology, it may also be a pleasant experience for the patient who can shorten his or her time in the dental chair and come away with an immediate dental cosmetic enhancement. Additionally, it will not create a financial burden or, require extensive healing time or unnecessary oral discomfort.
It is also beneficial to the dental practitioner since the procedure is shorter in duration, therefore physically less demanding, less complicated in that intricate tooth preparations are unnecessary, and ultimately more rewarding creatively, artistically and remuneratively [12].
Dr. RS Carlson graduated from the University of Michigan School of Dentistry in 1969 and completed Post Graduate training in pediatric dentistry with Strong-Carter Dental Clinic, Honolulu, Hawaii, 1970-71.
He is a founder of Kokua Kalihi Valley Dental Clinic in 1973 (http://www.kkv.net/index.php/history) and volunteered from 1973 to 1980 serving low-income families and immigrant populations from the South Pacific Islands and Asia. He has maintained a private practice in Honolulu since 1971 emphasizing Bio-Logical Dentistry. He can be reached at (808) 735-0282, ddscarlson@hawaiiantel.net or carlsonbiologicaldentistry.com.
Disclosure: Dr. Carlson is the inventor of the Carlson Bridge® “Winged Pontic” tooth replacement system, a noninvasive approach to replacing missing teeth, with patents issued in November 1999 and October 2001.
References
- Palmer SB (1880) The Dental cosmos a monthly record of dental science 22: 15-21
- Gittens RA, Olivares-Navarrete R, Tannenbaum R, Boyan BD, Schwartz Z (2011) Electrical Implications of Corrosion for Osseointegration of Titanium Implants. J Dent Res 90: 1389-1397
- Valle A, Zanardini E, Abbruscato P, Argenzio P, Lustrato G, et al. (2007) Effects of low electrical currents (LEC) treatment of pure bacterial cultures. J Appl Microbiol 103: 1376-1385
- Jokstad A, Gokce M, Hjortsjo C (2005) A systematic review of the scientific documentation of fixed partial dentures made from fiber-reinforced polymer to replace missing teeth. Int J Prosthodont 18: 489-496
- Carlson RS (1999) Breakthrough Dental Bridgework: The Bio-Logical Dental Bridge. Dent Today 18: 88-93
- Carlson RS (2003) Dental Artistry: General Dentistry. J A Gen Dent 51: 4.
- Carlson RS (2009) Cap it? Or Wrap it? Dent Today 28: 74-75
- Belvedere P, Turner WE Direct Fiber-Reinforcement Composite Bridges. Dent Today 21: 88-94.
- Knight JS, Whittaker DA (2003) A new look at chair-side fiber reinforcement of resin composite. Gen Dent 51: 334-336
- Carlson RS (2006) Immediate Post-Extraction in Situ Direct Lamination Composite Bridge. Dent Today 25: 116-119
- van Heumen CC, Kreulen CM, Bronkhorst EM, Lesaffre E, Creugers NH (2008) Fiber-reinforced dental composites in beam testing. Dent Mater 24: 1435-1443
- Bayne SC (2005) Dental Biomaterials: Where are We and Where Are We Going? J. Dent Ed 69: 571-585.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 5339
- [From(publication date):
March-2017 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 4397
- PDF downloads : 942