Research Article Open Access
The Correlation between Fetal Fibronectin, Bacterial Vaginosis and Cervical Length in Prediction of Preterm Labour
Ahmed Ibrahim Elkhadary1, Emad El-Temamy1*, Ehab Mohamed Hasanen1, Ehab Elhelw2, Ahmed Gamal Eldin Abou El Serour3 and Nabil Fathi Esmael41Department of Obstetrics and Gynecology, Al-Azhar University, Cairo, Egypt
2Department of Obstetrics and Gynecology, Al-Azhar University, Dommiate, Egypt
3International Islamic Center for Population Studies and Research, Egypt
4Department of Clinical Pathology, Al-Azhar University, Cairo, Egypt
- *Corresponding Author:
- Emad El-Temamy
Department of Obstetrics and Gynecology
Al-Azhar University, Cairo, Egypt
Tel: +201001574386
E-mail: mohammedelsokkary1@yahoo.com
Received date: April 04, 2017; Accepted date: April 14, 2017; Published date: April 18, 2017
Citation: Elkhadary AI, El-Temamy E, Hasanen EM, Elhelw E, El-Serour AGEA, et al. (2017) The Correlation between Fetal Fibronectin, Bacterial Vaginosis and Cervical Length in Prediction of Preterm Labour. J Preg Child Health 4:315. doi:10.4172/2376-127X.1000315
Copyright: © 2017 Elkhadary AI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Objective: To evaluate the diagnostic value of the cervical length (CL), fetal fibronectin (fFN) in the cervicovaginal secretion and Bacterial vaginosis (BV) infection in prediction of labor in women with threatened preterm labor (TPTL). Patients and methods: One hundred women (100) with TPTL included in this prospective study, which conducted in AL-AZHAR University, department of obstetrics and gynecology after approval of the study by the institute ethical committee and after informed consent. Women included in the study subjected to through history, general and abdominal examinations followed by collection of cervico-vaginal fluid sample for fFN assay, vaginal swab for detection of BV and TVS assessment of the cervical length. Collected data regarding, the cervical length, fFN and BV statistically analyzed to evaluate the diagnostic value of the cervical length, fFN and BV in prediction of labor in women with TPTL. Results: fFN had 86.6% sensitivity, 55.5% specificity, 52% PPV, 88.2% NPV and 64.2% accuracy for detection of labor within one week and the CL measured by TVS had 94.4% sensitivity, 77.7% specificity, 73.9% PPV, 95.4% NPV and 48.4% accuracy for detection of PTL within one week. Sensitivity, positive and negative predictive values were higher for the CL than fFN for detection of PTL within one week. However, the accuracy was better for fFN than the cervical length measured by TVS (64.2% versus 48.4%). Conclusion: fFN concentration in the cervico-vaginal secretion and CL measured by TVS were good predictors for PTL in women with TPTL. The CL at 25 mm cut-off between 28 and 35 weeks gestation had high sensitivity, high positive and negative predictive values than fFN in prediction of PTL, while the fFN was more accurate than the CL.
Keywords
Trans-vaginal; Cervical length; fFN; Bacterial vaginosis; Preterm labour
Introduction
PTL refers to the birth before 37 weeks gestation. PTL refers to the birth of a baby before its organs mature enough to allow normal postnatal survival and growth and development. Premature infants are at greater risk for short and long-term complications. As several organs in normal fetus mature between 34 and 37 weeks, and the fetus reaches adequate maturity by the end of this period. Prematurity reduced by using medications to accelerate maturation of the fetal lungs and tocolytic medications to prevent PTL [1].
Preterm singleton births indicated in 28% of all preterm singleton births due to; preeclampsia, placental abruption or fetal distress. The remaining 72% were due to spontaneous PTL with or without prematurely ruptured membranes [2]. The pathogenesis of PTL includes progesterone withdrawal, oxytocin initiation and decidual activation [3].
The diagnosis of PTL is challenging problem in contemporary obstetrics. Traditionally, the diagnosis made by combination of persistent uterine contractions and cervical changes (dilatation and/or effacement). However, the accuracy of these criteria is poor, mainly because manual assessment of cervical parameter is highly subjective [4].
Recently, two new methods for diagnosis of PTL introduced mainly transvaginal ultrasonography (TVS) and fetal fibronectin (fFN). TVS assessment of the uterine cervix provides clear images of the cervix and subsequent measurements of cervical parameters [5,6]. It noted that alterations in cervical length begin to occur approximately 10 weeks before delivery. High-risk patients with changes in their cervical length between 18 and 28 weeks gestation were at increased risk of PTL [7].
fFN is an extracellular matrix glycoprotein produced by the chorionic cells. It is normally present in vaginal secretions until 22 weeks gestation and then disappears from the cervico-vaginal secretions only to reappear before the onset of labor at term [8]. If the adhesive fibronectin interface between the chorion and the decidua damaged by mechanical factors or infection, fibronectin may reappear in the vaginal secretions earlier and its detection proposed as predictor of PTL, it measured using an Enzyme Linked Immunosorbent Assay [8]. A positive fibronectin test (50 ng/ml) or more in a patient with symptoms suggestive of PTL has been associated with an increase in the likelihood of birth before 34 weeks and birth within 7-14 days of the positive test result [9]. Although theoretical considerations suggest that these tests fFN and TVS measured cervical length are complementary, only two studies have performed with a direct comparison of these tests and achieved results are equivocal [10].
Therefore, this study designed to evaluate a diagnostic value of the CL, fFN level in the cervico-vaginal secretion and BV in prediction of labor in women with TPTL.
Patients and methods
One hundred women (100) with TPTL included in this prospective study, which conducted in AL-AZHAR University, department of obstetrics and gynecology after approval of the study by the institute ethical committee and after informed consent. Women with previous history of PTL between 24 and 33+6 weeks, singleton pregnancy, gestational age between 24-33+6 weeks, cervical dilatation <3 cm, cervical effacement ≤ 50%, intact membranes, and with 4-6 uterine contraction/hour were included in this study.
Women with multiple pregnancies, cervical dilatation ≥ 3 cm, rupture of membranes, medical disorders with pregnancy (cardiac, hypertension, diabetes and preeclampsia), congenital fetal malformations or intra uterine fetal death (IUFD), with cervical cerclage in place, ante-partum hemorrhage excluded from this study.
Women included in the study subjected to; through history including last menstrual period to determine the gestational age, full laboratory investigations (Complete Blood Count (CBC), liver and kidney functions and coagulation profile). Abdominal examination to detect fundal level, presenting part, fetal heart rate and uterine contractions.
Vaginal fluid collected from each patient from the posterior fornix before ultrasound and digital examination to assess fFN [11]. Under good illumination while the patient in lithotomy position, sterile Cusco speculum inserted into the vagina and insulin syringe used to aspirate 2 ml of secretion from the posterior vaginal fornix and the specimen placed in buffer, frozen at -70ºC within 2 h of collection and subsequently analyzed. For this study, a positive fFN result defined as any vaginal fFN ≥ 50 ng/ml [12].
Concentration of fFN antigen measured with a sensitive immunoassay (Adeza Biochemical, Sunny Vale, California, USA). This assay used the fFN specific monoclonal antibody FDC-6. The assay also used a goat antihuman plasma fibronectin IgG conjugated to alkaline phosphatase and a phenolphthalein monophosphate substrate. The absence of each standard and sample was determined in duplicate at a wavelength of 550 nm with an automated microtiter-plate reader and fFN concentrations derived from the soft Max software program.
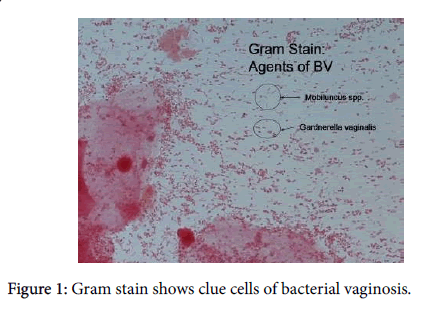
Vaginal swab obtained from all studied women using sterile cotton tipped swabs inserted 1-2 inches beyond the vaginal vestibule and rotated before withdrawing them. The swab collected under complete aseptic precautions by using a sterile dry Casco speculum (no lubricants or antiseptics were used). Swab specimen transported to laboratory and examined maximum within 2 h of collection. Swab used for direct film examination by rolling the swab on a clean glass slide. After swab drying, heat fixation and gram stain; then it examined under oil immersion lens to look for characteristic clue cells of BV. Clue cells are desquamated vaginal epithelial cells that densely coated with adherent bacteria such that their borders are indistinct [13] (Figure 1).
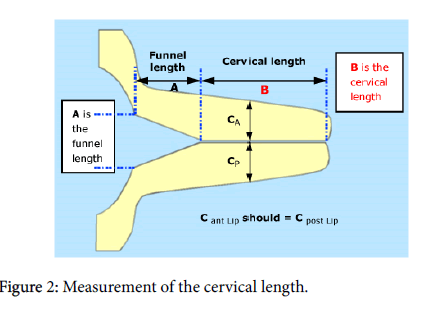
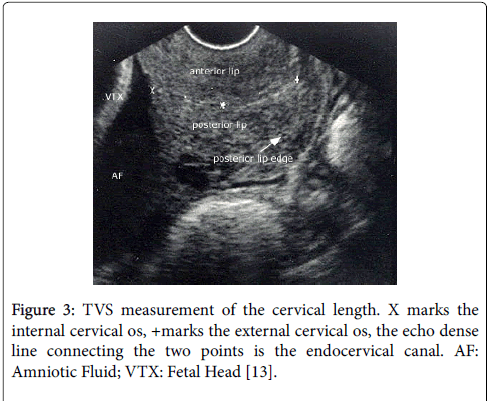
Pelvic examination done for all studied women to assess the position and consistency of the cervix, cervical effacement, conditions of the membranes and cervical dilatation. TVS examination done for studied women for dating, to rule out placenta previa and major anomalies. Estimation of the gestational age based on the last menstrual period if the last measured biparietal diameter agreed within 10 days. If not, the biparietal diameter used to define gestational age. TVS performed to measure the CL by the standardized method. Briefly, cervical length measured with a transvaginal real-time ultrasonographic probe with an empty bladder (Figure 2) [14].
The appropriate view for measurement was determined by finding the triangular echolucency at the external os, a V-shaped notch at the internal os and a faint line of echo density or echolucency between these markers. Pressure on the cervical canal, may artificially create the impression of long cervix, avoided by withdrawing the probe until the image blurred and then reapplying only sufficient pressure to restore the image again. The cervix measured three times along the line made by interface or the mucosal surface, and calipers placed at the notches made by between the internal os and external os (Figure 3) [15].
According to hospital protocol all studied women admitted and managed according to the hospital protocol as following: 1) Administration of tocolytic agent to in the form of indomethacin, atosiban or oral nifedipine. 2) Treatment continued until contractions stopped for 24 h, maximum doses attained without response unacceptable side effects occurred or labor proceeded. Women with successful treatment put under observation for another 24 h without additional treatment then discharged on no maintenance therapy. 3) Women with gestational age <34 weeks received corticosteroids in the form of 6 mg dexamethasone to be repeated/12 h for 4 doses. 4) Follow-up of the patients up to 7 days from 1st seen and then weekly in the obstetric outpatient clinic until delivery. Collected demographic data regarding, previous pregnancy, CL measured by TVS, fFN and BV statistically analyzed to evaluate a diagnostic value of the CL, fFN and BV in prediction of labor in women with TPTL.
Statistical Analysis
Collected data presented in form of range, mean ± standard deviation (SD) and percentage. Continuous test and categorical data were analyzed with the x² Pearson test. Receiver-operator curves generated for fFN in vaginal fluid and TVS assessment of the cervical length. The areas under the ROC curves analyzed and compared. Multiple logistic regression analysis performed to assess the independent contribution of fFN and CL for prediction of PTL. Pvalue< 0.05 was considered statistically significant. Sensitivity or true positive rate: addresses how good this test at picking up people who have the condition is. Specificity or true negative rate: addressees how good are this test at correctly excluding people without the condition. Positive predictive value (PPV) or posttest probability of a positive test: addresses if a person tests positive, what is the probability that he has the condition. Negative predictive value (NPV) or post-test probability of a negative test: addresses if a person tests negative, what is the probability that he does not have the condition. Accuracy: addresses what proportions of all tests have given the correct result. Likelihood ratio of a positive test: addresses how many times more likely is positive test to be found in a person with, as opposed to without, the condition.
Results
Hundred women (100) following the inclusion included in this prospective study. Their demographic and obstetric data represented in Table 1. The mean gestational age at sampling time was 31.2 ± 1.5 weeks` gestation. Ten patients (10%) had history of smoking, 8 (8%) had history of twin gestation, 30 (30%) had history of 2nd trimester loss (16-23 weeks) and 24 (24%) had history of PTL.
| Variables | Mean | ± S.D | |
|---|---|---|---|
| Maternal age (years) | 26.3 | ± 6.1 | |
| Maternal body mass index | 25.6 | ± 4.8 | |
| Gestational age at sampling time (weeks) | 31.2 | ± 1.5 | |
| Variables | Number | Percentage (%) | P value |
| Parity: | |||
| Nulliparous | 40 | 40% | 0.07 |
| Parous | 60 | 60% | |
| No. of preterm delivery (%) | |||
| Within one week | 30 | 30% | 0.15 |
| After one week | 16 | 16% | |
| No. of term delivery (%) | 54 | 54% |
Table 1: Demographic and obstetric data of the studied women.
Table 2 shows the association between fFN and PTL. 64 women (64%) had positive fFN in the cervico-vaginal fluid 36 of them (40%) delivered PTL within one week and 28 (24%) delivered PTL after one week. While 36 women (36%) had negative fFN in the cervico-vaginal fluid 4 of them (11%) delivered PTL within one week and 2 (6%) delivered PTL after one week (significance difference P=0.001). There were statistical differences between fFN positive and negative cases who delivered PTL within one week (P=0.01) and/or those delivered after 37 week (P=0.001). In this study fFN had 86.6% sensitivity for detection of PTL within one week, 55.5% specificity, 52% PPV, 88.2% NPV, 64.2% accuracy and it Likelihood ratio of was 2.9.
| Variable | Preterm delivery (37 weeks) [No., %] | P-value | Term delivery | P value | ||
|---|---|---|---|---|---|---|
| <7 days | >7 days | (>37 weeks) [No., %] | ||||
| Fetal fibronectin: | ||||||
| (+) ve>50 ng/ml [% of (+) ve cases] | 36 (40%) | 28 (22%) | 0.03* | 6 (37%) | 0.01* | |
| (-) ve<50 ng/ml [% of (-) ve cases] | 4 (11%) | 2 (6%) | 0.92 | 30 (83%) | 0.001* | |
| Gestational age at sampling time (w) | Mean | 31.9 | 32.1 | 0.21 | 30.9 | 0.09 |
| ± S.D | ± 2.5 | ± 3.4 | ± 1.2 | |||
| Gestational age at delivery (w) | Mean | 32.1 | 32.5 | 0.11 | 37.2 | 0.001* |
| ± S.D | 310% | ± 2.6 | ± 5.1 | |||
| Sampling delivery interval (days) | Mean | 250% | 9.1 | 0.18 | 49.5 | 0.01* |
Table 2: Vaginal fetal fibronectin concentrations and delivery data (*Significant difference).
Table 3 shows association between CL measured by TVS and PTL. 52 patients had short cervical length (<25 mm), 40 of them delivered PTL (34 patients within one week and 6 after one week with no significance difference) them), 48 patients had cervical length >25 mm, 6 of them delivered PTL (2 within one week and 4 after one week from examination) and 42 patients delivered term after 37 weeks gestation.
| PTD<37 week [No., %] | P value | TD (>37 week) [No., %) | P value | |||
|---|---|---|---|---|---|---|
| <1 week | >1 week | |||||
| Cervical length (% of total) | ||||||
| <25 mm | 34 (34%) | 6 (6%) | 0.12 | 6 (12%) | 0.01* | |
| >25 mm | 2 (2%) | 4 (4%) | 0.09 | 42 (42%) | 0.002* | |
| GA at sampling time (w) | Mean | 31.9 | 32.1 | >0.05 | 30.9 | 0.12 |
| ± S.D | ± 2.5 | ± 3.4 | ± 1.2 | |||
| Sampling delivery interval (days) | Mean | 2.5 | 910% | 0.08 | 49.5 | 0.01* |
| ± S.D | 0.5 | ± 1.2 | ± 3.1 | |||
| GA at delivery (w) | Mean | 32.1 | 3250% | 0.5 | 37.2 | 0.015 |
Table 3: TVS measurement of the cervical length and PTL; PTL: Preterm Labor; TD: Term Delivery; GA: Gestational Age.
In this study, the cervical length measured by TVS had 94.4% sensitivity for detection of PTL within one week, 77.7% specificity, 73.9% PPV, 95.4% NPV, 48.4% accuracy and its Likelihood ratio was 4.2.
Table 4 shows comparison between fFN test and CL measured by TVS as predictors for PTL within one week in symptomatic patients. Sensitivity, positive predictive and negative predictive values were higher for the CL than fFN for PTL within one week. However, accuracy was better for fFN (64.2% versus 48.4%).
| Variables | fFN (>50 ng/ml) | CL measured by TVS (= 25 mm) |
|---|---|---|
| Sensitivity | ||
| PTL<1 w of sampling | 86.60% | 94.40% |
| PTL>1 w of sampling | 87.50% | 60% |
| PTL = 37 w GA | 86.90% | 86% |
| Specificity | 55.50% | 77.7 |
| PPV | ||
| PTL<1 week of sampling | 52% | 73.90% |
| PTL>1 week of sampling | 36.80% | 33.30% |
| PTL<37 week GA | 62.50% | 76.90% |
| NPV | ||
| PTL<1 week of sampling | 88.20% | 95.40% |
| PTL>1 week of sampling | 93.70% | 91.30% |
| PTL<37 week GA | 83.30% | 87.50% |
| Accuracy | ||
| PTL<1 week of sampling | 64.20% | 48.40% |
| PTL>1 week of sampling | 52.30% | 75% |
| PTL<37 week of sampling | 70% | 82% |
| Likelihood ratio for positive test | 2.9 | 4.2 |
Table 4: Sensitivity, specificity, PPV, NPV and accuracy of vaginal fFN and CL measured by TVS for prediction of PTL; PTL: Preterm Labor; GA: Gestational Age; PPV: Positive Predictive Value; NPV: Negative Predictive Value; TVS: Trans-Vaginal Measurement; fFN: Fetal Fibronectin.
This study showed that incidence of BV was higher among asymptomatic women. The incidence of BV among cases with vaginitis was 12% (6 cases out of 50 cases had BV), while 16% (8 cases out of 50 cases had BV However they did not have vaginitis), P value was 0.684 (insignificant value) (Table 5).
| Vaginitis | Total | P-value | ||||
|---|---|---|---|---|---|---|
| Yes (positive) | No (Negative) | |||||
| Bacterial vaginosis | Yes | Count | 6 | 8 | 14 | 0.684 |
| % within PTB | 12.00% | 16.00% | 14.00% | |||
| No | Count | 44 | 42 | 86 | ||
| % within PTB | 88.00% | 84.00% | 86.00% | |||
| Total | Count | 50 | 50 | 100 | ||
| % within PTB | 100% | 100.00% | 100.00% |
Table 5: Incidence of Bacterial vaginosis among women who had symptoms suggestive of vaginitis versus asymptomatic.
Fifty-Two (52) cases out of 100 cases (52%) already delivered PTL, other 48% had threatened PTL, the incidence of BV among cases of established PTL was 15.4% (8 cases out of 52), but between 48 cases of TPTL, only 12.50% (6 cases out of 48) had BV. The P value was 0.769, which is insignificant. In addition 8% of the studied women cases had past history of PTL, 50% of them were positive BV (4 cases out of 8) while incidence of BV was 10.8% (10 cases out of 92) among women had no previous history of PTL, P value was 0.158 (insignificant value).
Discussion
In humans, PTL refers to the birth of a baby of less than 37 weeks gestational age, the first step in preventing disease is early prediction. In the case of PTL, two new methods for prediction were introduced recently the CL measured by TVS and fFN [16]. fFN is a glycoprotein found in the amniotic membranes, decidua and cytotrophoblast. The presence of fFN in the cervico-vaginal secretions after the 20th week of gestation is abnormal and may indicate disruption of the attachment of the membranes to the deciduas [17].
Pregnant mothers with TPTL prior to 34 weeks are often administered at least one course of glucocorticoids (beta-methasone or dexamethasone), a steroid that crosses the placental barrier and stimulates the production of surfactant in the lungs of the fetus to decrease the risk of respiratory distress syndrome. Other neonatal complications also reduced by the use of glucocorticoids namely intraventricular hemorrhage, necrotizing enterocolitis and patent ductus arteriosus [18].
Anti-contraction medications (tocolytics) appear only to have a temporary effect in delaying delivery. Tocolysis has not fulfilled its promise, as it is rarely successful beyond 24-48 h because current medications do not alter the fundamentals of labor activation [19].
Our aim was to evaluate the role of the CL measured by TVS and fFN in the cervico-vaginal secretions in prediction of PTL in symptomatic patients.
Hundred (100) women with singleton pregnancy and TPTL included in this study. In this study 40 women (40%) were nulliparous and 60 women (60%) were multiparous with no significant difference (P=0.07). The mean gestational age of the studied women at sampling time was 31.2 weeks.
Forty-Six women (46%) delivered PTL. 30 women (30%) delivered PTL within one week (with mean sampling delivery interval=2.5 days), 16 (16%) patients delivered PTL after one week (with mean samplingdelivery interval=9.1 days) with no statistical significance (P=0.08). While 54 (54%) women delivered after 37 weeks gestational age (with mean sampling-delivery interval=49.5 days) with no significance difference between PTL and term delivery (P=0.15). In this study, the incidence of PTL in women with symptoms of PTL was 46% (30% within one week and 16% after one week). It was relatively high in this study compared to (7% actually delivered within 48 h from presentation), 11% within one week [19] and still varied greatly across other studies, ranging from 8.4% [20] to 31% [21].
A flexible definition of PTL most probably underlies the cause of marked variations in the incidence of PTL in symptomatic women, as mentioned in their meta-analysis study [22].
In addition, socioeconomic variables may be included as risk factors for PTL in our population as in the United States [23], found high rate of PTL in blacks than in whites, as the gene for decidual relaxin is one candidate for PTL may be involved in preterm membrane rupture as postulated [24].
fFN test was positive in 64% of the studied women with symptomatic PTL, 26 of them (40% of positive cases) delivered PTL within one week, 14 women (22% of positive cases) delivered PTL after one week and 24 patients (37%) delivered >37 weeks (significant difference P=0.03).
While 36 patients (36%) had negative fFN test, four of them (11% of negative cases) delivered PTL within one week, two (6%) delivered PTL after one week and 30 of them (83% of negative cases) delivered after 37 weeks gestation (significance difference P=0.001). So the rate of PTL within one week in vaginal fFN positive cases was 40% in this study (P=0.01), and the difference was statistically significant in fFN positive cases for delivery within one week or after one week (P=0.03).
Marrison found that in women with positive fFN test results, 100% had true labor before 37 weeks and the interval between the assessment and sampling and the delivery was significantly shorter than in women with negative fFN.
Sensitivity of fFN in this study was similar for PTL within one week or after one week (86.6% versus 87.5%), but PPV were higher in PTL within than after one week (52% versus 36.8%). There are wide variations in fFN test in women symptomatic for preterm contractions as the sensitivity and PPV of PTL (<37 weeks) ranged from 23% to 82% and 45% to 83% respectively. Specificity and NPV were 81% to 96% and 76% to 92% in a study done [25].
While in this study sensitivity (86.6%), PPV (52%) and specificity (55.2%) within one week were comparable with those reported [26] who found 77% sensitivity and 87% specificity in symptomatic women delivered before 37 weeks within one week from sampling time.
Variability in fFN test results may due to many factors during sampling (digital examination, intercourse within 24 h, premature rupture of membranes, vaginal bleeding or the use of vaginal lubricants and disinfectants).
TVS allows obtaining clear images of the cervix and subsequent measurements of cervical parameters [27]. A cervical length of <25 mm at or before 28 weeks is always abnormal and associated with a higher incidence of PTL [28].
Fifty-Two (52%) of the studied women had short cervical length (<25 mm), 20 of them (76% of positive cases) delivered PTL (significant difference P=0.01), 34 (65%) of positive cases delivered PTL within one week with (examination-delivery interval 2.5 days) and 6 patients (15% of positive cases) delivered after PTL after one week (examination-delivery interval 9.1 days (non-significant difference P=0.12).
While 12 patients (30% of positive cases) with short cervical length delivered after 37 weeks statistically significant (P=0.01). On the other hand, 48 patients (48%) had negative results (CL>25 mm), 6 of them (12% of negative cases) delivered PTL (no significance difference P=0.09) and 42 of them delivered after 37 weeks (87% of negative cases), (significant difference P=0.002).
Leitich performed a systematic review of the use of the CL measured by TVS to predict PTL. They found that the cut-off values of CL for PTL varied in different studies from 18 to 30 mm. The incidence of PTL in short CL ranged for 70% to 100% [29].
In this study, the incidence of PTL in short cervical length patients was 76% (significant P=0.01) and for PTL within one week, it ranged from 18.2% to 46.2% and but in this study it was higher (65% of positive cases) but not significant (P=0.12). This difference may be due to the heterogeneity across the studies, different cut-offs, dynamic cervical changes associated with uterine contractions, different gestational age or risk factors.
Moreover, patients with negative CL had high incidence of term delivery after 37 weeks (87% of negative cases) in this study with statistical significance (P=0.002).
Regarding birth within 7 days in this study the sensitivity and specificity were 94.4% and 77.7% respectively for short cervical length (<25 mm) in symptomatic women. In the meta-analysis, study done on 28 studies by Sotiriadis, the pooled sensitivity and specificity of cervical length <25 mm were 78.3% and 70.8% respectively. In this study the sensitivity and specificity for CL<25 mm in predicting PTL after one week were 86% and 77.7% respectively, while were 72.4% and 93.1% respectively [30]. These differences may be due to study protocol differences as they studied patients until birth <34 weeks but this study was for delivery before 37 weeks.
In this study, comparing both tests (fFN and TVS measurement for cervical length) for prediction of PTL before 37 weeks, the positive fFN had 86.9% sensitivity, 55.5% specificity, 62.5% PPV and 70% NPV, while, the CL<25 mm assessed by TVS had 86% sensitivity, 76.9% specificity, 76.9% PPV and 87.5% NPV. This means that they are quite similar in prediction of PTL and this in agree with Rozenberg as they concluded that the advantages of performing both tests are modest. However, in their multiple logistic regression analysis confirmed that fFN in cervico-vaginal secretions and shortening of cervix, are both independently associated with PTL and proposed performing a twostep test combing the use of TVS and fFN assay [31].
In this study, the sensitivity was 86.6% for fFN versus 94.4% for CL<25 mm as predictive for PTL in positive cases within one week in symptomatic women with singleton pregnancy. These results agreed with Sotiriadis and they concluded in their meta-analysis on the CL for prediction of PTL in women with TPTL that measurement of CL in symptomatic women can detect a significant proportion of the women who will deliver within one week.
All studied women examined by taking sterile vaginal swabs to screen for BV and the prevalence of BV in women complaining of TPTL using Gram stain was 14% (14/100).
In a cohort study, 10,397 pregnant women at 23 to 26 weeks gestation who had no medical risk factors for PTL enrolled from seven medical centers. BV determined to be present or absent based on the vaginal pH and the results of Gram's staining. BV detected in 16 percent of cases [32,33] reported that the prevalence of BV varies according to size of the population studied.
Higher prevalence of BV among women with established PTL agrees with the results of this study, which reported a higher prevalence of BV in pregnant women with established PTL than threatened PTL. The incidence of BV among cases of established PTL was 15.4% and was 12.5% in cases of threatened PTL (insignificant difference). However, women with PTL might gain some benefit from this rapid BV test and antibiotics treatment [34]. Determining the prevalence of BV is difficult because one third to three quarters of affected women are asymptomatic [35]. This agreed with this present study as the incidence of BV in asymptomatic cases was 16% compared with 12% in symptomatic women.
Conclusion
fFN concentration in the cervico-vaginal secretion and CL measured by TVS were good predictors for PTL in women with TPTL. The CL at 25 mm cut-off between 28 and 35 weeks` gestation had high sensitivity, high positive and negative predictive values than fFN in prediction of PTL, while the fFN was more accurate than the CL.
References
- Berghella V, Roman A, Daskalakis C (2007) Gestational age at cervical length measurement and incidence of preterm birth. Obstet Gynecol 110: 311-317.
- Carey JC, Klebanoff MA, Hauth JC (2000) Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vaginosis. National institute of child health and human development network of maternal-fetal medicine units. N Eng J Med 342: 534-540.
- Daskalakis G, Thomakos N, Hatziionanou L (2005) Cervical assessment in women with threatened preterm labor. J Matern Fetal Neonatal Med 17: 309-312.
- Goldenberg RL, Iams JD, Das D (2008) The preterm prediction study: Spontaneous preterm birth. Am J Obstet Gynecol 182: 636-643.
- Goldenberg RL, Kleban Off M (2000) Vaginal fetal fibronectin measurements from 8 to 22 weeks gestation and subsequent spontaneous preterm birth. Am J Obstet Gynecol 183: 469-675.
- Gomez R, Romero R, Redina L (2005) Corvicovaginal fibronectin improved delivery based on sonographic cervical length in patients with preterm intact membranes. Am J Obstet Gynecol 192: 350-356.
- Gramellini D, Feini S, Kaihura C (2007) Cervical length as a predictor of preterm delivery: Gestational age-related percentiles vs. fixed cut-offs. Acta Biomed 78: 220-224.
- Hill HA, Brogan DJ, Blackmore-Prince C (2002) Exploration of threshold analysis in the relation between stressful life events and preterm delivery. Am J Epid 155: 117-124.
- Hincz P, Wilczynski J, Kozarzewski M (2002) Two-step test: The combined use of fetal fibronectin and sonographic examination of the uterine cervix for prediction of preterm delivery in symptomatic patients. Acta Obstet Gynecol Scand 81: 58-63.
- Holst RM, JAcobsson B, Hagberg H (2006) Cervical length in women in preterm labour with intact membranes. Relationship to intra-amniotic inflammation microbial invasion, cervical inflammation and preterm delivery. Ultrasound Obstet Gynecol 28: 768-774.
- Honest H, Bachmann LH, Gupta JK (2007) Accuracy of cervico-vaginal fetal fibronectin test in predicting risk of spontaneous preterm birth: Systematic review. BMJ 325: 1-10.
- Imas D, Goldenberg RL, Meis PJ (2006) The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med 334: 56-72.
- Johnson JR, Lockwood CJ, Iams JD (2010) Prediction of prematurity by transvaginal ultrasound assessment. Up to date, the clinical information service, pp: 1-7.
- Keeler SM, Roman AS, Coletta JM (2009) Fetal fibronectin testing in patients with short cervix in the mid-trimester: Can it identify optimal candidates for ultrasound-indicated cerclage? Am J Obstet Gynecol 200: 158.
- Lamont RF, Duncan SL, Mandal D (2003) Intravaginal clindamycin to reduce preterm birth in women with abnormal genital tract flora. Obstet Gynecol 101: 516-522.
- Leeson SC, Maresh MJ, Martindale EA (2008) Detection of fetal fibronectin as a predictor of preterm delivery in high risk asymptomatic pregnancies. Int J Obstet Gynaecol 103: 48-53.
- Leitich H, Brunbauer M, Bodner-Adler B (2003) Antibiotic treatment of bacterial vaginosis in pregnancy: a meta-analysis. Am J Obstet Gynecol 188: 752-758.
- Leitich H, Brun-bauer M, Kaider A (1999) Cervical length and dilatation of the internal cervical os detected by vaginal ultra-sonography as markers for preterm delivery: A systematic review. Am J Obstet Gynecol 181: 1465-1472.
- Lu GC, Goldenberg RL, Cliver SP (2001) Vaginal fetal fibronectin levels and spontaneous preterm birth in symptomatic women. Obstet Gynecol 97: 225-258.
- Maymon E, Mazor M, Romero R (2003) The ��?Yom-kippur� effect on human parturition. Am J Obstet Gynecol 176: 115.
- Meis PJ, Goldenberg RI, Mercer B (2007) The preterm prediction study: Significance of vaginal infection national institute of child health and human development maternal-fetal medicine units network. Am J Obstet Gynecol 173: 1231-1235.
- Meis PJ, Michielutte R, Peters TJ (2005) Factors associated with preterm birth in Cardiff, Wales, univariable and multivariable analysis. Am J Obstet Gynecol 173: 590-595.
- Mella MT, Berghella V (2009) Prediction of preterm birth: Cervical sonography. Semin Perinatol 33: 317-324.
- Morken NH, Hallen K, Jacobsson B (2006) Fetal growth and onset of delivery: A nation-wide population-based study of preterm infants. Am Obstet Gynecol 195: 154-159.
- Myziuk L, Romanowski B, Johnson SC (2003) BV blue test for diagnosis of bacterial vaginosis. J Clin Microbiol 41: 1925-1928.
- Netta D (2009) Polymorphism of tumor necrosis factor��?x and preterm premature rupture of membranes. Am J Obstet Gyncol 189-174.
- Oakeshott, P, Kerry S, Hay S (2004) Bacterial vaginosis and preterm birth: A prospective community-based cohort study. Br J Gen Pract 54: 119-122.
- Roberts D, Dalziel S (2006) Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 3: 4454.
- Roman AS, Koklanaris N, Paidas MJ (2005) ��?Blind� vaginal fetal fibronectin as a predictor of spontaneous preterm delivery. Obstet Gynecol 105: 285-289.
- Rozenberg P, Goffinet F, Malagrida L (1997) Evaluating the risk of preterm delivery: A comparison of fetal fibronectin and transvaginal ultrasonographic measurement of cervical length. Am J Obstet Gyncol 176: 196-199.
- Simhan HN, Caritis SN (2007) Prevention of preterm delivery. N Engl J Med 357: 477-487.
- Sotiriadis A, Makrydimas G, Papatheodorou S (2009) Does dilation and curettage versus expectant management for spontaneous abortion in patients undergoing in vitro fertilization affect subsequent endometrial development? Fertil Steril 92: 1776-1779.
- Sotiriadis A, Papathodorou S, Kavvadias A (2010) Transvaginal cervical length measurement for prediction of preterm birth in women with threatened preterm labor: A meta-analysis. Ultrasound Obstet Gynecol 35: 54-64.
- Staffarod IP, Garite TJ, Dildy GA (2008) A comparison of speculum and cervicovaginal specimens for fetal fibronectin testing. Am Obstet Gynecol 51: 614-620.
- Tosi E, Euchs IB, Rane S (2009) Sonographic measurement of cervical length in threatened preterm labour in singleton pregnancies with intact membranes. Ultrasound Obstet Gynecol 25: 353-356.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 7259
- [From(publication date):
April-2017 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 6304
- PDF downloads : 955