Research Article Open Access
The Center for Promoting Health and Health Equality’s Racial and Ethnic Approaches to Community Health Program
Kosoko-Lasaki O1*, Stone JR2, Smith J3, Brown RL3, Harris T3, Sanders R3, Jackson S4, Lassiter D5, McMorris K6, Issaka S7 and Klimowicz J31Department of Preventive Medicine and Public Health, Creighton University, Nebraska, USA
2Department of Medicine, Center for Health Policy and Ethics, Creighton University, Nebraska, USA
3Creighton University, Nebraska, USA
4Department of Douglas County Health, Creighton University, Nebraska, USA
5Nebraska Center for Healthy Families Project, Doris Lassiter Consulting, LLC, USA
6Charles Drew Health Center, Omaha, USA
7Department for Family and Community Service, Omaha, USA
- *Corresponding Author:
- Kosoko-Lasaki O, MD
MSPH, MBA, Department of Preventive Medicine and Public Health
Creighton University, Omaha, Nebraska, USA
Tel: 402-280-2332
E-mail: skosoko@creighton.edu
Received date: June 07, 2017; Accepted date: June 15, 2017; Published date: June 19, 2017
Citation: Kosoko-Lasaki O, Stone JR, Smith J, Brown RL, Harris T, et al. (2017) The Center for Promoting Health and Health Equality’s Racial and Ethnic Approaches to Community Health Program. J Community Med Health Educ 7:530. doi:10.4172/2161-0711.1000530
Copyright: © 2017 Kosoko-Lasaki O, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
African-Americans in Douglas County, Nebraska, experience above-average incidence of death and disability from chronic diseases, particularly cardiovascular disease. Current screening and education services are independent and poorly available to minority citizens. Despite communities’ progress in addressing health disparities, barriers prevent effective and culturally-competent care. Addressing these inequalities requires new and innovative models like Creighton University’s Center for Promoting Health and Health Equity, Racial and Ethnic Approaches to Community Health (CPHHE-REACH) program. This collaborative partnership with community stakeholders in Douglas County, Nebraska addresses chronic disease disparities in Omaha African-Americans by increasing community opportunities for access to physical activities. The REACH strategy involves promoting and supporting changes in policy, systems and environment (PSE). The Omaha African-American community for REACH comprises some 50,000 people. REACH program settings include Omaha faith-based organizations (churches of diverse denominations), public housing towers, a federally qualified health center, and public middle schools’ after-school program. The Douglas County Health Department and Creighton University School of Medicine personnel are key partners that provide technical assistance through the Physical Activity Leadership Train-the- Trainer mechanism for Community Health Ambassadors (CHAs) and direct support for (PSE) improvements. Thirtytwo (32) program-certified CHAs support enhancing access to physical activity in the affiliated public housing towers, diverse faith-based organizations, the health center, and the after-school programs.
Keywords
Health disparities; Physical activity; Community
Abbreviations
AA: African American; CPHHE: Center for Promoting Health and Health Equality; CDC: Centers for Disease Control and Prevention; CDHC: Charles Drew Health Center; CHA: Community Health Ambassadors; DCHD: Douglas County Health Department; PSE: Policy, Systems and Environment; REACH: Racial and Ethnic Approaches To Community Health
Introduction
Although many communities now address health disparities more effectively, barriers still prevent or impair effective culturallycompetent care, health promotion, and chronic-disease management that meet diverse peoples’ needs. These deficits call for new and innovative models to reduce community health disparities. One such framework is the Center for Promoting Health and Health Equality- Racial and Ethnic Approaches to Community Health (CPHHEREACH) Initiative, a community and academic partnership to enhance existing prevention and educational activities regarding African-American (AA) health disparities. The purpose of this publication is to describe the REACH partnership and how we have successfully promoted increased physical activity opportunities in the AA Community in Omaha, Nebraska.
REACH, a national program administered by the Centers for Disease Control and Prevention (CDC), aims to reduce racial and ethnic health disparities by strengthening capacity and implementing evidence and practice-based strategies. Through REACH, CDC supports awardee partners that establish community-based programs and culturally-tailored interventions serving six (6) minority populations (African Americans, American Indians, Hispanics/ Latinos, Asian Americans, Alaska Natives, and Pacific Islanders). REACH 2014, a three-year initiative, builds on knowledge previously developed through REACH 2010, REACH CORE, REACH U.S., REACH Minority-Serving Organizations, and REACH National Networks.
REACH partners use community-based, participatory approaches to identify, develop, and disseminate effective strategies for addressing health disparities in priority conditions or needs such as cardiovascular disease, diabetes, breast and cervical cancer, infant mortality, asthma, immunization, and obesity. Complex causes of racial and ethnic health disparities include interacting individual, community, societal, cultural, and environmental factors [1]. Thus, CDC REACH aims to eliminate racial and ethnic health disparities by:
• Supporting community coalitions that design, implement, evaluate, and disseminate community-driven strategies that target chronic disease.
• Providing the infrastructure to implement, coordinate, refine, disseminate, and evaluate successful evidence- or practice-based approaches and programs in local communities.
• Supporting national and international organizations with local affiliates and chapters to share evidence- and practice-based strategies and culturally-based community practices.
Given these REACH aims, the Center for Disease Control and Prevention (CDC) awarded Creighton University’s CPHHE a threeyear (REACH Basic) Cooperative Agreement of $1,478,778. CPHHEREACH is a collaborative agreement with community-based organizations in the AA community of Omaha (Douglas County), Nebraska, and community-serving entities, to educate about, develop, and implement policy, systems, and environmental (PSE) improvements that increase access to physical activities that reduce or prevent lifestyle-related chronic disease.
To promote such increased access to physical activity in the AA community, CPHHE-REACH involves twelve (12) local AA churches, eleven (11) Omaha Public Housing towers, Charles Drew Health Center (a federally-funded community health center), and six (6) local middle schools. We will show how the partners’ actions benefit AA experiencing chronic-disease disparities with associated physical inactivity as a risk factor. The mechanism is strengthened capacity to implement and evaluate locally-tailored PSE improvement strategies that follow above CDC REACH aims.
Increasing physical activity (PA) prevents and decreases chronic disease, such as cardiovascular disease [2-11]. To implement the CPHHE-REACH Initiative, we developed strategies to create, initiate, and maintain policies, partnering with Omaha Housing Authority (OHA), Douglas County Health Department (DCHD), Charles Drew Health Center (CDHC), Nebraska Center for Healthy Families (NCHF), Creighton University School of Medicine (SOM), Creighton University’s Health Sciences Multicultural and Community Affairs (HS-MACA), and Collective for Youth Program.
The hub of CPHHE-REACH is Creighton University’s Center for Promoting Health and Health Equality (CPHHE), a ten year community-academic partnership that (1) provides community education, promotes health risk-factor screenings, and provides other outreach activities; (2) provides student and faculty training in health disparities research; and (3) writes and promotes grant proposals to eliminate health inequalities in the Omaha community. Founded in 1878, Creighton University (CU), www.creighton.edu, is a private Jesuit, comprehensive university located in Omaha, Nebraska. CU’s mission is guided by the fundamental philosophy of education through service, caring, and community. Service to others, the importance of family life, the inalienable worth of each individual, and appreciation of ethnic and cultural diversity are core Creighton values.
As of the 2016-2017 U.S Census, the selected intervention population for CPHHE-REACH Initiative is 55,950 AA residents in Douglas County, Nebraska; 13% of the total county population of approximately 517,110 individuals [12]. These AA individuals primarily live in eastern Douglas County (northeast Omaha), essentially next-door neighbors of Creighton University.
Heart disease was the leading cause of death for AA in DCHD’s 2007 Health Status Indicator Report, an analysis of the county’s status in comparison to the Healthy People 2010 goals [13]. Moreover, “death rates for black residents in the county have followed the pattern of decline, but disparity exists with the black rate (206.2 per 100,000), about 25% higher than that seen among whites (164.7 per 100,000).” Furthermore, the 2007 Big City Health Inventory Report published by the National Association of County and City Health Officials observed that the average cardiovascular death rate for AA in the 54 cities studied was 222 deaths per 100,000, whereas the U.S. goal is 217/100,000 [14]; Omaha’s AA death rate was 203.3.
Well-known risk factors for cardiovascular disease include hypertension (HTN) and obesity, highly prevalent among AA. The Nebraska incidence of HTN in AA was 29.4% (1998-2000 survey), versus 22.6% in Whites [15]. Obesity is also a risk factor for hypertension and diabetes; the latter another risk factor for cardiovascular disease.
The CDC reports that 51% of non-Hispanic Black women age>20 are obese, compared to 33% of non-Hispanic Whites [16]. In 2007, the CDC found that about 38% of Nebraska adults were overweight and 27% were obese. While the CDC has a Nebraska-level obesity program, the Nutrition and Activity for Health (NAFH) program serves the general population. We failed to identify a program specifically targeting obesity in Nebraska AA [17].
Nationally, diabetes in AA is almost twice the prevalence in non- Hispanic Whites. AA more often develop type 2 diabetes complications like end-stage renal failure, diabetic retinopathy, and lower limb amputation [18-20]. University of Maryland Cardiologist, Elijah Saunders, states, “One AA dies as a result of high blood pressure every hour in this country, which is nearly twice as often as their White counterparts. Blacks suffer from heart and kidney disease at alarmingly high rates, both of which are adversely affected by high blood pressure. In fact, Blacks make up about 30% of those on dialysis due to kidney failure [21].” Thus, risk factors for cardiovascular disease also lead to renal problems.
Many complex medical, environmental, and psychosocial factors influence control of essential HTN (hypertension) in AA. Major barriers to awareness, treatment, and control include: (1) failure to diagnose, (2) insufficient access to medical care, (3) distrust of medical professionals, (4) inadequate treatment regimens, (5) poor adherence to medical treatments and therapeutic lifestyle changes, including tobacco avoidance, and (6) adverse medication effects [22].
To reduce and eliminate disparities such as HTN and cardiovascular disease, evidence is that effective programs require a significant community base and must build local capacity and engagement. Nationally, many programs and organizations participate in community health alliances. Strategically, these partnerships focus on one of three primary objectives: acquiring needed organizational knowledge and skills, addressing common resource needs, and pursuing a shared organizational mission. Alliances involve service delivery, planning and policy development, surveillance and assessment, and education and outreach [23].
Methods
As noted above, CPHHE-REACH and community partners include faith-based organizations, the local county health department, a federally qualified health center, health education staff from Creighton University School of Medicine, Collective for Youth after-school programs, and the local public housing authority. Each entity contributes to PSE implementation while promoting physical activities. CPHHE-REACH collaborating partners use community-based participatory research strategies in developing health policies to promote healthy living, providing health education through the Physical Activity Leadership Train-the-Trainer education of community health ambassadors (CHA), and creating indoor and outdoor walking-trail signage and mapping to guide individuals to internal and external physical-activity opportunities.
Our CPHHE-REACH Initiative employed CDC-developed guidelines for assessing policies before and after our community-based interventions. An example source was CDC’s The Community Guide: What Works to Promote Health [24]. For specific policy evaluation approaches, we also used CDC’s Using Indicators for Program Planning and Evaluation: Evaluation Guide, and Promoting Health Equity: A Resource to Help Communities Address Social Determinants of Health [25,26]. As CDC advises, program partners assess existing policies for their evidence basis, amend or develop new policies that include cost considerations, and track whether these policies are enacted. Given our diverse partners, the loci of policy analysis and advocacy vary.
Another aim of the CPHHE-REACH Initiative is to provide health education and chronic disease- awareness classes in six “pipeline” middle schools’ after-school program as part of an ongoing Focus on Health Promotions activity in the department of HS-MACA. The selected middle schools are 21st Century Learning Centers required to have at least forty percent (40%) of the student population eligible for free or reduced-cost lunch. In 2016, eight-five percent (85%) of the middle-school students served by Collective for Youth were eligible for free or reduced-cost lunch. Youth are important to target because overweight children are more likely to become obese adults with increased risk for heart disease, high blood pressure, stroke, diabetes, some types of cancer, and gall bladder disease [27].
Results
CPHHE-REACH successfully implemented the grant as CDC stipulated. The grant was awarded in the fall of 2014. All staff positions contracted and filled by February, 2015. Community Partners were identified, contracted, and regularly meeting by January, 2015. The Community Action Plan (CAP) was the contractual agreement collaboratively designed by CPHHE-REACH Administration and the CDC chief grant officer. According to the CAP, each Community Partner was assigned a Project Period Objective (PPO).
Each PPO was written with the stipulation that each Community Partner member was contracted to accomplish two (2) distinct objectives: 1.) Work with Douglas County Health Department (DCHD) to institute a series of PSE improvements, and 2.) Increase/ expand the number of new units participating internally in each separate Community Partners’ organization. A third objective, although not formally written in the CAP, was essential to the initial, continued, and future success of the agreement. That objective was: 3.) Identify a group of Community Health Ambassadors (CHA) who, after professional-development training, would design site-specific “Implementation Plans” to increase access to physical-activity opportunities in their specific community sites.
Each Community Partner fulfilled the CAP’s contracted objectives. Douglas County Health Department (DCHD) staff met with all other Community Partners to conceptualize and write new policies germane to their organization. Currently, twenty (20) newly-written policies are in CPHHE-REACH files and posted visibly throughout each Community Partners’ site.
Creighton University School of Medicine’s (SOM) health education staff and the Douglas County Health Department were contracted to provide professional-development training to the Community Health Ambassadors. They conducted three (3) training sessions employing the Train-the-Trainer model. The sessions’ purpose for CHAs was to provide lectures and experiential discussions that included human physiology, advantages and barriers to promoting physical activity, motivational principles, physical activity monitoring devices, and designing physical activity regimens to share with people in their respective communities.
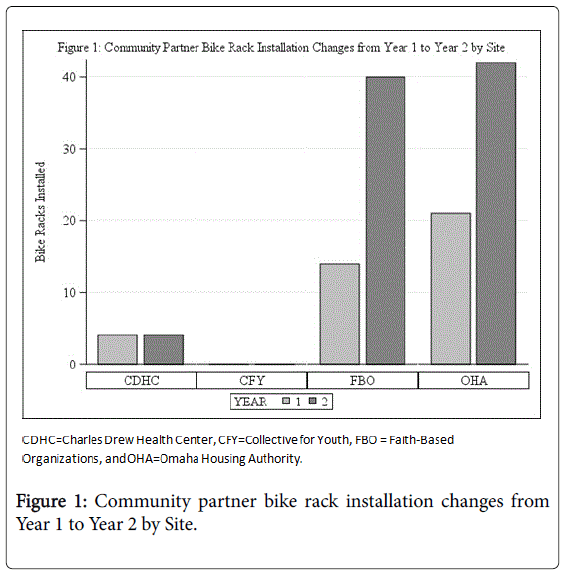
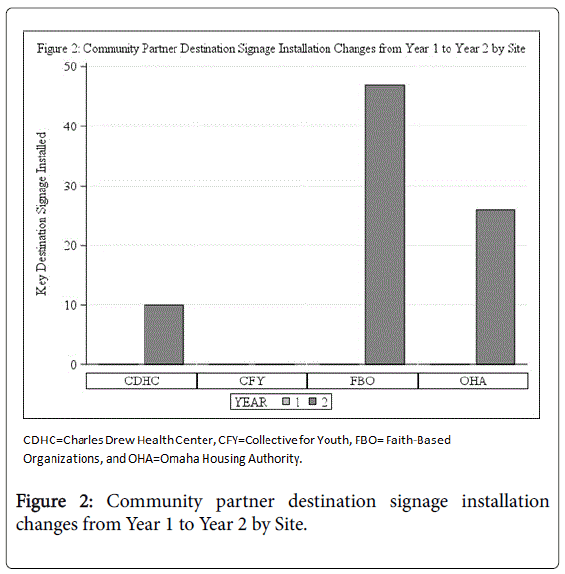
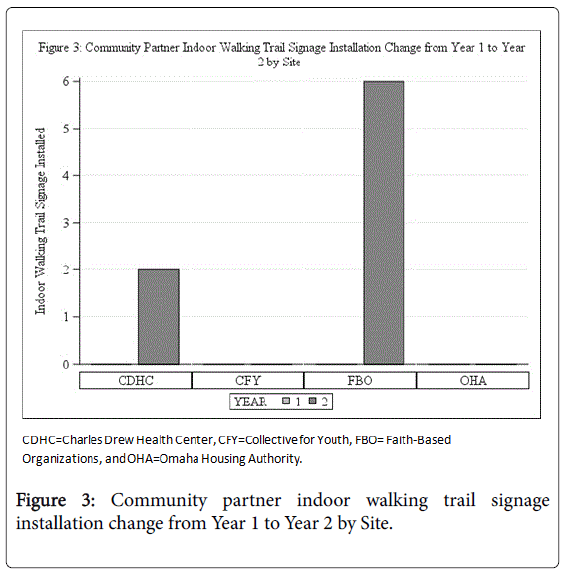
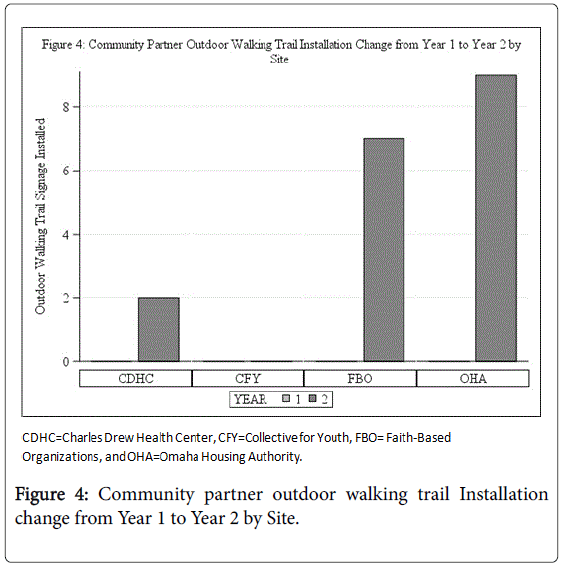
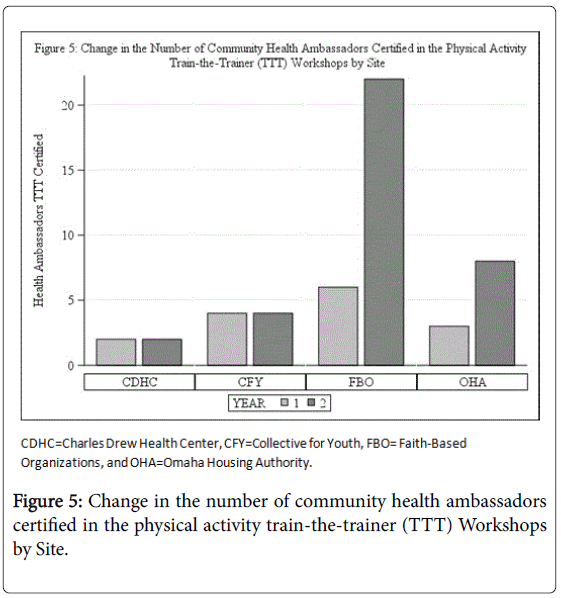
The SOM staff trained and certified thirty-seven (37) CHAs over the first two (2) grant years; twelve (12) in Year 1 and twenty-five (25) in Year 2. These areas of identified success were essential for CPHHEREACH’s success: new written policies that guided the various Community Partner members and the CHA functioning in the grassroot areas to implement the newly-designed, physical-activity opportunities at the specific sites (Figures 1-5).
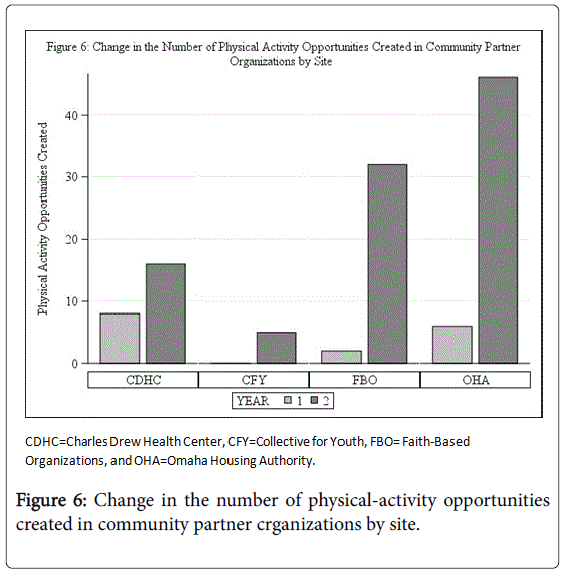
The following graphs present the increase in PSE improvements from Year 1 to Year 2.
With increased numbers of newly recruited Faith-Based Organizations (FBO) and Omaha Housing Authority (OHA) residential towers as Community Partners from Year-1 to Year-2, the figure represents the dramatic increase in newly-installed bike racks at those sites. The bike racks reflect Environmental Improvements in the Community Action Plan (CAP) objective of increasing Policy, Systems and Environmental (PSE) improvements.
The figure shows an increase in the number of Destination Signage installed near each community partner setting from Year-1 to Year-2. There were no Key Destination Signage installations conducted during Year 1, thus reflecting the dramatic increase displayed in Year 2.
The figure shows the indoor walking trail signage installation increased from zero in Year 1 at CDHC and FBO to the numbers represented in the graph in Year 2. No signage was installed for CFY or OHA during Year 1 and Year 2.
The figures show the outdoor walking trail signage installation increased from zero at CDHC, FBO, and OHA to the numbers represented in the figure in Year 2. No signage was installed for CFY during Year 1 and Year 2.
The figure shows there was a change in the number of Community Health Ambassadors from Year 1 to Year 2. FBO had a significant increase in Health Ambassadors and OHA also shows an increase. The number of Community Health Ambassadors remained the same for both CDHC and CFY (Figure 6).
The figure shows the increase in the number of physical-activity opportunities created through the Community Health Ambassadors from Year-1 through Year-2. As the number of trained and certified Community Health Ambassadors increased, physical-activity opportunities increased for patients and staff at CDHC and for parishioners and residents at other REACH Partner sites.
Discussion
The literature employs the related terms of Physical Activity (PA), Exercise (E), and Physical Fitness (PF). We follow the definition of Caspersen et al. that PA is “any bodily movement produced by skeletal muscles that results in energy expenditure” [27]. Exercise is “a subset of physical activity that is structured and repetitive and has a final or intermediate objective; the improvement or maintenance of physical fitness” [27]. Physical Fitness (PF) is “…a set of attributes that are either health- or skill-related” [27].
The sedentary lifestyle of over 40 million adults in the U.S. increases their risk for chronic-disease morbidity and mortality [27-30]. Epidemiologic studies suggest a linear dose-response relationship between physical activity and chronic-disease reduction. However, the type of PA is unimportant. Rather, total energy expenditure is key. Studies also confirm that low levels of PA and PF are strong and are independent risk factors for cardio-vascular disease, cancer, diabetes, and obesity. Further, cross-sectional studies show lower blood pressures in active individuals compared with sedentary peers. Activity alone, however, does not seem to normalize blood pressure in hypertensive individuals [30-33].
We should explain the importance of focusing on PSE improvements as identified in the CAP for CPHHE-REACH. Policy, System and Environmental improvements have the potential to sustain foundational impacts at population levels for a protracted time [33,34]. We have trained and certified Community Health Ambassadors to support the leaders of each Community Partner Member’s organization to implement the PSE improvements and promote PA in the AA in the Omaha community. Thus, CPHHE-REACH has significant potential to create persistently-positive outcomes.
Conclusion
This paper summarizes the nature of CDC REACH programs and the results of the CPHHE-REACH physical-activity initiative for AA in Omaha, Nebraska. Since 2014, CPHHE-REACH has increased physical-activity access to combat above-average death and disability rates from chronic diseases experienced by many minority and resource-poor populations. We established a team of trained Community Health Advocates who encourage “movement” in faithbased organizations, low-income housing, community healthcare centers, and youth-serving organizations.
CPHHE-REACH partners have collaboratively strengthened existing capacity to implement and evaluate locally tailored evidence, practice, and population–based PSE improvement strategies in the AA population. These efforts aim to reduce physical inactivity, is a risk factor for chronic-disease disparities.
Community partners collaboratively employed this CDC award to achieve initial success. With each Community Partner Member fulfilling their PPO, the following numbers have increased: community organizational units; newly-written policies on file and posted at the community sites; and CHAs identified, trained, and implementing newly-designed physical activities inside their respective sites. Also, physical-activity opportunities increased in all Community Partner organizations from Year 1 to Year 2.
Upon successful completion of the REACH Initiative, the physical and cultural environment for AA will be more conducive to participating in physical activity. Now, thirty-nine (39) certified REACH health ambassadors are trained to create and implement policies, systems, and environmental improvements within their organizations and surrounding communities. Those health ambassadors will be able to train others while building a team of competent instructors to teach the Physical Activity Leadership Trainthe- Trainer and PSE course.
Acknowledgement: The authors wish to thank Elaine Ickes, BGS, for her editorial assistance.CDC grant number 5 NU58DP005842-03-00
Funding/Support: No endorsement for this article was received from the Centers of Disease Control and Prevention or from Douglas County Health Department.
References
- Giles WH, Tucker P, Brown L, Crocker C, Jack N, et al. (2004) Racial and Ethnic Approaches to Community Health (REACH 2010): An Overview. Ethn Dis 14: 5-8.
- Chave SPW, Morris JN, Moss S, Semmence AM (1978) Vigorous exercise in leisure time and the death rate: A study of male civil servants. J Epid Commu Health 32: 329-343.
- Salonen JT, Puska P, Tuomilehto J (1982) Physical activity and risk of myocardial infarction, cerebral stroke and death: A longitudinal study in Eastern Finland. Am J Epidemiol 115: 526-537.
- Bissonette R, Jacoby DB, Petty GB (1986) Physical activity and longevity of college alumni. N Engl J Med 315: 399-401.
- Leon AS, Connett J, Jacobs DR Jr, Rauramaa R (1987) Leisure-time physical activity levels and risk of coronary heart disease and death: The Multiple Risk Factor Intervention Trial. JAMA 258: 2388-2395.
- Slattery ML, Jacobs DR Jr, Nichaman MZ (1989) Leisure time physical activity and coronary heart disease death: The US Railroad Study. Circulation 79: 304-311.
- Blair NS, Kohn HW, Paffenbarger RS Jr, Clark DG, Cooper KH, et al. (1989) Physical fitness and all-cause mortality: A prospective study of healthy men and women. JAMA 262: 2395-2401.
- Morris JN, Clayton DG, Everitt MG, Semmence AM, Burgess EH (1990) Exercise in leisure-time: Coronary attack and death rates. Br Heart J 63: 325-334.
- Sytkowski PA, Kannel WB, D’Agostino RB (1990) Changes in risk factors and the decline in mortality from cardiovascular disease: The Framingham Heart Study. N Engl J Med 332: 1635-1641.
- Arraiz GA, Wigle DT, Mao Y (1992) Risk assessment of physical activity and physical fitness in the Canada Health Survey mortality follow-up study. J Clin Epidemiol 45: 419-428.
- Wannamethee G, Shaper AG (1992) Physical activity and stroke in British middle aged men. BMJ 4: 597-601.
- Douglas County Health Department (2011) Region population summary by race/ethnicity.
- Douglas County Health (2007) Health status indicators report: A special public health report.
- Lenihan P, Benbow N, Weaver K, Johnson V, Brown C (2007) Big cities health inventory: The health of Urban America. National Association of County and City Health Officials.
- (2009) PRC national health report, monitoring the health status, risk & needs of Americans.
- CDN(2005) Health disparities experienced by Black or African Americans, USA 54: 11-13.
- Nebraska’s Response to Obesity (2012) Over weight and obesity. Center for Disease Control.
- Cowe CC, Port FK, Wolf RA, Savage PJ, Moli PP, et al. (1989) Disparities in incidence of diabetic end-stage renal disease according to race and type of diabetes. N Engl J Med 321: 1074-1079.
- Eggers PW, Gohdes D, Pugh J (1999) Non traumatic lower extremity amputations in the medicare end-stage renal disease population. Kidney Int 56: 1524-1533.
- Klein R, Klein BEK, Moss SE (1992) Epidemiology of proliferative diabetic retinopathy. Diabetes Care 15: 1875-1891.
- University of Maryland Medical Center (2012) Experts urge more aggressive treatment of hypertension in African-Americans.
- Bakris GL, Ferdinand KC, Douglas JG, Sowers JR (2002) Optimal treatment of essential hypertension in African Americans. Reaching and maintaining target blood pressure goals. Postgrad Med 112: 73-84.
- Mays GP, Halverson PK, Kaluzny AD (1998) Collaboration to Improve community health: Trends and alternative models. Jt Comm J Qual Improv 24: 518-540.
- Community Preventive Services Task Force (2012) The community guide: What works to promote health.
- German RR, Lee LM, Horan JM, Milstein RL, Pertowski CA, et al. (2001) Updated guidelines for evaluating public health surveillance systems. MMWR Recomm Rep 50: 1-35.
- Kreuter MW, Lezin NA, Young LA (2000) Evaluating community-based collaborative mechanisms: Implications for practitioners. Health Promotion Practice 1: 49-63.
- Caspersen CJ, Powell KE, Christenson GM (1985) Physical activity, exercise, and physical fitness. Definitions and distinctions for health-related research. Public Health Rep 100: 125-131.
- Paffenbarger RS, Hyde RT, Wing AL, Hsieh CC (1986) Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med 314: 605-613.
- Powell KE, Thompson PD, Caspersen CJ, Ford ES (1987) Physical activity and the incidence of coronary heart disease. Annu Rev Public Health 8: 253-287.
- Bouchard C, Shephard RJ, Stephens T, Sutton JR (1993) Exercise, fitness, and health: A consensus of current knowledge: Proceedings of the International Conference on exercise, fitness and health, May 29-June 3, 1988, Toronto, Canada. CABI pp: 455-566.
- Centers for Disease Control and Prevention (1991) Prevalence of sedentary lifestyle-behavioral risk factor surveillance system, United States. MMWR Morb Mortal Wkly Rep 42: 576-579.
- American College of Sports Medicine (1990) Position stand on the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness in health adults. Med Sci Sports Exer 22: 265-274.
- Mason JO, McGinnis JM (1990) Healthy people 2000: An overview of the national health promotion and disease prevention objectives. Public Health Rep 10: 441-446.
- Bunnell, O'Neil D, Soler R, Payne R, Giles WH, et al. (2012) Fifty communities putting prevention to work: Accelerating chronic disease prevention through policy, systems and environmental change. J Comm Health 375: 1081-1090.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 3641
- [From(publication date):
June-2017 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 2831
- PDF downloads : 810