Research Article Open Access
The Biohybrid Lung - Current Perspective
Christian G Cornelissen* and Stefan JockenhoevelDepartment for Tissue Engineering and Textile Implants, Helmholtz Institute of the RWTH Aachen, RWTH Aachen, Pauwelsstraße 20, Germany
- Corresponding Author:
- Christian G Cornelissen
Department for Tissue Engineering and Textile Implants
Helmholtz Institute of the RWTH Aachen
RWTH Aachen, Pauwelsstraße 20, Germany
Tel: (+49 241) 80 85551
E-mail: cornelissen@hia.rwth-aachen.de
Received date: July 19, 2013; Accepted date: December 16, 2013; Published date: December 22, 2013
Citation: Cornelissen CG, Jockenhoevel S (2013) The Biohybrid Lung - Current Perspective. J Biotechnol Biomater 3:162. doi:10.4172/2155-952X.1000162
Copyright: © 2013 Cornelissen CG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Biotechnology & Biomaterials
In the European Union, 700 lung transplantations are performed for the treatment of lung failure per year [1]. Because organ shortage limits this number, 20% of patients on the waiting list for a transplant die every year [2]. Lung transplantation’s associated risks such as acute and chronic graft rejection, the need for life-long immunosuppression and a five year survival rate of just above 50% lead to its classification as a treatment of last resort [2]. In addition, the development of obstructive bronchiolitis over time is a major problem in these patients. Leading to transplantation early in life, Mucoviscidosis is the most frequent inborn cause of terminal chronic respiratory insufficiency with an incidence of 1 in 3000 live-births [3]. End stage treatment of other chronic respiratory diseases such as Chronic Obstructive Pulmonary Disease (COPD), idiopathic pulmonary fibrosis or pulmonary arterial hypertension also involves lung transplantation as the final treatment option.
Extracorporeal Membrane Oxygenation (ECMO) can replace the lungs’ gas exchange capacity until recovery or may be used as bridge-to-transplant in terminal lung failure [4]. However, limited hemocompatibility associated with possible subsequent plasma leakage and loss of gas transfer capacity due to unspecific protein adsorption on the gas exchange membranesas well as inflammatory processes initiated by the foreign material’s surface limit its use for long-term application. Also, the limitations delineated above constrained the development of a fully implantable lung assist device.
In-depth investigation on the procoagulatory and proinflammatory processes has been carried out on cardiopulmonary bypass procedures for open heart surgery. These investigations have not only revealed altered functional status of all blood cell lines and the coagulation cascade, resulting in consumptive coagulopathy with multiple microemboli ensuing [5]. Furthermore, a set of more than 70 plasma proteins altered in their function triggers a substantive inflammatory response and a temporary dysfunction of nearly every internal organ [6,7].
As the endothelium is the only surface known not to elicit inflammatory and coagulatory responses in the blood, adopting a tissue engineering approach in persuing the goal of a fully implantable lung assist device seems sensible. The confluent endothelial layer of blood vessels regulates coagulation by tightly controlling the plasmatic coagulation cascade and the adherence of thrombocytes. The intact endothelium also orchestrates the delicate balance between pro- and anti-inflammatory stimuli at its surface.
Adopting a tissue-engineering approach to this problem, research has moved along two different paths. The holy grail of tissue engineering, the in vitro production of a complete autologous organ, has been pursued with some success. Vacanti’s group repopulated a decellularized rat lung with stem cells and demonstrated a limited gas transfer of this tissue engineered lung during in vitro tests [8]. After orthotopic transplantation in rats, the tissue engineered lungs retained their gas exchange capability for 6 hours before becoming edematous. This experiment represents a leap forward in whole organ tissue engineering but also demonstrates the long way to go before adopting this method in clinical routine.
Meanwhile, engineering of a biohybrid lung assist device seems an intermediary goal that might allow for enhanced biocompatibility of oxygenators by fabricating a confluent endothelial cell layer on top of the gas exchange membrane. In a tissue-engineering approach, this endothelialization could be performed in vitro prior to the possible implantation of the device.
Material characteristics have hampered surface endothelializationin several instances. Bengtsson and Haegerstrand [9] implanted endothelialized mechanical heart valves made from pyrolytic carbon in pigs in the pulmonary position. The endothelial cells were swept away by the blood flow within one hour. Herring et al. [10] observed similar results for the endothelialization of vessel grafts fabricated from Polytetrafluoroethylene.
Still, extensive surface modification as proposed by Haverich et al. [11] resulted in a confluent endothelial cell layer on Polymethylpentene (TPX), a material employed in the production of gas exchange membranes. These membranes, also manufactured from Polypropylene (PP) and Polydimethylsiloxane (PDMS), have been developed with a focus on lowering adhesion of proteins and cells, thus endothelial cell seeding on these surfaces is not straightforward (Table 1).
| Membrane material &O2/CO2 permeability coefficient (x10-13 cm3 cm cm-2 s-1 Pa-1) | Bio-chemical coating strategy | Confluent cell layer? | Cell layer shear stress resistant? | Reference |
|---|---|---|---|---|
| Polydimethylsiloxane 400 / 2500 | Protein adsorption | √ | Ø | Wang, Lee, Cornelissen |
| Covalent RGD bonding | √ Colon cancer cell line |
? | Sui | |
| Covalent RGD microdotting | √ | √ | Feinberg | |
| Polymethylpentene 20 / 70 |
Protein adsorption | √ | Ø | Cornelissen |
| Covalent RGD bonding | √ | √ | Hess |
Table 1: Oxygenator membrane materials and endothelial cell coating strategies.
Surface modification of Poly Di Methyl Siloxane (PDMS) for cellular attachment has been extensively studied as it is in use for microfluidic applications [12]. Proteins and peptides facilitating cell culture adhere to PDMS by adsorption or covalent bonds. Wang et al. [13] immobilized fibronectin and collagen on PDMS by adsorption and showed good cell attachment and growth rates for intestinal epithelial cells while Lee et al. [14] demonstrated growth of human umbilical artery endothelial cells on PDMS coated with fibronectin by adsorption.
Regarding adsorption strategies for protein coating onto oxygenator membranes and their effects on endothelial cell adhesion, growth and differentiation, our group performed a head-to-head comparison of a wider array of adsorbed proteins on all currently used oxygenator materials with unsatisfying results [15]. Though adsorption of fibronectin made endothelialization possible on PP, PDMS and TPX, cells reached confluence only and PDMS. Cells were swept away by fluid shear stress comparable to conditions in a conventional oxygenator.
Plasma or aggressive chemicals create reactive groups on PDMS that are highly unstable due to its low glass transition temperature of -120°C, but allow for further covalent immobilization of proteins [16]. Sui et al. [17] demonstrated this approach by covalently immobilizing RGD peptides onto PDMS, which resulted in adequate attachment of A427 cells (a colon cancer cell line). Feinberg et al. [18] employed this approach to immobilize fibronectin in a microprinted dot array onto PDMS that supported an endothelial layer of an exceptionally high density for a culture period of up to 18 days.
Much less attention has been paid to endothelial cell coating of Polymethylpentene (TPX). As it can be produced in thinner layers and thus allows higher gas transfer rates, it is presentlya better choice for oxygenator membranes but also highly expensive and difficult to process. Though our group as well as Haverich et al. [11] have shown some initial success in coating TPX with endothelial cells via adsorbed Fibronectin or covalently bond RGD peptides, this work is in its early stages [15].
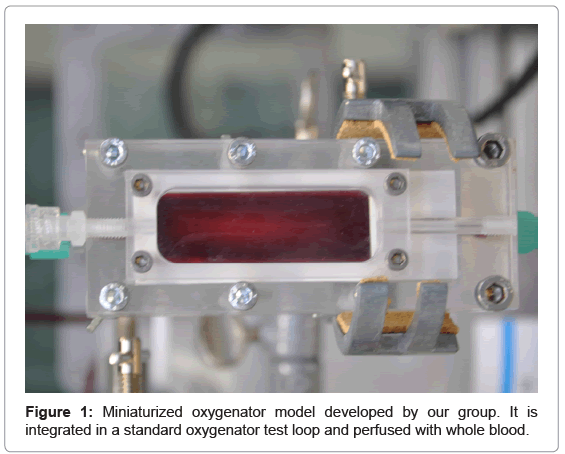
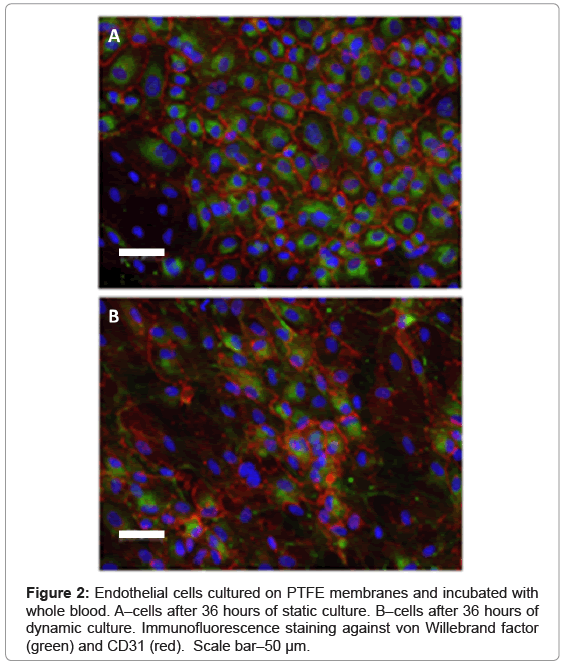
For initial studies, our group has resorted to PTFE membranes that are coated the same way as standard tissue culture plastic. These membranes are marketed by Sarstedt under the name Lumox™. Their main advantage is reliable cell coating without any further modification of the membrane’s surface. We use these membranes for an initial evaluation of a model system for a biohybrid lung assist device developed by our group (Figures 1 and 2). Currently, we are performing gas transfer measurements on endothelial cell coated membranes in this system.
Though a confluent, shear stress resistant endothelialization has been achieved on PDMS and promising first steps have been taken for TPX, at present there are no adequate investigations into the long term stability of the protein layers that allow for endothelial cell attachment [19]. As a constant turnover of extracellular matrix proteins is physiologic and has been shown to be necessary for tissue engineering, this implies at least the possibility and maybe even the likelihood of the endothelial cells changing the protein layer.
Even if successful, flow resistant endothelialization is achieved, gas transfer might be hampered to some degree by this additional diffusion barrier. Up-to-date oxygenators, such as the Novalung™ membrane ventilator, harbor membranes as thin as 2 to 5 μm. Once these dimensions are reached, the endothelial cell layer, which is approximately 5 μm in height in standard cell culture conditions, is a part of the gas transfer resistance that must be taken into account [20]. Oxygen permeability of TPX is comparable to endothelial cells’ permeability while PDMS’ oxygen permeability is higher by a factor of 10 [21]. In other words, gas permeability of the endothelial cell layer might account for half the oxygen diffusion resistance on TPX and might even be responsible for most of the oxygen diffusion resistance on PDMS if standard cell culture conditions are applied. Therefore, endothelial cell biology will become an integral part in the development of a biohybrid lung. More insight into endothelial cell biology might allow us to differentiate the endothelium towards a lung capillary phenotype. Thus, we might be able to approach the natural blood–gas barrier’s thickness of 0.3 μm.
New membrane materials that have high O2 and CO2 diffusion coefficients but also allow for endothelial cell attachment might also diminish the significant challenges awaiting researchers working the field of respiratory tissue engineering and biohybrid lung assist.
In conclusion, advances in respiratory tissue engineering and biohybrid lung assist rely on future research in:
1. Oxygenator membrane materials
2. Bio-chemical modification of membrane surfaces
3. Differentiation of lung capillary endothelial cells
References
- ISHLT Transplant Registry Quarterly Reports for Lung in Europe (2011) Characteristics for Transplants performed between January 1, 2010 and March 31, 2011
- Hertz MI, Aurora P, Benden C, Christie JD, Dobbels F, et al. (2011) Scientific Registry of the International Society for Heart and Lung Transplantation: introduction to the 2011 annual reports. J Heart Lung Transplant 30: 1071-1077.
- Dietel M, Suttorp N, Zeitz M (2005) Harrisons Innere Medizin. AWB Wissenschaftsverlag Berlin. (16thedn).
- Pesenti A, Gattinoni L, Kolobow T, Damia G (1988) Extracorporeal circulation in adult respiratory failure. ASAIO Trans 34: 43-47.
- Edmuns LH Jr, Colma RW (2003) Cardiac surgery in the adult: Thrombosis and bleeding. (2ndedn), McGraw-Hill, New York.
- Menasche P, Edmunds LH Jr (2003) Cardiac surgery in the adult: Inflammatory response. (2ndedn), McGraw-Hill, New York.
- Hammon JW, Edmunds LH Jr (2003) Cardiac surgery in the adult: Organ damage. (2ndedn), McGraw-Hill, New York.
- Ott HC, Clippinger B, Conrad C, Schuetz C, Pomerantseva I, et al. (2010) Regeneration and orthotopic transplantation of a bioartificial lung. Nat Med 16: 927-933.
- Bengntsson LA, Haegerstrand AN (1993) Endothelialization of mechanical heart valves in vitro with cultured adult human cells. J Heart Valve Dis 2: 352-356.
- Herring MB, Gardner AL, Glover J (1978) A single staged technique for seeding vascular grafts with autogenous endothelium. Surgery 84: 498.
- Haverich A, Hess C, Wiegmann B, Maurer AN, Fischer P, et al. (2010) Reduced thrombocyte adhesion to endothelialized poly4-methyl-1-pentene gas exchange membranes—a first step toward bioartificial lung development. Tissue Eng Part A 16:3043-3053.
- Zhou J, Ellis AV, Voelcker NH (2010) Recent developments in PDMS surface modification for microfluidic devices. Electrophoresis 31: 2-16.
- Wang L, Sun B, Ziemer KS, Barabino GA, Carrier RL (2010) Chemical and physical modifications to poly (dimethylsiloxane) surfaces affect adhesion of Caco-2 cells. J Biomed Mater Res A 93:1260-1271.
- Lee JN, Jiang X, Ryan D, Whitesides GM (2004) Compatibility of mammalian cells on surfaces of PDMS. Langmuir 20:11684-11691.
- Cornelissen CG, Dietrich M, Gromann K, Frese J, Krueger S, et al. (2013) Fibronectin coating of oxygenator membranes enhances endothelial cell attachment. Biomed Eng Online 12: 7.
- Bausch GG, Stasser JL, Tonge JS, Owen MJ (1998) Behavior of Plasma-Treated Elastomeric Polydimethylsiloxane Coatings in Aqueous Environment. Plasmas and Polymers. 3: 23-34.
- Sui G, Wang J, Lee CC, Lu W, Lee SP, et al. (2006) Solution-phase surface modification in intact poly(dimethylsiloxane) microfluidic channels. Anal Chem. 78: 5543-5551.
- Feinberg AM, Schumacher JF, Brennan AB (2009) Engineering high density EC monolayers on soft substrates. Acta Biomater 5:2013-2024.
- Harwardt M (2007) Funktionalisierung von Polydimethylsiloxan-Oberflächen zur Steuerung molekularer Zell-Substrat Wechselwirkungen. Dissertation. RWTH Aachen, Aachen.
- Liu SQ, Morris Y, Fung YC (1994) On measuring the third dimension of cultured endothelial cells in shear flow. Proc Natl Acad Sci 91: 8782-8786.
- Silbernagel S, Despopoulos A (2001) Taschenatlas der Physiologie. Georg Thieme Stuttgart 120.
Relevant Topics
- Agricultural biotechnology
- Animal biotechnology
- Applied Biotechnology
- Biocatalysis
- Biofabrication
- Biomaterial implants
- Biomaterial-Based Drug Delivery Systems
- Bioprinting of Tissue Constructs
- Biotechnology applications
- Cardiovascular biomaterials
- CRISPR-Cas9 in Biotechnology
- Nano biotechnology
- Smart Biomaterials
- White/industrial biotechnology
Recommended Journals
Article Tools
Article Usage
- Total views: 14256
- [From(publication date):
December-2013 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 9728
- PDF downloads : 4528