The Airway Management of One Lung Ventilation in a Patient with Tracheal Bronchus
Received: 16-Apr-2018 / Accepted Date: 20-Apr-2018 / Published Date: 27-Apr-2018 DOI: 10.4172/2167-0846.1000316
Abstract
We describe the airway management of one lung ventilation (OLV) in a 69-year-old patient with tracheal bronchus (TB). In addition to supportive treatment, we offered the patient controlled intravenous analgesia pump postoperative. The patient recovered well without any complication.
Keywords: Anesthetic management; One lung ventilation; Tracheal bronchus
Introduction
Anesthesia of one lung ventilation for patients with tracheal bronchus is a huge challenge for anesthesiologists who don’t visit the patient preoperative. In 1785, Sandifort firstly described the term TB, which was of a right upper lobe (RUL) bronchus originating from the trachea [1]. We describe the airway management of one lung ventilation in a 69-year-old patient with the tracheal bronchus.
Case Report
A 69-year-old healthy man, with the weight of 60 kg, height of 172 cm, and classified as the American society of Anesthesiologists (ASA) with the esophageal carcinoma was scheduled for a subtotal esophagogastrostomy through a combination of thoracoscopic and laparoscopic approach. Less attention was paid to the patient in consideration of no any disease. Before anesthesia was induced, the patient breathed 100% oxygen via a mask for 3 min. The patient underwent the induction of general anesthesia with propofol (2 mg/ kg), sufentanil (0.5 μg/kg) and rocuronium (0.8 mg/kg). A left sided, 37F double-lumen tube was placed by using visual laryngoscopy, the position of the bronchial cuff was confirmed by fiberoptic bronchoscope. We found the orifice above the carina which was caused by the carcinoma of the esophagus we thought through the fiberoptic bronchoscopy. We realized the importance of the airway management if the tracheal cuffs obstruct the orifice of the right upper lobe the surgeon said which can cause atelectasis or hypoxemia. We examined accurately the relationship between the position of the TB and tracheal cuff. The tracheal cuff of the tube could not obstruct the TB when the bronchial cuff in the left main bronchus. We maintained the anesthesia with appropriate concentration of sevoflurane, intermittent sufentanil and rocuronium. The operative course accomplished uneventful meanwhile the patient controlled intravenous analgesia pump (contained sufentanil 1 μg/ml, 100 ml) was offered postoperative. The patient was discharged on postoperative day 15.
Discussion
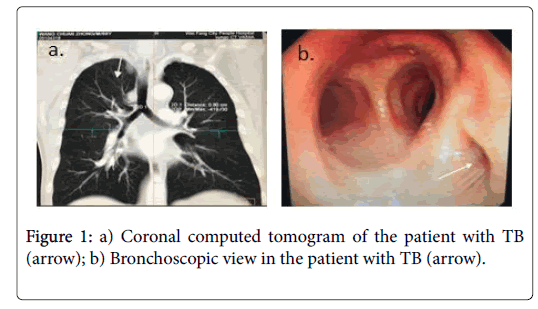
The term TB referred to a series of bronchial anomalies which originate from the trachea or main bronchus and finally merge into the upper lobe [2]. Bronchographic and bronchoscopic studies have found the prevalence of right tracheal bronchus was 0.1%-2% and the prevalence of left tracheal bronchus was 0.3%-1% [3]. In our case we thought the TB was the right upper lobe, but actually it was the apical segmental bronchus thorough evaluation of the preoperative CT scans by ourselves (Figure 1). The distance from the carina was mostly within 2 cm which was described as bronchial trifurcation [4] or as high as 6 cm which was mostly in the right side [5]. In our case the distance between the TB and carina was 0.9 cm which was located below the tracheal cuff ensuring the patency of the TB. The normal right upper lobe bronchus arises above the right pulmonary artery which was described as eparterial, and the normal left upper lobe bronchus arises below the left pulmonary artery which was described as hyparterial. It’s called preeparterial if the anomalous bronchus arises from the origin of the right upper lobe bronchus [6] in our case. TB has two types: Supernumerary TB which is an accessory bronchus and displaced TB which arises from an abnormal position and supplies the apical segment or more segments of the upper lobe [7]. In our case the apical segmental bronchus displaced the tracheal above the carina 0.9 cm. In retrospect our case, the length from the peripheral edge of the tracheal cuff to the proximal edge of the bronchial cuff was 3.4 cm which ensure the TB below the tracheal cuff. It’s fortune for us who undiscovered the TB to succeed in lung isolation and ventilation. There was different result if the surgical site and type of OLV device were different.
Conclusion
In summary, we report a case of airway management of one lung ventilation in a patient with TB. It’s important for us to evaluate the preoperative scans by ourselves instead of relying on the surgeon and radiologist reporting. It’s necessary to correctly place the double lumen tube by using the fiberoptic bronchoscope.
References
- Srivastava A, Warrier G, Trehan M (2010) Tracheal Bronchus: A Cause of unexplained prolonged hypoxemia during ventilation. Pediatr Cardiol 31: 1229-1231.
- Agarwal S, Banks MA, Dalela S (2016) Incidental finding of tracheal bronchus complicating the anesthetic management of a left video-assisted thoracoscopic procedure. J Anaesthesiol Clin Pharmacol 32: 106-108.
- Ghaye B, Szapiro D, Fanchamps JM (2001) Congenital bronchial abnormalities revisited. RadioGrap 21: 105-119.
- Zylak CJ, Eyler WR, Spizarny DL (2002) Developmental lung anomalies in the adult: Radiologic-pathologic correlation. RadioGrap 22: S25-S43.
- Wong DT, Kumar A (2006) Case report: Endotracheal tube malposition in a patient with a tracheal bronchus. Can J Anaesth 53: 810-813.
- Boonsarngsuk V, Suwatanapongched T (2011) Puzzling bronchial trifurcation. Respiratory Care 56: 1206-1208.
- Ikeno S, Mitsuhata H, Saito K (1996) Airway management for patients with a tracheal bronchus. British J anaesth 76: 573-575.
Citation: Li H, Zhu XL, Li M, Lang B, Li R (2018) The Airway Management of One Lung Ventilation in a Patient with Tracheal Bronchus. J Pain Relief 7: 316. DOI: 10.4172/2167-0846.1000316
Copyright: © 2018 Li R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5230
- [From(publication date): 0-2018 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 4346
- PDF downloads: 884