The 100 Most Influential Manuscripts in Laparoscopic Adjustable Gastric Banding: A Bibliometric and Altmetric Analysis
Received: 13-Oct-2021 / Accepted Date: 27-Oct-2021 / Published Date: 03-Nov-2021 DOI: 10.4172/2165-7904.1000468
Abstract
Background: Bibliometric analysis identifies the most cited publications, which define understanding of Laparoscopic Adjustable Gastric Banding (LAGB). In this study, the 100 most cited articles in the field of LAGB were studied and correlation between Total Citation Count (TCC), Citation Rate Index (CRI), Level of Evidence (LOE), and Altmetric Attention Scores (AAS) analysed.
Methods: The Thomson Reuters Web of Science database was used to identify relevant English language articles using the search terms: ((laparo* and adjust* and gastr* and band*) OR (LAGB or L.A.G.B.)) AND ALL FIELDS: ((endoscop* or remov* or complicat*)). The 100 most cited papers analysed.
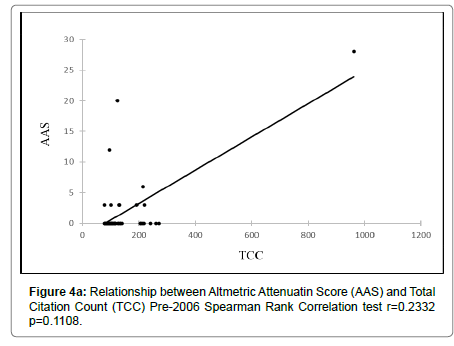
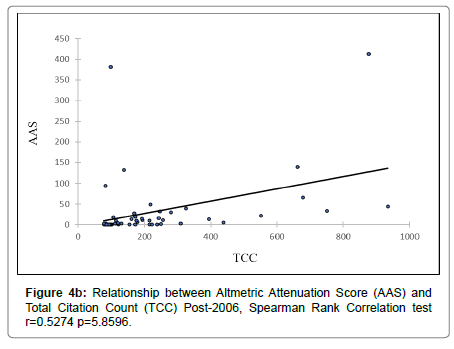
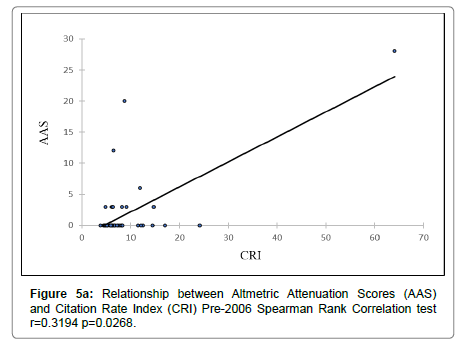
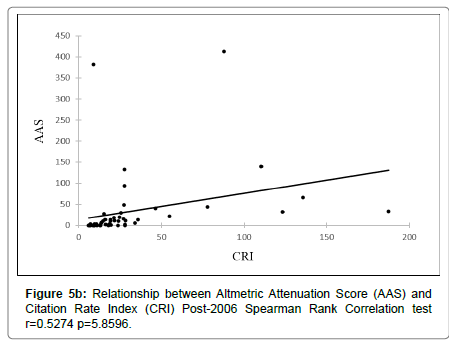
Results: 1,473 articles were returned with median citation count of 122 [interquartile range (IQR):96.75–215.25]. The most cited article was ‘Surgical Treatment of Obesity’ by Maggard et al. (962 citations). The journal “Obesity Surgery” published the most papers within the top 100 and had the highest TCC (n=36, 5633 citations). The article with the highest AAS. LOE was significantly related to TCC (p=0.0029), CRI (p=0.00002) and AAS (p=0.00173). Articles published post-2006 had a higher AAS compared to pre-2006 (p=0.00001). The AAS of articles published pre-2006 were not correlated with the TCC (r=0.2332, p=0.1108) but had a positive correlation with the CRI (r=0.3194, p=0.0268). The AAS post-2006 did not have a significant correlation with TCC (r=0.5274, p=5.8596) or CRI (r=0.5274, p=5.8596).
Conclusion: Bibliometric indices provide an important perspective on article impact and are related to evidence level. AAS and, consequently, social media impact is now a valid measurement of academic impact.
Keywords: Obesity; Overweight; Laparoscopy; Laparoscopic adjustable gastric banding
Introduction
Laparoscopic adjustable gastric banding (LAGB) is one of the most popular operations performed worldwide for morbid obesity [1]. There is an ever expanding body of evidence about LAGB which includes indications, effect on weight loss and improvement of associated comorbidities, common complications and long-term outcomes. One of the methods of identifying the published research work that has had the greatest impact on our understanding of the various aspects of LAGB is by generating and analysing a citation rank list. A citation is generated when a published article formally references another article and it is now widely accepted by the academic medical community that research impact is strongly correlated with the number of citations [2]. Bibliometrics is a branch of information research which deals with the study and analysis of meta-data surrounding published material [3]. Citation analysis is a branch of bibliometrics that evaluates the impact of an article or journal based on the total number of citations received by that article. Detailed review and statistical analysis of the publications in the citation rank list provides valuable information and insight into the types of research studies that influence and generate interest in the academic world. To date, there has been no study undertaken to identify and analyse the most influential publications in the context of LABG.
Citation count is now a well-established method within the field of Bibliometrics to measure the impact of a published research study but it does have some recognised weaknesses. For example, papers with very high original impact can become a victim of their own success as far as citations are concerned due to the phenomenon of obliteration by incorporation [4]. These papers tend to be cited with increasingly low frequency with time as the original findings become universally accepted within the academic community and therefore, no longer routinely referenced in published articles. Furthermore, the process of accrual of citations is a slow process and takes several years. In an effort to circumvent this issue, other methods of assessing research impact more rapidly have been developed recently and are known as alternative metrics or “Altmetrics”. These are based on utilisation of alternative information sources that are also considered as independent or surrogate markers of impact such as frequency of online article downloads, discussion in social media platforms, use in consensus or guideline development and mention in patent applications amongst others. One of the most popular platforms that is currently favoured by many journals to assess these alternative metrics is the Altmetric Attention Score (AAS) developed by Altmetric LLP. The AAS is a relatively new concept initiated in 2011 and is derived from algorithms which assess the distribution and influence of a scientific paper through social media and until recently was known simply as the ‘Altmetric Score’ [5]. There is an urgent need to conduct research that helps to assess the utility and value of Altmetric indices over more traditional indices of academic impact such as citation number (bibliometric index), journal impact factor and level of evidence of the publication.
The primary aim of this study is to identify and perform a citation rank analysis of the 100 most cited publications that have influenced the understanding of LAGB. The secondary aim is to analyse the correlation between Total Citation Count (TCC), Level Of Evidence (LOE) and AAS of the listed publications to gain a further understanding of the dynamics between these metrics and assess the reliability of AAS as an index of academic impact.
Methods
A search of the Thomson Reuters Web of Science citation indexing database and research platform was performed using the search terms ((laparo* and adjust* and gastr* and band*) OR (LAGB or L.A.G.B.)) AND ALL FIELDS: ((endoscop* or remov* or complicat*)). The returned dataset was filtered to include only English language and full manuscripts and sorted using the TCC in descending order as per the method originally developed by Paladugu and colleagues [6]. Each manuscript was analysed to ensure that content was relevant to the study topic and the four articles were excluded as they were deemed not to have substantial content related to LAGB [7-10]. The 100 most cited manuscripts were subsequently analysed in detail and used to populate a database which included several data indices such as the publishing journal (name of journal, country of publication, 2018 impact factor and year of publication), authors (institutional affiliation and country) and article details (TCC, type of study, LOE and AAS). The quality of evidence contained within the articles was assessed and recorded according to the Oxford Evidence Based Medicine scoring system [11]. The ‘‘Altmetric it’’ application downloaded from the Altmetric.com website was used to generate Altmetric scores by utilising the journal article page containing the doi reference number [5].
Results
The Web of Science search returned 1,473 full-length, English language papers. Table 1 lists the 100 most cited of these papers: [12-109].
|
Rank |
Citations |
First author |
Rank |
Citations |
First Author |
|---|---|---|---|---|---|
|
1 |
962 |
Maggard, M |
51 |
121 |
Friedenberg, F K |
|
2 |
935 |
Dixon, J |
52 |
120 |
Fried M |
|
3 |
877 |
Flum, D R |
53 |
118 |
Nguyen, N T |
|
4 |
750 |
Angrisani, L |
54 |
117 |
Dargent, J |
|
5 |
678 |
Colquitt, J L |
55 |
116 |
Mognol, P |
|
6 |
662 |
Chang, S |
56 |
114 |
Black, J A |
|
7 |
551 |
Picot, J |
57 |
114 |
Chevallier, J |
|
8 |
439 |
Himpens, J |
58 |
114 |
Favretti, F |
|
9 |
395 |
Colquitt, J L |
59 |
112 |
Angrisani, L |
|
10 |
325 |
O’Brien, P E |
60 |
112 |
Busetto, L |
|
11 |
310 |
Tice, J A |
61 |
111 |
Trastulli, S |
|
12 |
280 |
Maggard, M |
62 |
107 |
O’Brien, P E |
|
13 |
272 |
Chevallier, J |
63 |
106 |
Paulus, G F |
|
14 |
262 |
Demaria, E J |
64 |
106 |
O’Brien, P E |
|
15 |
255 |
Rubino, F |
65 |
105 |
Fielding, G A |
|
16 |
250 |
Elder, K A |
66 |
103 |
Parikh, M S |
|
17 |
247 |
Angrisani, L |
67 |
101 |
Pontiroli, A E |
|
18 |
244 |
Birkmeyer, N J O |
68 |
101 |
Busetto, L |
|
19 |
241 |
O’Brien, P E |
69 |
100 |
Pontiroli, A E |
|
20 |
238 |
Gagner, M |
70 |
100 |
Miller, K |
|
21 |
224 |
Deitel, M |
71 |
99 |
Cunneen, S A |
|
22 |
220 |
Sauerland, S |
72 |
98 |
Encinosa, W E |
|
23 |
219 |
Himpens, J |
73 |
97 |
Lancaster, R T |
|
24 |
217 |
Weiner, R |
74 |
97 |
Martikainen, T |
|
25 |
216 |
Demaria, E J |
75 |
97 |
Chelala, E |
|
26 |
215 |
Nocca, D |
76 |
96 |
Ponce, J |
|
27 |
214 |
Dixon, J |
77 |
94 |
Li, Vicky K M |
|
28 |
213 |
Belachew, M |
78 |
92 |
Frezza, E E |
|
29 |
206 |
Belachew, M |
79 |
91 |
Ahroni, J H |
|
30 |
205 |
Fisher, B L |
80 |
90 |
Steffen, R |
|
31 |
194 |
Shi, X |
81 |
90 |
Fielding, G A |
|
32 |
192 |
Abbatini, F |
82 |
90 |
Weiss, H G |
|
33 |
192 |
Belachew, M |
83 |
89 |
Wageningen, B V |
|
34 |
178 |
Favretti, F |
84 |
89 |
Ren, C J |
|
35 |
175 |
Lalor, P F |
85 |
86 |
Demaria, E J |
|
36 |
173 |
Carlin, Arthur M |
86 |
86 |
Ponce, Jaime |
|
37 |
172 |
Angrisani, L |
87 |
84 |
Ducarme, G |
|
38 |
169 |
Treadwell, Jonathan R |
88 |
84 |
Forsell, P |
|
39 |
161 |
Nguyen, Ninh T |
89 |
83 |
Nguyen, Ninh T |
|
40 |
155 |
Lee, Crystine M |
90 |
83 |
Bernante, Paolo |
|
41 |
139 |
Inge, Thomas H |
91 |
83 |
Frigg, Arno |
|
42 |
139 |
Pontiroli, Antonio E |
92 |
82 |
Parikh, Manish S |
|
43 |
134 |
Zinzindohoue, Franck |
93 |
81 |
Cottam, Daniel R |
|
44 |
132 |
Favretti, F |
94 |
81 |
Niville, E |
|
45 |
131 |
Franco Juan V A |
95 |
80 |
Vertruyen, Marc |
|
46 |
131 |
Biertho, Laurent |
96 |
80 |
Rubenstein, Richard B |
|
47 |
129 |
Sugerman, H J |
97 |
79 |
Nadler, Evan P |
|
48 |
127 |
Westling, A |
98 |
79 |
Ren, Christine J |
|
49 |
125 |
Spivak, Hadar |
99 |
78 |
Gumbs, Andrew A |
|
50 |
123 |
Colquitt, Jill L |
100 |
78 |
Skull, A J |
|
Abbrevation: 1LAGB = Laparoscopic Adjustable Gastric Banding |
|||||
Table 1: The top 100 most cited papers in LAGB1.
The total number of citations ranged from 78 for Skull et al. (Laparoscopic adjustable banding in pregnancy: Safety, patient tolerance and effect on obesity-related pregnancy outcomes) to 962 for Maggard et al. (Meta-analysis: Surgical Treatment of Obesity) (Table 1). The median citation count was 122 (interquartile range (IQR): 96.75 – 215.25) and this was not normally distributed (Skewness=2.86, Kurtosis=8.29). The oldest article within this top 100 list was a report on LAGB published in 1994 by Belachew et al. titled ‘Laparoscopic adjustable silicone gastric banding in the treatment of morbid-obesity – A preliminary report’. The most recent paper titled ‘Bariatric surgery for obesity and metabolic disorders: state of the art’ was published in 2017 by Nguyen et al.
|
Journal Title |
Impact factor (2018) |
Number of articles in the top 100 |
Total number of |
|---|---|---|---|
|
American Journal of Gastroenterology |
10.24 |
1 |
121 |
|
American Journal of Surgery |
2.2 |
5 |
581 |
|
Annals of internal medicine |
19.32 |
1 |
962 |
|
Annals of Surgery |
9.48 |
10 |
1678 |
|
Annual Review of Medicine |
9.5 |
1 |
255 |
|
Archives of Surgery |
- |
1 |
219 |
|
Diabetes Care |
13.4 |
2 |
314 |
|
Gastroenterology |
19.23 |
1 |
250 |
|
Health Technology Assessment |
3.9 |
1 |
551 |
|
International Journal of Gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics |
1.67 |
1 |
84 |
|
Journal of Clinical Endocrinology and Metabolism |
5.61 |
1 |
139 |
|
Journal of Laparoendoscopic Advanced Surgical Techniques. Part A |
1.32 |
2 |
185 |
|
Journal of the American College of Surgeons |
4.45 |
3 |
320 |
|
Journal of Pediatric Surgery |
2.1 |
1 |
79 |
|
Journal of the American Medical Association |
51.27 |
4 |
2260 |
|
Journal of the American Medical Association – Pediatrics |
12 |
1 |
139 |
|
Medical Care |
3.8 |
1 |
98 |
|
Microbiology |
1.03 |
1 |
83 |
|
Nature Reviews: Gastroenterology and Hepatology |
23.57 |
1 |
83 |
|
New England Journal of Medicine |
70.67 |
1 |
877 |
|
Obesity Surgery |
3.6 |
36 |
5633 |
|
Surgery for Obesity and Related Diseases: Official Journal for the American Society for Bariatric Surgery |
3.16 |
7 |
462 |
|
Surgery Today |
2.08 |
1 |
92 |
|
Surgical Endoscopy |
3.21 |
10 |
1462 |
|
The American Journal of Medicine |
4.76 |
1 |
310 |
|
The British Journal of Surgery |
5.57 |
1 |
241 |
|
The Cochrane Database of Systematic Reviews |
7.76 |
3 |
1197 |
|
World Journal of Surgery |
2.77 |
1 |
192 |
|
Abbrevation: 1LAGB = Laparoscopic Adjustable Gastric Banding |
|||
Table 2: Journals with the top 100 most cited LAGB1 articles.
The 100 most significant papers spanning between 1994 and 2017 were published across a spectrum of 28 journals with the number of published articles per journal ranging from 1 to 36 (Table 2). The journal “Obesity Surgery” published the highest number of papers within the top 100 and also, had the highest cumulative TCC amongst all journals (n=36, 5633 citations). Amongst this list of the top 100 articles, 11 publications were in 2002 making it the most frequent year of publication. Most articles were published in journals which had an impact factor (IF) greater than 3 with only 11 articles published in journals with a lesser IF.
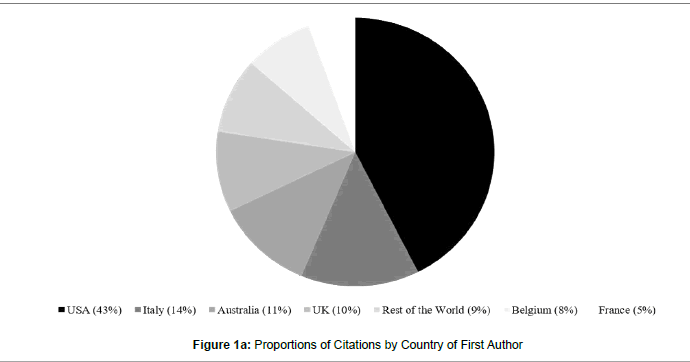
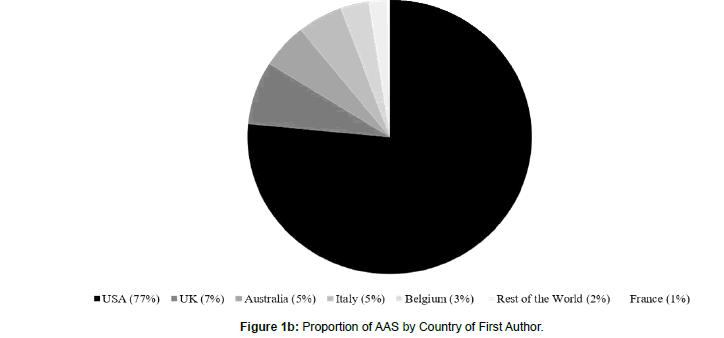
The country with the most publications when first author affiliation was considered was the United States of America (USA) with 41 publications and, incidentally, USA also had the highest cumulative TCC at 8,174 (43% of total citations) (Figure 1). This was followed by Italy with 15 publications. Analysis of senior author affiliation revealed that the country with the most publications and the highest cumulative TCC was also USA (n=42, 5,954 citations, 31% of total citations) followed by Italy (n=17; 5404 citations). The country with the highest AAS by first author affiliation (1,350, 77% of total AAS) as well as second author affiliation (1,350; 76% of total AAS scores) was also USA. Monash University and its affiliated institutions had the highest number of articles in the top 100 with 6 publications.
There were two first authors with the highest number of publications in the top 100 with 4 articles each - Paul E. O’Brien who is affiliated with Monash University, and L. Angrisani who is affiliated with S. Giovanni Bosco Hospital and the Fondazione Institute for Spreading and Valorisation of Scientific Culture, they both had 4 publications each. L. Angrisani also had the most citations overall as first author with 1,281 citations. The senior author with the highest number of publications in the top 100 with 4 articles was G. Enzi who is affiliated with the University of Padova and the University of Padua. The senior author with the highest number of citations was Paul G. Shekelle who is affiliated with the RAND Health Division, California with 1,242 citations.
The citation rate index (CRI) was also calculated in order to control for the fact that older papers would have had more time to accrue citations. The CRI for the top 10 articles ranged from 187.5 for Angrisani et al. (Bariatric Surgery Worldwide, 2013) to 35.908 for Colquitt et al. (Surgery for Obesity, 2009) (Table 3). The highest 5 CRIs came from articles published between 2009 and 2017. The countries that published the highest number of articles in the top 10 CRI were UK and USA with 3 articles each.
|
Rank
|
Citation rate |
Journal |
First author |
Senior author |
Title |
Institution (first author) |
Country |
|---|---|---|---|---|---|---|---|
|
1 |
187.5 |
Obesity Surgery |
Angrisani, L |
Scopinaro, N |
Bariatric Surgery Worldwide 2013 |
University of Genoa |
Italy |
|
2 |
135.6 |
The Cochrane Database of Systematic Reviews |
Colquitt. J.L |
Frampton, G.K |
Surgery for Weight Loss in Adults |
University of Southampton |
UK |
|
3 |
123.5 |
Obesity Surgery |
Angrisani, L |
Scorpinaro, N |
Bariatric Surgery and Endoluminal Procedures: IFSO Worldwide Survey 2014 |
University of Genoa |
Italy |
|
4 |
110.332 |
Journal of the American Medical Association |
Chang, S |
Colditz, G.A |
The Effectiveness and risks of Bariatric Surgery An Updated Systematic Review and Meta-analysis, 2003-2012 |
Washington University |
USA |
|
5 |
87.7 |
University of Washington |
Flum, D.R |
Yanovski, S.Z |
Perioperative Safety in the Longitudinal Assessment of Bariatric Surgery |
National Institute of Diabetes and Digestive and Kidney Diseases |
USA |
|
6 |
77.917 |
Journal of the American Medical Association |
Dixon, J |
Anderson, M |
Adjustable gastric banding and conventional therapy for type 2 diabetes - A randomized controlled trial |
Monash University |
Australia |
|
7 |
64.132 |
Annals of Internal Medicine |
Maggard, M |
Shekelle, P.G |
Meta-analysis: Surgical Treatment of Obesity |
Southern California Evidence-Based Practice Center |
USA |
|
8 |
55.1 |
Health Technology Assessment |
Picot, J |
Clegg, A.J |
The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation |
University of Southampton, UK. |
UK |
|
9 |
46.429 |
Annals of Surgery |
O’Brien, P.E |
Brown, W.A |
Long-Term Outcomes After Bariatric Surgery Fifteen-Year Follow-Up of Adjustable Gastric Banding and a Systematic Review of the Bariatric Surgical Literature |
Monash University |
Australia |
|
10 |
35.908 |
The Cochrane Database of Systematic Reviews |
Colquitt, J.L |
Clegg, A.J |
Surgery for obesity |
University of Southampton |
UK |
|
Abbrevation: 1CRI = Citation Rate Index |
|||||||
Table 3: Top 10 articles with the highest CRI1.
The articles with the five highest AAS were published between 2009 and 2017 with the highest score being 413 (Perioperative Safety in the Longitudinal Assessment of Bariatric Surgery, Flum et al) (Table 4). Altmetric scores ranged between 0 and 413 (median = 0, IQR: 0 – 10.25) with 54 articles scoring 0 for AAS. The article with the highest AAS was (Perioperative Safety in the Longitudinal Assessment of Bariatric Surgery). The USA had the most articles in the top 10 AAS with 5 publications. 93 papers dealt with complications of LAGB making this the most extensively studied topic in this review followed by weight loss which was investigated in 93 papers (Table 5). Long term prognosis or outcomes following LAGB was the least discussed topic with only 4 articles dealing with this topic.
|
Rank |
AAS |
First author |
Senior author |
Title |
Institution (first author) |
Country |
|---|---|---|---|---|---|---|
|
1 |
413 |
Flum, D.R |
Yanovski, S.Z |
Perioperative Safety in the Longitudinal Assessment of Bariatric Surgery. |
University of Washington |
USA |
|
2 |
382 |
Encinosa, W.E |
Steiner, C.A |
Recent Improvements in Bariatric Surgery Outcomes |
Center for Delivery, Organization, and Markets, Agency for Healthcare Research and Quality, USA |
USA |
|
3 |
139 |
Chang, S |
Colditz, G.A |
The Effectiveness and Risks of Bariatric Surgery An Updated Systematic Review and Meta-analysis, 2003-2012 |
Washington University |
USA |
|
4 |
132 |
Inge, T.H |
Buncher, C.R |
Perioperative Outcomes of Adolescents Undergoing Bariatric Surgery The Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) Study |
Cincinnati Children's Hospital Medical Center |
USA |
|
5 |
94 |
Nguyen, N.T |
Varela, J.E |
Bariatric surgery for obesity and metabolic disorders: state of the art |
University of California |
USA |
|
6 |
66 |
Colquitt, J.L |
Frampton, G.K |
Surgery for Weight Loss in Adults |
University of Southampton |
UK |
|
7 |
49 |
Himpens, J |
Dapri, G |
Long-term Outcomes of Laparoscopic Adjustable Gastric Banding |
Saint Pierre University Hospital |
Belgium |
|
8 |
44 |
Dixon, J |
Anderson, M |
Adjustable gastric banding and conventional therapy for type 2 diabetes - A randomized controlled trial |
Monash University |
Australia |
|
9 |
40 |
O’Brien, P.E |
Brown, W |
Long-Term Outcomes After Bariatric Surgery Fifteen-Year Follow-Up of Adjustable Gastric Banding and a Systematic Review of the Bariatric Surgical Literature |
Monash University |
Australia |
|
10 |
33 |
Angrisani, L |
Scopinaro, N |
Bariatric Surgery Worldwide 2013 |
General and Endoscopic Surgery Unit Bosco Hospital |
Italy |
|
Abbrevation: 1AAS = Altmetric Attention Score |
||||||
Table 4: Top 10 articles with the highest AAS1.
|
S. No |
Topic / Subject area |
Number of papers |
|---|---|---|
|
1 |
Complications |
93 |
|
2 |
Weight Loss |
91 |
|
3 |
Improvement of Co-morbidities |
69 |
|
4 |
Indications |
43 |
|
5 |
Long Term Prognosis or Outcomes |
4 |
Table 5: Most frequently referenced topics.
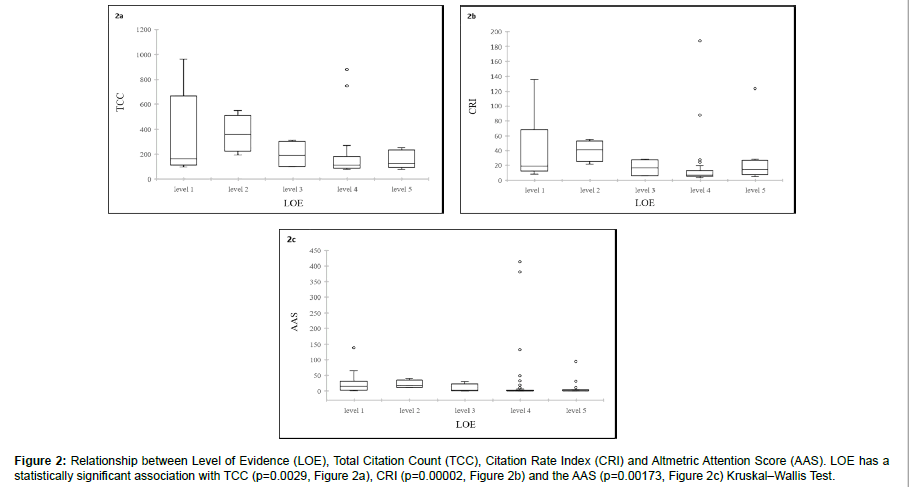
Evidence levels for the top 100 articles were scored using the Oxford Evidence Based scoring system [11]. 14 papers were classed as providing level 1 evidence, 4 papers were level 2 evidences and level 3 evidences each, 62 papers were level 4 evidence and 16 papers were level 5 evidence. There was a statistically significant difference between the LOE and TCC (p=0.0029) (Figure 2a). The median number of citations received at each evidence level was level 1 165 (IQR 115.25-606.25), level 2 460 (IQR 292.25-434), level 3 190.5 (IQR 100.75-287.5), level 4 112 (IQR 89.25-177.25) and level 5 126 (IQR 103.25-227.5). There was a statistically significant difference between LOE and CRI (p=0.00002, Figure 2b). The median CRI at each evidence level was level 1 18.75 (IQR 13.75-49.75), level 2 3.05 (IQR 26.51-38.54), level 3 16.30 (IQR 6.92-41.02), level 4 7.18 (IQR 5.88-12.37) and level 5 13.33 (IQR 8.90- 21.51). There was also a statistically significant difference between LOE and the AAS (p=0.00173, Figure 2c). The median AAS received at each evidence level was level 1 26 (IQR 6.5-43), level 2 8.5 (IQR 0.75-20), level 3 1.5 (IQR 0-14.5), level 4 0 (IQR 0-3.75) and level 5 0 (IQR 0-1).
Figure 2: Relationship between Level of Evidence (LOE), Total Citation Count (TCC), Citation Rate Index (CRI) and Altmetric Attention Score (AAS). LOE has a statistically significant association with TCC (p=0.0029, Figure 2a), CRI (p=0.00002, Figure 2b) and the AAS (p=0.00173, Figure 2c) Kruskal–Wallis Test.
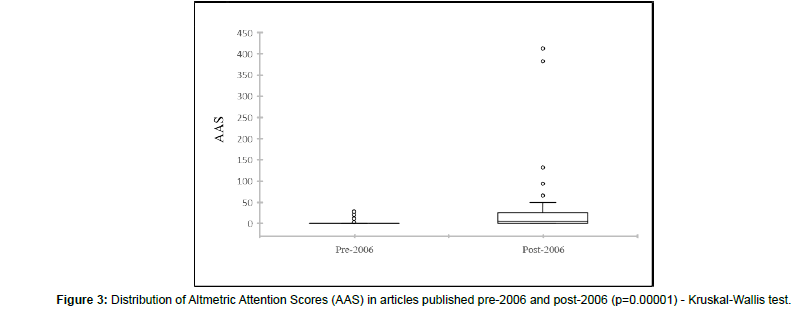
Articles published from the year 2006 onwards had a significantly higher AAS compared to articles published prior to 2006 with median of 5.5 (IQR 0-23.25) and 0 (IQR 0-0) respectively (p = 0.00001) (Figure 3). The AAS of articles which were published both prior to 2006 did not have a significant correlation with the TCC (r = 0.2332, p = 0.1108) (Figure 4a) but was positively correlated with the CRI (r =0.3194, p =0.0268) (Figure 5a). The AAS of articles which were published following 2006 did not have a significant correlation with either the TCC (r = 0.5274, p = 5.8596, Figure 4b) or the CRI (r = 0.5274, p = 5.8596) (Figure 5b).
Discussion
Bariatric Surgery is now well established as an effective treatment for morbid obesity and associated co-morbidities [110]. However, there is still ongoing debate regarding the exact indications for different bariatric operations and their long term outcomes. LAGB is one of the most widely used procedures worldwide for the treatment of morbid obesity [1]. There has been widespread interest in recent years regarding LAGB and, in particular, the indications, weight loss results, effect on co-morbidities, complications and long-term results following LAGB. It is therefore, not surprising, that the four most widely studied topics amongst the top 100 articles featured in this review include complications, weight loss, improvement of co-morbidities and indications of LAGB. This highlights that a bibliometric analysis is a very useful way to ascertain the most relevant and important topics in an area of interest as well as providing the interested reader with a ready reckoner of the most influential manuscripts in that setting.
The traditional gold standard for assessing the impact of a published manuscript has been the TCC whilst an important measure of the quality of the research is the LOE it provides. Hence, bibliometrics which utilises these metrics for analysis and comparison is considered to be a very useful tool. Our study has shown a significant difference between the LOE and TCC as well as CRI. Studies with level 1 & 2 evidences have overall higher TCC and CRI compared to studies with level 4 & 5 evidences. Whist this is not unexpected, it does demonstrate that TCC and CRI are both useful metrics to assess academic impact and studies with superior evidence quality attract more citations. In contrast, Powell et al. did not note any correlation between LOE and TCC in their study and noted that this was a surprising result in their opinion. They attributed this to the challenges inherent in linking impact with citation and research quality but an alternative explanation could be the lead time bias inherent in measuring citation count [111].
An interesting finding of this study is that 89 of the 100 articles in this study have been published since 2000. This is perhaps not surprising because surgery for morbid obesity is still a field in its relative infancy and indeed most of the major developments have taken place during this century. However, the relatively short time period that spans most of the articles in this study makes this study uniquely robust in assessing the utility of AAS as an alternative index to other bibliometric indices. All the studies comparing bibliometric indices and AAS so far have been limited by the fact that a significant proportion of their articles were published before 2000 and, therefore, inherently biased against AAS as a measure of impact. This bias arises because most social media and other platforms included in the AAS scoring algorithm have evolved after 2000 such as Twitter in 2006 and Mendeley in 2007. In fact, our study demonstrates this bias clearly and shows a significantly lower AAS for articles published pre-2006 compared with articles post- 2006. Our study also shows that AAS correlates with LOE in a trend that is similar to TCC and CRI. This shows that AAS can be used as an alternative index to citation count and CRI as a measure of article impact. Previous studies have also demonstrated correlation between AAS and TCC [112]. Another finding that supports the credibility of AAS as an alternative metric to TCC and CRI is the fact that 60% of the publications all three lists of top 10 articles ranked on basis of the highest number of citations, CRIs and ASS were the same [Tables 1, 3 & 4].
Another interesting finding of note is that there is no significant difference in the association between AAS and TCC or CRI in post- 2006 articles (Figure 4a and 5a) suggesting that perhaps CRI is a redundant index and that TCC alone should suffice. However, in pre-2006 papers AAS is significantly correlated with CRI but not TCC (Figure 4b and 5b). The explanation of this perhaps lies in the phenomenon of lead-time bias or, more accurately, the lack of it in the post-2006 articles in this study. It is likely that articles published early in the 2006-2020 period have not had sufficient time to accrue enough citations compared to articles published more recently to generate a lead-time bias. It is likely that if this study is repeated after a decade or two, then divergent results will be noted between TCC and CRI in the post-2006 cohort.
This study has some limitations due to deficiencies intrinsic to the chosen study design as well as weaknesses inherent in the bibliometric indices. Firstly, citation counts and CRI are influenced by several types of bias such as language bias, institutional bias, and publication bias amongst others. In this study the language bias resulted in high numbers of English speaking countries being represented, particularly publications from USA which has been seen previously [111,113]. Secondly, the search strategy used to identify the top 100 articles invariably includes articles that are not relevant and can also exclude high impact articles. We noted that our search strategy included 4 articles that were eventually considered as being not relevant. Thirdly, as discussed earlier, the use of AAS as a metric is biased by the fact that articles published prior to early 2000s are significantly underrepresented in social media and other online platforms used to calculate the AAS. Finally, a top 100 analysis invariably limits the total data points available for analysis across different sub-groups to exactly 100 and the statistical results should be interpreted whilst bearing this in mind.
Conclusion
By analyzing the most influential articles that have shaped our understanding of LAGB, this study serves as a reference of the highest impact articles that have shaped the role of LAGB as an operation for morbid obesity whilst also serving as a guide for future research. Our study shows that AAS is a valid metric for assessing the impact of a study along with traditional metrics such as TCC and CRI. However, AAS is not reliable for articles published before 2006. Furthermore, the LOE of a study is significantly associated with all three indices of study impact including TCC, CRI and AAS.
References
- Kang JH, Le QA (2017) Effectiveness of bariatric surgical procedures: A systematic review and network meta-analysis of randomized controlled trials. Medicine (Baltimore) 96: e8632.
- Lefaivre KA, Shadgan B, O’Brien PJ (2011) 100 Most Cited Articles in Orthopaedic Surgery. Clin Orthop Relat Res 469: 1487-97.
- Borgman C, Furner J (2005) Scholarly Communication and Bibliometrics. ARIST. 1: 02–72.
- McCain KW (2014) Assessing obliteration by incorporation in a full-text database:JSTOR, Economics, and the concept of “bounded rationality.†Scientometrics  101: 1445-59.
- Altmetric [Internet]. Available from: https://www.altmetric.com/?s=citation&cPfyHZwpXsjq=lHFnWgkybEAC&jbvcfox-p_ZCNs=a4prhQSl_I%5DiTq&cPfyHZwpXsjq=lHFnWgkybEAC&jbvcfox-p_ZCNs=a4prhQSl_I%5DiTq
- Iqbal U, Rehan A, Akmal M, Jamali M, Iqbal A, et al. (2019) Top 100 most influential articles in the field of myeloid neoplasms: A bibliometric study. Acta Haematol 1: 68-78.
- Roa PE, Kaidar-Person O, Pinto D, Cho M, Szomstein S, Â et al. (2006) Laparoscopic sleeve gastrectomy as treatment for morbid obesity: Technique and short-term outcome. Obes Surg 16: 1323-6.
- Gagner M, Deitel M, Erickson AL, Crosby RD (2013) Survey on laparoscopic sleeve gastrectomy (LSG) at the fourth international consensus summit on sleeve gastrectomy. Obes Surg 23: 2013–17.
- Parikh MS, Laker S, Weiner M, Hajiseyedjavadi O, Ren CJ (2006) Objective comparison of complications resulting from laparoscopic bariatric procedures. J Am Coll Surg 202: 252-61.
- Bernante P, Foletto M, Busetto L, Pomerri F, Pesenti FF, et al. (2006) Feasibility of laparoscopic sleeve gastrectomy as a revision procedure for prior laparoscopic gastric banding. Obes Surg 16: 1327-30.
- OCEBM Levels of Evidence — Centre for Evidence-Based Medicine (CEBM), University of Oxford . Available from: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence
- Maggard MA, Shugarman LR, Suttorp M, Maglione M, Sugerman HJ, et al. (2005) Meta-analysis: Surgical treatment of Obesity. Ann Intern Med 142: 547-59.
- Dixon JB, O’Brien PE, Playfair J, Chapman L, Schachter LM, et al. (2008) Adjustable gastric banding and conventional therapy for type 2 Diabetes A randomized controlled trial. JAMA 299: 316-23.
- Flum DR, Belle SH, Berk P, Chapman W, Courcoulas A, et al. (2009) Peri-operative safety in the longitudinal assessment of bariatric surgery. The longitudinal assessment of bariatric surgery (LABS) consortium. N Engl J Med 361: 445-54.
- Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, et al. (2015) Bariatric surgery Worldwide 2013. Obes Surg 25: 1822-32.
- Colquitt JL, Pickett K, Loveman E, Frampton GK (2014) Surgery for weight loss in adults. Cochrane Database Syst Rev 2014.
- Chang SH, Stoll CRT, Song J, Varela JE, Eagon CJ, et al. (2014) The effectiveness and risks of bariatric surgery an updated systematic review and meta-analysis, 2003-2012. JAMA Surg 149: 275-87.
- Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, et al. (2009) The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: A systematic review and economic evaluation. Health Technol Assess 13:1-190.
- Himpens J, Dapri G, Cadière GB (2006) A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: Results after 1 and 3 years. Obes Surg 16: 1450-56.
- Colquitt JL, Picot J, Loveman E CA (2019) Surgery for obesity. Med (United Kingdom) 47: 184-7.
- O’Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA (2013) Long-term outcomes after bariatric surgery: Fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 257: 87-94.
- Tice JA, Karliner L, Walsh J, Petersen AJ, Feldman MD (2008) Gastric Banding or Bypass? A systematic review comparing the two most popular bariatric procedures. Am J Med 121: 885-93.
- Maggard MA, Yermilov I, Li Z, Maglione M, Newberry S, et al. (2008) Pregnancy and fertility following Bariatric Surgery: A systematic review. JAMA 300: 2286-96.
- Chevallier JM, Zinzindohoué F, Douard R, Blanche JP, Berta JL, et al. (2004) Complications after laparoscopic adjustable gastric banding for morbid obesity: Experience with 1,000 patients over 7 years. Obes Surg 14: 407-14.
- DeMaria EJ, Sugerman HJ, Meador JG, Doty JM, Kellum JM, et al. (2001) High failure rate after laparoscopic adjustable silicone gastric banding for treatment of morbid obesity. Ann Surg 233: 809-18.
- Rubino F, Schauer PR, Kaplan LM, Cummings DE (2010) Metabolic Surgery to Treat Type 2 Diabetes: Clinical Outcomes and Mechanisms of Action. Annu Rev Med 61: 393-411.
- Francesco Rubino, Philip R Schauer, Lee M Kaplan, David E Cummings (2010) Metabolic Surgery to Treat Type 2 Diabetes: Clinical Outcomes and Mechanisms of Action. Annual Review of Medicine 61:393-411
- Angrisani L, Santonicola A, Iovino P, Vitiello A, Zundel N, et al. (2017) Bariatric Surgery and endoluminal procedures: IFSO Worldwide survey 2014. Obes Surg 27: 2279-89.
- Birkmeyer NJO, Dimick JB, Share D, Hawasli A, English WJ, et al. (2010) Hospital Complication Rates With Bariatric Surgery in Michigan. JAMAÂ 304: 435-42.
- O’Brien PE, Brown WA, Smith A, McMurrick PJ, Stephens M (1999) Prospective study of a laparoscopically placed, adjustable gastric band in the treatment of morbid obesity. Br J Surg 86: 113-18.
- Gagner M, Deitel M, Kalberer TL, Erickson AL, Crosby RD (2009) The Second International Consensus Summit for Sleeve Gastrectomy, March 19-21, 2009. Surg Obes Relat Dis 5: 476-85.
- Deitel M, Gagner M, Erickson AL, Crosby RD (2011) Third International Summit: Current status of sleeve gastrectomy. Surg Obes Relat Dis 7: 749-59.
- Sauerland S, Angrisani L, Belachew M, Chevallier JM, Favretti F, et al. (2005) Obesity surgery: Evidence-based guidelines of the European Association for Endoscopic Surgery (E.A.E.S.). Surg Endosc Other Interv Tech 19: 200-21.
- Himpens J, Cadière G-B, Bazi M, Vouche M, Cadière B, et al. (2011) Long-term Outcomes of Laparoscopic Adjustable Gastric Banding. Arch Surg 146: 802-7.
- Weiner R, Blanco-Engert R, Weiner S, Matkowitz R, Schaefer L, et al. (2003) Outcome after laparoscopic adjustable gastric banding - 8 Years experience. Obes Surg 13: 427-34.
- DeMaria EJ, Pate V, Warthen M, Winegar DA (2010) Baseline data from American society for metabolic and bariatric surgery-designated bariatric surgery centers of excellence using the bariatric outcomes longitudinal database. Surg Obes Relat Dis 6: 347-55.
- Nocca D, Krawczykowsky D, Bomans B, Noël P, Picot MC, et al. (2008) A prospective multicenter study of 163 sleeve gastrectomies: Results at 1 and 2 years. Obes Surg 18: 560-5.
- Dixon, John B, O’Brien PE (2002) Health Outcomes of Severely Obese Type 2 Diabetic Subjects 1 Year After. Emerg Treat Technol 25.
- Belachew M, Belva PH, Desaive C (2002) Long-term results of laparoscopic adjustable gastric banding for the treatment of morbid obesity. Obes Surg 12: 564-8.
- Belachew M, Legrand MJ, Defechereux TH, Burtheret MP, Jacquet N (1994) Laparoscopic adjustable silicone gastric banding in the treatment of morbid obesity - A preliminary report. Surg Endosc 8: 1354-6.
- Fisher BL, Schauer P (2002) Medical and surgical options in the treatment of severe obesity. Am J Surg 184: S9-16.
- Shi X, Karmali S, Sharma AM, Birch DW (2010) A review of Laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg 20: 1171-7.
- Abbatini F, Rizzello M, Casella G, Alessandri G, Capoccia D, et al. (2010) Long-term effects of laparoscopic sleeve gastrectomy, gastric bypass, and adjustable gastric banding on type 2 diabetes. Surg Endosc 24: 1005-10.
- Belachew M, Legrand M, Vincent V, Lismonde M, Le Docte N, et al. (1998) Laparoscopic adjustable gastric banding. World J Surg 22: 955-63.
- Favretti F, Segato G, Ashton D, Busetto L, De Luca M, et al. (2007) Laparoscopic adjustable gastric banding in 1,791 consecutive obese patients: 12-Year results. Obes Surg 17: 168-75.
- Lalor PF, Tucker ON, Szomstein S, Rosenthal RJ (2008) Complications after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis 4: 33-8.
- Carlin AM, Zeni TM, English WJ, Hawasli AA, Genaw JA, et al. (2013) The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann Surg 257: 791-7.
- Angrisani L, Lorenzo M, Borrelli V (2007) Laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass: 5-year results of a prospective randomized trial. Surg Obes Relat Dis 3: 127-32.
- Treadwell JR, Sun F, Schoelles K (2008) Systematic review and meta-analysis of bariatric surgery for pediatric obesity. Ann Surg 248: 763-76.
- Nguyen NT, Slone JA, Nguyen XMT, Hartman JS, Hoyt DB (2009) A prospective randomized trial of laparoscopic gastric bypass versus laparoscopic adjustable gastric banding for the treatment of morbid obesity: Outcomes, quality of life, and costs. Ann Surg 250: 631-9.
- Lee CM, Cirangle PT, Jossart GH (2007) Vertical gastrectomy for morbid obesity in 216 patients: Report of two-year results. Surg Endosc 21: 1810-16.
- Inge T.H, Zeller M.H, Jenkins T.M, Helmrath M, Brandt M.L, et al. (2014) Perioperative Outcomes of Adolescents Undergoing Baratric Surgery: The Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) Study. JAMA Pediatr 168: 47-53.
- Pontiroli AE, Pizzocri P, Librenti MC, Vedani P, Marchi M, Â et al. (2002) Laparoscopic adjustable gastric banding for the treatment of morbid (grade 3) obesity and its metabolic complications: A three-year study. J Clin Endocrinol Metab 87: 3555-61.
- Zinzindohoue F, Chevallier J-M, Douard R, Elian N, Ferraz J-M BJ-P, et al. (2003) Laparoscopic gastric banding: A minimally invasive surgical treatment for morbid obesity: Prospective study of 500 consecutive patients. Ann Surg 237: 1-9.
- Favretti F, Cadiere GB, Segato G, Himpens J, Busetto L, et al. (1997) Laparoscopic adjustable silicone gastric banding (Lap-Band®): How to avoid complications. Obes Surg 7: 352-8.
- Franco JVA, Ruiz PA, Palermo M, Gagner M (2011) A review of studies comparing three laparoscopic procedures in bariatric surgery: Sleeve gastrectomy, roux-en-y gastric bypass and adjustable gastric banding. Obes Surg 21: 1458-68.
- Biertho L, Steffen R, Ricklin T, Horber FF, Pomp A, et al. (2003) Laparoscopic gastric bypass versus laparoscopic adjustable gastric banding: A comparative study of 1,200 cases. J Am Coll Surg 197: 536-45.
- Sugerman HJ, Felton WL, Sismanis A, Kellum JM, DeMaria EJ, et al. (1999) Gastric surgery for pseudotumor cerebri associated with severe obesity. Ann Surg 229: 634-42.
- Westling A, Gustavsson S (1998) Silicone-Adjustable Gastric Banding: Disappointing Results. Obes Surg 8: 467-74.
- Spivak H, Hewitt MF, Onn A, Half EE (2005) Weight loss and improvement of obesity-related illness in 500 U.S. patients following laparoscopic adjustable gastric banding procedure. Am J Surg 189: 27-32.
- Colquitt J, Clegg A, Loveman E, Royle P, Sidhu MK (2005) Surgery for morbid obesity. Cochrane database Syst Rev 4: CD003641.
- Friedenberg FK, Xanthopoulos M, Foster GD, Richter JE (2008) The association between gastroesophageal reflux disease and obesity. Am J Gastroenterol 103: 2111-22.
- Fried M, Ribaric G, Buchwald JN, Svacina S, Dolezalova K, et al. (2010) Metabolic surgery for the treatment of type 2 diabetes in patients with BMI <35 kg/m2: An integrative review of early studies. Obes Surg 20: 776-90.
- Nguyen NT, Hinojosa MW, Smith BR, Reavis KM (2008) Single laparoscopic incision transabdominal (SLIT) surgery-adjustable gastric banding: A novel minimally invasive surgical approach. Obes Surg 18: 1628-31.
- Dargent J (1999) Laparoscopic adjustable gastric banding: Lessons from the first 500 patients in a single institution. Obes Surg 9: 446-52.
- Mognol P, Chosidow D, Marmuse JP (2004) Laparoscopic conversion of laparoscopic gastric banding to Roux-en-Y gastric bypass: A review of 70 patients. Obes Surg 14: 1349-53.
- Black JA, White B, Viner RM, Simmons RK (2013) Bariatric surgery for obese children and adolescents: A systematic review and meta-analysis. Obes Rev 14: 634-44.
- Chevallier JM, Paita M, Rodde-Dunet MH, Marty M, Nogues F,  et al. (2007) Predictive factors of outcome after gastric banding: A nationwide survey on the role of center activity and patients’ behavior. Ann Surg 246: 1034-39.
- Favretti F, Cadière GB, Segato G, Himpens J, De Luca M, et al. (2002) Laparoscopic banding: Selection and technique in 830 patients. Obes Surg 12: 385-90.
- Angrisani L, Furbetta F, Doldi SB, Basso N, Lucchese M,  et al. (2003) Lap Band® adjustable gastric banding system: The Italian experience with 1863 patients operated on 6 years. Surg Endosc Other Interv Tech 17: 409-12.
- Busetto L, Segato G, De Marchi F, Foletto M, De Luca M, Â et al. (2002) Outcome predictors in morbidly obese recipients of an adjustable gastric band. Obes Surg 12: 83-92.
- Trastulli S, Desiderio J, Guarino S, Cirocchi R, Scalercio V, et al. (2013) Laparoscopic sleeve gastrectomy compared with other bariatric surgical procedures: A systematic review of randomized trials. Surg Obes Relat Dis 9: 816-29.
- O’Brien PE, Dixon JB (2002) Weight loss and early and late complications - The international experience. Am J Surg 184: S42-45.
- Paulus GF, de Vaan LEG, Verdam FJ, Bouvy ND, Ambergen TAW, et al. (2015) Bariatric Surgery in Morbidly Obese Adolescents: a Systematic Review and Meta-analysis. Obes Surg 25: 860-78.
- O’Brien PE, Dixon JB (2003) Lap-band®: Outcomes and results. J Laparoendosc Adv Surg Tech A 13: 265-70.
- Fielding GA, Rhodes M, Nathanson LK (1999) Laparoscopic gastric banding for morbid obesity: Surgical outcome in 335 cases. Surg Endosc 13: 550-4.
- Pontiroli AE, Fossati A, Vedani P, Fiorilli M, Folli F, et al. (2007) Post-surgery adherence to scheduled visits and compliance, more than personality disorders, predict outcome of bariatric restrictive surgery in morbidly obese patients. Obes Surg 17: 1492-97.
- Busetto L, Segato G, De Luca M, Bortolozzi E, Maccari T, et al. (2004) Preoperative weight loss by intragastric balloon in super-obese patients treated with laparoscopic gastric banding: A case-control study. Obes Surg 14: 671-6.
- Pontiroli, Antonio E, Franco, Folli, Paganelli, et al. (2005) Laparoscopic Gastric Banding Prevents Type 2 Diabetes and Arterial Hypertension and Induces Their Remission in Morbid Obesity. Diabetes Care 28: 22-4.
- Miller K, Hell E (1999) Laparoscopic adjustable gastric banding: A prospective 4-year follow-up study. Obes Surg 9: 183-7.
- Cunneen SA (2008) Review of meta-analytic comparisons of bariatric surgery with a focus on laparoscopic adjustable gastric banding. Surg Obes Relat Dis 4.
- Encinosa WE, Didem M, Bernard DM, CASCA (2006) Recent Improvements in Bariatric Surgery Outcomes. Med Care 47: 386-408.
- Lancaster RT, Hutter MM (2008) Bands and bypasses: 30-Day morbidity and mortality of bariatric surgical procedures as assessed by prospective, multi-center, risk-adjusted ACS-NSQIP data. Surg Endosc Other Interv Tech 22: 2554-63.
- Martikainen T, Pirinen E, Alhava E, Poikolainen E, Pääkkönen M,  et al. (2004) Long-term results, late complications and quality of life in a series of adjustable gastric banding. Obes Surg 14: 648-654.
- Chelala E, Cadiére GB, Favretti F, Himpens J, Vertruyen M, et al. (1997) Conversions and complications in 185 laparoscopic adjustable silicone gastric banding cases. Surg Endosc 11: 268-71.
- Ponce J, Haynes B, Paynter S, Fromm R, Lindsey B, et al. (2004) Effect of Lap-Band®-induced weight loss on type 2 diabetes mellitus and hypertension. Obes Surg 14: 1335-42.
- Li VKM, Pulido N, Fajnwaks P, Szomstein S, Rosenthal R, et al. (2009) Predictors of gallstone formation after bariatric surgery: A multivariate analysis of risk factors comparing gastric bypass, gastric banding, and sleeve gastrectomy. Surg Endosc 23: 1645.
- Frezza EE (2007) Laparoscopic vertical sleeve gastrectomy for morbid obesity. The future procedure of choice? Surg Today 37: 275-81.
- Ahroni JH, Montgomery KF, Watkins BM (2005) Laparoscopic adjustable gastric banding: Weight loss, co-morbidities, medication usage and quality of life at one year. Obes Surg 15: 641-7.
- Steffen R, Biertho L, Ricklin T, Piec G, Horber FF (2003) Laparoscopic Swedish Adjustable Gastric Banding: A five-year prospective study. Obes Surg 13: 404-11.
- Fielding GA, Allen JW (2002) A step-by-step guide to placement of the LAP-BAND adjustable gastric banding system. Am J Surg 184: S26-30.
- Weiss HG, Nehoda H, Labeck B, Peer-Kühberger MDR, Klingler P, et al. (2000) Treatment of morbid obesity with laparoscopic adjustable gastric banding affects esophageal motility. Am J Surg 180: 479-82.
- Van Wageningen B, Berends FJ, Van Ramshorst B, Janssen IFM (2006) Revision of failed laparoscopic adjustable gastric banding to Roux-en-Y gastric bypass. Obes Surg 16: 137-41.
- Ren CJ, Horgan S, Ponce J (2002) US experience with the LAP-BAND system. Am J Surg 184: S46-50.
- Demaria EJ, Winegar DA, Pate VW, Hutcher NE, Ponce J, et al. (2010) Early postoperative outcomes of metabolic surgery to treat diabetes from sites participating in the ASMBS bariatric surgery center of excellence program as reported in the bariatric outcomes longitudinal database. Ann Surg 252: 559-66.
- Ponce J, Paynter S, Fromm R (2005) Laparoscopic adjustable gastric banding: 1,014 Consecutive cases. J Am Coll Surg 201: 529-35.
- Ducarme G, Revaux A, Rodrigues A, Aissaoui F, Pharisien I, et al. (2007) Obstetric outcome following laparoscopic adjustable gastric banding. Int J Gynecol Obstet 98: 244-7.
- Forsell P, Hellers G (1997) The Swedish adjustable gastric banding (SAGB) for morbid obesity: 9 year experience and a 4-year follow-up of patients operated with a new adjustable band. Obes Surg 7: 345-51.
- Nguyen NT, Varela JE (2017) Bariatric surgery for obesity and metabolic disorders: State of the art. Nat Rev Gastroenterol Hepatol 14: 160-9.
- Frigg A, Peterli R, Peters T, Ackermann C, Tondelli P (2004) Reduction in Co-morbidities 4 years after laparoscopic adjustable gastric banding. Obes Surg 14: 216-23.
- Parikh MS, Fielding GA, Ren CJ (2005) U.S. experience with 749 laparoscopic adjustable gastric bands: Intermediate outcomes. Surg Endosc Other Interv Tech 19: 1631-35.
- Cottam DR, Atkinson J, Anderson A, Grace B, Fisher B (2006) A case-controlled matched-pair cohort study of laparoscopic Roux-en-Y gastric bypass and Lap-Band® patients in a single US center with three-year follow-up. Obes Surg 16: 534-40.
- Niville E, Dams A, Vlasselaers J (2001) Lap-Band® erosion: Incidence and treatment. Obes Surg 11: 744-7.
- Vertruyen M (2002) Experience with Lap-Band System® up to 7 years. Obes Surg 12: 569-72.
- Rubenstein RB, Ferraro DR, Raffel J (2002) Laparoscopic adjustable gastric banding at a U.S. center with up to 3-year follow-up. Obes Surg 12: 380-4.
- Nadler EP, Youn HA, Ren CJ, Fielding GA (2008) An update on 73 US obese pediatric patients treated with laparoscopic adjustable gastric banding: comorbidity resolution and compliance data. J Pediatr Surg. 43: 141-6.
- Ren CJ, Fielding GA (2003) Laparoscopic adjustable gastric banding: surgical technique. J Laparoendosc Adv Surg Tech A. 13: 257-63.
- Gumbs AA, Pomp A, Gagner M (2007) Revisional bariatric surgery for inadequate weight loss. Obes Surg 17: 1137-45.
- Skull AJ, Slater GH, Duncombe JE, Fielding GA (2004) Laparoscopic Adjustable Banding in Pregnancy: Safety, Patient Tolerance and Effect on Obesity-Related Pregnancy Outcomes. Obes Surg 14: 230-5.
- Wolfe BM, Kvach E, Eckel RH (2016) Treatment of Obesity: Weight Loss and Bariatric Surgery. Circ Res 118: 1844-55.
- Byrne J., Rogers C, Welbourn R, Jennings N. BJ (2015) The By-Band-Sleeve Study: A Pragmatic Multicentre Randomised (Conntrolled) Trial to Examine The Effectiveness and Cost Effectiveness of Adjustable Gastric Band, Roux-En-Y Gastric Bypass And Sleeve Gastrectomy for Severe and Complex Obesity. Surg Obes Relat Dis 11.
- Powell AGMT, Bevan V, Brown C, Lewis WG (2018) Altmetric Versus Bibliometric Perspective Regarding Publication Impact and Force. World J Surg 42: 2745-56.
- Chang J, Desai N, Gosain A (2019) Correlation Between Altmetric Score and Citations in Pediatric Surgery Core Journals. J Surg Res 243: 52-8.
- He L, Fang H, Wang X, Wang Y, Ge H, et al.( 2020) The 100 most-cited articles in urological surgery: A bibliometric analysis. Int J Surg 75: 74-9.
Citation: Thompson D, Baruah B, Barry J (2021) The 100 Most Influential Manuscripts in Laparoscopic Adjustable Gastric Banding: A Bibliometric andAltmetric Analysis. J Obes Weight Loss Ther 11: 468 DOI: 10.4172/2165-7904.1000468
Copyright: © 2021 Thompson D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided theoriginal author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1562
- [From(publication date): 0-2021 - Apr 26, 2025]
- Breakdown by view type
- HTML page views: 1018
- PDF downloads: 544