Research Article Open Access
Ten-Year Coronary Artery Disease Risk in 1571 Newly Presenting Hypertensive Black Subjects
Ojji D1*, Stewart S2, Atherton J3, Ajayi S4, Mamven M5, Ngabea M1, Ojji O6 and Karen S7
1Cardiology Unit, Department of Medicine, University of Abuja Teaching Hospital, Gwagwalada , Abuja
2NHMRC Centre of Research Excellence to Reduce Inequality in Heart Disease, Australian Catholic University, Melbourne, Australia
3Department of Cardiology, Royal Brisbane and Women Hospital and University of Queensland School of Medicine, Brisbane, Australia
4Nephrology Unit, Department of Medicine, University College Hospital, Ibadan, Nigeria
5Nephrology Unit, Department of Medicine, University of Abuja Teaching Hospital, Gwagwalada, Nigeria
6Nephrology Unit, Department of Medicine, University of Abuja Teaching Hospital, Gwagwalada, Nigeria
7Hatter Institute of Cardiovascular Research in Africa, Faculty of Medicine, University of Cape Town, South Africa
- *Corresponding Author:
- Dike Ojji
Cardiology Unit, Department of Medicine
University of Abuja Teaching Hospital
Gwagwalada, Abuja, Nigeria
Tel: +234-8060094456
E-mail: dikeojjki@yahoo.co.uk
Received date: May 20, 2016; Accepted date: June 13, 2016; Published date: June 24, 2016
Citation: Ojji D, Stewart S, Atherton J, Ajayi S, Mamven M, et al. (2016) Ten-Year Coronary Artery Disease Risk in 1571 Newly Presenting Hypertensive Black Subjects. J Community Med Health Educ 6:442. doi:10.4172/2161-0711.1000442
Copyright: © 2016 Ojji D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Although hypertension is highly prevalent in Nigeria, coronary artery disease (CAD) remains relatively uncommon. This may well change due to epidemiological transition. To ascertain the future role of CAD in Nigeria, we risk stratified every consecutive hypertensive subject referred to the Cardiology unit of the University of Abuja Teaching Hospital over 7 years.
Hypothesis: A significant proportion of the study population will fall within the intermediate or high risk category.
Methods: It is a prospective, observational study. 1571 hypertensive subjects were risk stratified according to the Framingham 10-year Risk Score.
Results: 834(53.1%) of the subjects were female while 737(46.9%) were male. The mean age, mean body mass index and mean arterial pressure of the subjects were 50.9 ± 11.4 years, 28.1 ± 9.4 kg/m2 and 116.23 ± 13.1 mmHg respectively. According to Framingham criteria, 1263(80.4%) of the study population were low risk individuals, 286(18.2%) were medium risk, 22(1.4%) were high risk individuals. When the age of the subjects was hypothetically increased by an additional 10 years, the high risk group increased from 1.3% to 21.3%.
Conclusions: According to the Framingham risk score, the majority of subjects with hypertension presenting to a large teaching hospital in Nigeria have a low risk of developing CAD in the near future, which contrasts with the risk profile seen in hypertensive subjects in Europe and North America. Nonetheless, approximately one in four subjects were classified as intermediate or high risk emphasizing the importance of lifestyle modification and the need to consider absolute risk stratification to guide management in countries undergoing epidemiological transition.
Keywords
Coronary artery; Disease; Risk; Hypertensive subjects
Introduction
Despite a relatively high prevalence of hypertension in Nigeria (estimated to affect 25-27% of the population) [1], and the high burden of hypertensive left ventricular hypertrophy [2-6], hypertensive heart failure [7-10], chronic kidney disease [11-16] and strokes [17,18] due to uncontrolled hypertension, the prevalence of coronary artery disease (CAD) is still relatively low [19,20].
This represents a paradox given that each 20 mmHg increase in SBP over the range of 115-185 mmHg doubles coronary heart disease and stroke mortality [21]. Consequently, in clinical trials, anti-hypertensive therapy is associated with a 20-25% reduction in incident myocardial infarction [22]. Furthermore, a 10 to 12 mmHg reduction in systolic blood pressure and a 5 to 6 mmHg reduction in diastolic blood pressure has been shown to reduce the risk of coronary artery disease (CAD) by 16% [21]. It has however, been projected that with the epidemiological transition in disease pattern being experienced in many parts of sub-Saharan Africa [23], CAD is likely to play a more significant role in the burden of disease in Nigeria in the future.
To ascertain the future role of CAD in Nigeria, we risk stratified consecutive hypertensive subjects undergoing specialist cardiology review in a major tertiary referral hospital in Nigeria, according to 10 year Framingham risk criteria.
Methods
Subjects
We prospectively studied every consecutive patient referred for the first time to the Cardiology Clinic of the University of Abuja Teaching Hospital with a diagnosis of hypertension from April 2006 to August 2013. These patients were typically referred by General and Family Physicians in Primary and Secondary Healthcare facilities including both the public and private sector. The patients included public servants, traders, businessmen, politicians, farmers, artisans and retired public servants. A total of 2275 subjects were recruited for the study with an average recruitment of 28 per month. Subjects with established cardiovascular disease including prior documented stroke, coronary artery disease, heart failure and chronic kidney disease which represented 30% of the total subjects recruited were excluded from the study. This left 1571 hypertensive subjects with no documented vascular disease or chronic kidney disease at baseline, of whom 110(7%) were diabetic.
Study data
Using a standardized questionnaire, baseline demographic and clinical characteristics of patients were obtained. In order to minimize selection bias, data were collected on a consecutive patient basis. Information obtained from the patients included gender, age, prior history of hypertension or diabetes mellitus and family history of hypertension or diabetes mellitus. Other information collected was past or present history of myocardial infarction, angina pectoris, stroke, heart failure and renal failure. Pharmacological treatment was determined by the treating clinician.
Each subject had a complete physical examination including height and weight measurements. Blood pressure measurement was according to standard guidelines with a mercury sphygmomanometer (Accosson, London, UK). Systolic and diastolic blood pressures was measured using Korotkof sounds I and V. Blood pressure was measured at the right arm three times, with a 5 minute rest between each measurement. The diagnosis of hypertension was made when the average of three blood pressure measurements was ≥ 140/90 mmHg or the subject had been previously diagnosed with hypertension and was on antihypertensive therapy. Subjects were asked to fast for 8-12 hours before blood sample collection. Blood chemical analysis was performed at a certified central laboratory. Fasting blood glucose and lipids were analysed enzymatically by auto analyzer (Erber Spectrophotometer). This study complied with the Declaration of Helsinki and all participants provided written informed consent and the study was approved by the University of Abuja Teaching Hospital Ethics Committee.
Framingham risk
The specific 10-year risk of CAD was calculated (as a specific percentage score) in all the subjects according to the Framingham Risk Stratification algorithm including age, gender, total and high-density lipoprotein-cholesterol, systolic blood pressure, and cigarette smoking. Subjects were then classified as <10% (low risk), 10-20% (intermediate risk) and >20% (high risk). The Framingham risk score has been found to perform well in African Americans which is a population that has the same ancestry origin as our subjects [24].
Data analysis
SPSS software version 16.0 (SPSS Inc, Chicago, IL) was used for statistical analysis. Continuous variables were expressed as mean ±SD. We compared the distribution of the three risk groups and related the distribution to the sex of the subjects and the presence or absence of diabetes mellitus. We also compared the demographic and clinical characteristics of the subjects using student t-test. A 2-tailed p value<0.05 was considered significant.
Results
Demographic and clinical characteristics of the subjects
Table 1 shows the demographic and clinical characteristics of the subjects and also by gender. This was a predominantly middle-aged cohort (mean age 50.1 ± 12.6 years), 53% women and predominantly overweight (mean BMI 28.9 ± 6.7 kg/m2).
| Variables | ALL (N=1571) | Males (N=737) |
Females (N=834) |
P-value |
|---|---|---|---|---|
| Age (Years) | 50.1 ± 12.6 | 50.8 ± 12.1 | 49.5 ± 12.9 | 0.03 |
| Smoking Habits | 13.3 | 0.9 | <0.0001 | |
| Systolic Blood Pressure (mmHg) | 153.4 ± 25.1 | 156.1 ± 25.3 | 152.7 ± 25.0 | 0.28 |
| Diastolic Blood Pressure (mmHg) | 95.2 ± 15.7 | 95.9 ± 16.1 | 94.3 ± 15.3 | 0.09 |
| Mean Arterial Pressure(mmHg) | 107.1 ± 18.6 | 110.4 ± 19.1 | 109.9 ± 19.9 | 0.63 |
| Body Mass Index (mmHg) | 28.9 ± 6.7 | 27.3±5.8 | 30.4±7.0 | <0.0001 |
| Total Cholesterol (mmol/L) | 5.0 ± 1.2 | 4.9 ± 1.2 | 5.3 ± 1.3 | <0.0001 |
| LDL Cholesterol (mmol/L) | 3.2 ±1.2 | 3.2 ± 1.1 | 3.3 ± 1.3 | 0.59 |
| HDL Cholesterol (mmol/L) | 1.2 ± 0.51 | 1.0 ± 0.49 | 1.3 ± 0.56 | 0.44 |
| Triglyceride (mmol/L) | 1.3 ± 0.69 | 1.0 ± 0.30 | 2.1 ± 0.77 | <0.0001 |
| Urea(mmol/L) | 5.5 ± 2.7 | 5.2 ± 1.4 | 5.9 ± 1.5 | 0.05 |
| Creatinine (µmol/L) | 103.0 ± 20.8 | 99.8 ± 47.8 | 109.0 ± 47.2 | 0.12 |
| Packed Cell Volume (%) | 39.7 ± 5.4 | 41.3 ± 6.2 | 38.0 ± 5.2 | <0.0001 |
| White Blood Count | 5.9 ± 2.3 | 5.9 ± 2.7 | 5.9 ± 1.7 | 0.69 |
Table 1: Demographic and clinical characteristics of all the subjects by gender.
Females were slightly younger than their male counterparts (49.5 ± 12.9 years versus 50.8 ± 12.1 years, p=0.03). They also smoked less than their male counterparts (0.9% versus 13.3% p<0.0001). Female subjects had higher body mass index, total cholesterol and triglyceride levels (30.4 ± 7.0 kg/m2 versus 27.3 ± 5.8 kg/m2, p<0.0001, 5.3 ± 1.3 mmol/L versus 4.9 ± 1.2 mmol/L, p<0.0001 and 2.1 ± 0.77 mmol/L versus 1.0 ± 0.30 mmol/L, p<0.0001). Blood pressures were similar in men and women.
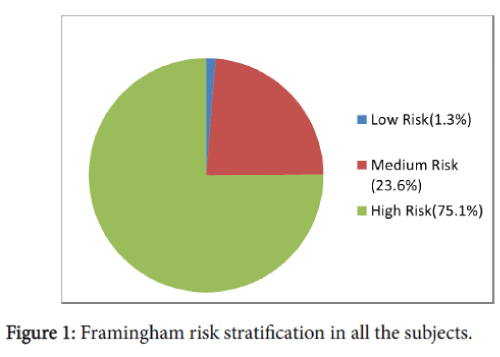
Distribution of risk stratification in all the subjects
Figure 1 shows the distribution of risk stratification in the 1591 subjects. 1263(80.4%) were classified low risk, 286(18.2%) moderate risk and 22(1.4%) high risk of CAD events within 10 years.
Distribution of risk stratification in all the subjects
Figure 1 shows the distribution of risk stratification in the 1591 subjects. 1263(80.4%) were classified low risk, 286(18.2%) moderate risk and 22(1.4%) high risk of CAD events within 10 years.
Table 2 shows the increasing trend in the proportion of subjects classified in the highest risk category when the average age of the cohort is hypothetically increased by 5 years at a time to a maximum of 10 years. The high risk category increased from 1.3% to 21.3% when 10 years was added to the original age of subjects.
| FRS | Normal Age N=1571 |
Age+5years N=1571 |
Age+10years N=1571 |
|---|---|---|---|
| Low | 1,263(80.4%)**,*** | 1,178(75.0)*** | 819(52.1%) |
| Moderate | 286(18.2%) | 240(15.3%) | 417(26.6%)*, ** |
| High | 22(1.4%) | 153(9.7%) | 334(21.3%)*, ** |
*= significantly higher than those with Normal Age, **= significantly higher than those with Age+5year,***= significantly higher than those with Age+10years, P-value less than 0.05 is significant.
Table 2: Comparison of framingham risk score in the cohort with progressive ages.
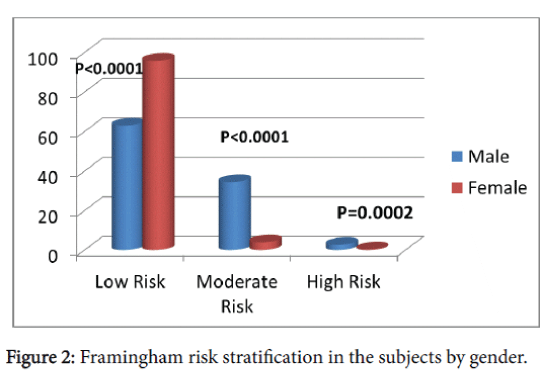
Distribution of risk stratification in the subjects by gender
Figure 2 shows the distribution of risk stratification in the subjects by gender. The male subjects had a higher proportion classified as moderate and high risk compared to the female subjects (34.4% versus 5.9%, p<0.0001 and 2.6% versus 0.3%, p=0.0002 respectively), and had a lower proportion of those classified as low risk (63.0% versus 94.8%, p < 0.0001).
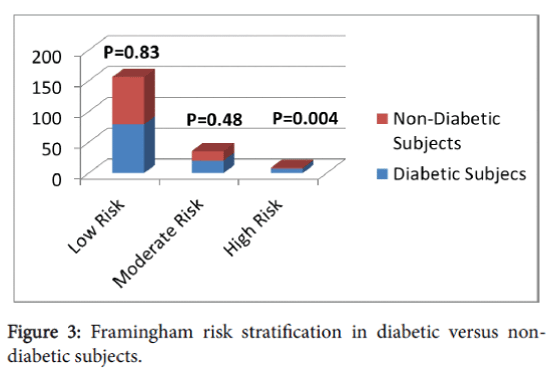
Framingham risk classification in diabetic and non-diabetic subjects
Figure 3 shows that the proportion of the diabetic subjects classified as high risk was significantly higher than that of the non-diabetic subjects (7.7% versus 1.3%, p=0.004), while there was no significant difference in proportions classified in the low and moderate risk categories.
Discussion
Consistent with a relatively low prevalence of CAD in Nigeria, amongst a large cohort of individuals with newly diagnosed hypertension, we found that only 1.3% of our subjects were classified as being at high risk of developing CAD in the next ten years according to Framingham criteria. The remainders were either at intermediate (approximately one quarter) or low risk (approximately three quarters of the cohort) for such an outcome.
These data contrast with that reported by Wong and colleagues [25] who reported that 55% of hypertensive subjects were classified as high risk using the Framingham Risk Score in American subjects, and an Italian study where approximately 60% were classified as high risk based on European guidelines [26]. It is also much lower than the findings of Fagard et al. [27] who showed that 39.6% of subjects with isolated systolic hypertension were classified as high risk as compared to 68.4% of subjects with diastolic hypertension. The much lower risk of developing CAD in our subjects compared to Caucasians and Asians is not surprising as our subjects have been shown previously to have a lower prevalence of cardio metabolic risk factors [28], compared to Caucasians [29] and Asians [30]. A diet that is lower in saturated fat and rich in vegetables might also be contributory to the lower risk in our subjects [23]. Furthermore, our subjects were younger than other hypertensive cohorts, however this is unlikely to completely explain the much lower risk of CAD observed in our cohort. Indeed, when the age of our cohort was hypothetically increased by an additional 10 years (similar to the average age reported by Mancia et al. in an Italian hypertensive cohort in which 55% were classified as high risk), only 21% of subjects were classified as high risk. Whilst this admittedly assumes that other risk factors remain the same, given that age is the major driver of absolute risk, it implies that our cohort has a substantially lower risk driven by the low prevalence of other cardiovascular risk factors.
Our female subjects were at lower risk of developing coronary artery disease compared to male subjects similar to previous report [31]. This is most likely due to the younger age and higher smoking rates in men. The female subjects were however found to have higher total cholesterol and triglyceride levels, similar to previous report in African Americans [32]. We found our diabetic subjects to be at a higher risk of developing coronary artery disease when compared to non-diabetic subjects. This finding is not surprising as diabetes mellitus is a strong risk factor for ischemic heart disease [32-34].
With recent westernization and improvements in the control of infectious diseases in most parts of Sub-saharan Africa, life expectancy in Nigeria is most likely going to increase. Such an increase in the aging population fuelled by changing diet from westernization means that a higher proportion of our hypertensive subjects will develop CAD in the near future. This will mean triple burden of cardiovascular disease from not only hypertensive heart failure and stroke but also from coronary artery disease.
Therefore, apart from increasing public health education on life style modification to stem the trend of changing lifestyle and diet, there might be the need for additional catheterization laboratories (presently there are only two publicly run catheterization laboratories in Nigeria). This will obviously involve planning and appropriation of resources especially in the face of increasing burden of hypertensive heart failure and stroke in this population group [35].
Limitations of the Study
Since Framingham Risk Score was used to risk stratify our subjects, BMI was not taken into account. In addition, risk factors such as family history of premature cardiovascular disease, obesity, high sensitivity Creactive protein, homocysteine, cytokines, hypertriglyceridemia, impaired glucose tolerance and obesity were not taken into account. There would have also been under estimation of risk score in subjects with severe hypertension (systolic blood pressure >180 mmHg and/or DBP>110 mmHg) or associated target organ damage. However, the fact that Framingham risk score is the only risk score that has been validated in African Americans who have the same ancestry origin as our subjects makes it the most suitable risk scoring system for our subjects.
Conclusion
Whilst the risk of developing coronary artery disease in hypertensive subjects presenting to a major teaching hospital in Nigeria appears to be substantially lower compared to European and North American cohorts, one in four subjects were nonetheless classified as intermediate or high risk. This emphasizes the need to address emerging risk factors including smoking and obesity, and the need to consider absolute risk to guide treatment decisions in countries undergoing epidemiological transition.
Acknowledgement
Our sincere appreciation goes to all members of staff of Cardiology Unit, Department of Medicine, University of Abuja Teaching Hospital, Gwagwalada, Abuja.
References
- Ogah OS (2006) Hypertension in sub-Saharan African Population: the burden of hypertension in Nigeria. Ethn Dis 16: 765.
- Aje A, Adebiyi AA, Oladapo OO, Dada A, Ogah OS, et al. (2006) Left ventricular geometric patterns in newly presenting Nigerian hypertensives: An echocardiographic study. BMC CardiovascDisord 6: 4.
- Salako BL, Ogah OS, Adebiyi AA, Oladapo OO, Aje A, et al. (2009) Blood pressure control and left ventricular hypertrophy in hypertensive Nigerians. Ann Afr Med 8: 156-162.
- Dada A, Adebiyi AA, Aje A, Oladapo OO, Falase AO, et al. (2005) Standard electrocardiographic criteria for left ventricular hypertrophy in Nigerian hypertensives. Ethn Dis 15: 578-584.
- Kolo PM, Omotosho ABO, Katibi IA, Sanya EO, Adamu UG, et al. (2008) Gender Differences in left ventricular size and Geometric Pattern of Hypertension Subjects. The Cardiol 4: 11-15.
- Adebayo RA, Bamikole OJ, Balogun MO, Akintomide AO, Adeyeye VO, et al. (2013) Echocardiographic Assessment of Left Ventricular Geometric Patterns in Hypertensive Patients in Nigeria. Clin Med Insights Cardiol 7:161-167.
- Ojji DB, Alfa J, Ajayi SO, Mamven MH, Falase AO, et al. (2009) Pattern of heart failure in Abuja, Nigeria: an echocardiographic study. Cardiovasc J Afr 20: 349-352.
- Onwuchekwa AC, ASekomah GE (2009) Pattern of heart failure in a Nigerian teaching hospital. Vasc Health Risk Manag 5: 745-750.
- Laabes EP, Thacher TD, Okeahialam BN (2008) Risk factors for heart failure in adult Nigerians. ActaCardiol 63: 437-443.
- Ogah OS, Falase AO, Carrington M, Sliwa K (2012) Hypertensive heart failure in Nigerian Africans: Insights from the Abeokuta heart failure registry. J Clinic Hypertension 17: e703
- Ojogwu LI (1990) The pathological basis of end stage renal disease in Nigerians: experience from Benin City. West Afri J Med 9: 193-196.
- Ulasi II, Ijoma CK (2010) The enormity of chronic kidney disease in Nigeria: the situation in a teaching hospital in South-East Nigeria. J Trop Med pp: 1-6.
- Ojo OS, Akinsola AA, Nwosu SO, Odesanmi WO (1992) The pathological basis of chronic renal failure in Nigerians. An autopsy study. Trop Geogr Med 44: 42-46.
- Akinsola W, Odesanmi WO, Ogunniyi JO, Ladipo GO (1989) Diseases causing chronic renal failure in Nigerians- a prospective study of 100 cases. Afr J Med Sci 18: 131-137.
- Arogundade FA, Sanusi AA, Hassan MO, Akinsola A (2011) The pattern, clinical characteristics and outcomes of ESRD in Ile-Ife, Nigeria: is there a change in trend? Afr Health Sci 11: 594-601.
- Alebiosu CO, Ayodele OO, Abbas A, Olutoyin AI (2006) Chronic renal failure at OlabisiOnabanjo University Teaching Hospital, Sagamu, Nigeria. Afr Health Sci 6: 132-138.
- Ogun SA, Ojini FI, Ogungbo B, Kolapo KO, Danesi MA (2005) Stroke in South West Nigeria: a 10-year review. Stroke 36: 1120-1122.
- Wahab KW (2008) The burden of stroke in Nigeria. Int J Stroke 3: 290-292.
- Sani MU, Adamu B, Mijinyawa MS, Abdu A, Karaye KM, et al. (2006) Ischemic heart disease in Aminu Kano Teaching Hospital, Kano, Nigeria: a 5 year review. Niger J Med 15: 128-131.
- Anjorin CO, Buba F, Ene AC (2005) Myocardial Infarction at the University of Maiduguri Teaching Hospital, North Eastern Nigeria: A Long-term Review. J Med Sci5: 358-362.
- Lewington S, Clance R, Quizibash N, Peto R, Collins R; et al. (2002) Age-Specific relevance of usual blood pressure to vascular mortality: a meta-analysis individual data for one million adults in 61 prospective studies. Lancet 360: 1903-1913.
- Neal B, Mac Mahon S, Chapman N (2000) Effects of ACE inhibitors. Calcium antagonists and other blood pressure lowering drugs: results of prospectively designed overviews of randomised trials. Lancet 356: 1955-1964.
- Akinboboye O, Idris O, Akinboboye O, Akinkugbe O (2003) Trends in Coronary artery disease and associated risk factors in sub-Saharan Africans. J Hum Hypertens 17: 381-387.
- Hurley LP, Dickinson LM, Estacio RO, Steiner JF, Havranek EP (2010) Prediction of Cardiovascular Death in Racial/Ethnic Minorities using Framingham Risk Factors. CircCardiovadcQual Outcomes 3: 181-187.
- Wong ND, Dede J, Chow VH, Wong KS, Franklin SS, et al. (2012) Global Cardiovascular Risk Associated with Hypertension and Extent of Treatment and Control According to Risk Group. Am J Hypertens 25: 561-567.
- Mancia G, Volpe R, Boros S, Ilardi M, Giannattasio C (2004) Cardiovascular risk profile and blood pressure control in Italian hypertensive patients under specialist care. J Hypertens 22: 51-57.
- Fagard RH, Van Den Enden M, Leeman M, Warling X (2002) Survey on treatment of hypertension and implementation of World Health Organization/International Society of Hypertension risk stratification in primary care in Belgium. J Hypertens 20: 1297-1302.
- Ojji DB, Ajayi SO, Mamven MH, Alabi P (2012) Prevalence of Metabolic Syndrome among Hypertensive Patients in Abuja, Nigeria. Ethn Dis 22: 1-4.
- Jurgen S, Eduardo A, Claudio F, Langham S, Stevens W, et al. (2010) Epidemiological and economic burden of metabolic syndrome and its consequences in patients with hypertension in Germany, Spain and Italy; a prevalence-based model. BMC Public Health 10: 529.
- Chih-Neng H, Iya-Chen C, Tzung-Dau W (2005) Prevalence and Characteristic of Metabolic Syndrome in Chinese Hypertensive Patients: A Hospital-Based Observation. ActaCardiol Sin 21: 89-97.
- Lloyd-jones DM, Larson MG, Beiser A, Levy D (1999) Lifetime risk of developing coronary heart disease. Lancet 353: 89-92.
- O’Meara JG, Kardia SLR, Armon JJ, Brown CA, Boerwinkle E, et al. (2004) Ethnic and Sex Differences in the Prevalence, Treatment and Control of Dyslipidaemia among Hypertensive Adults in the GENOA Study. Arch Intern Med 164: 1313-1318.
- Scnnohr P, Jensen JS, Scharling H, Nordestgaard BG (2002) Coronary heart disease risk factors ranked by importance for the individual and community. A 21-year follow-up of 12000 men and women from Copengham city Heart Study. European Heart J 23: 620-626.
- Howard BV, Best LG, Galloway JM, Howard WJ, Jones K, et al. (2006) Coronary Heart Disease Risk Equivalence in Diabetes Depends on Concomitant Risk Factors. Diabetes Care 29: 391-397.
- Maiyaki MB, Garbati MA (2014) The burden of non-communicable diseases in Nigeria; in the context of globalization. Ann Afr Med 13: 1-10.
--
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 11775
- [From(publication date):
June-2016 - Apr 01, 2025] - Breakdown by view type
- HTML page views : 10859
- PDF downloads : 916