Research Article Open Access
Temperature Control of Infants with/without Asphyxia during Transport
Uemura H1, Ioroi T1, Nabetani M2*, Egawa T1, Kugo M1, Sano H2, Takahashi A3, Watabe S3 and Tamura M4
1Department of Pediatrics, Perinatal Medical Center, Japanese Red Cross Society Himeji Hospital, Japan
2Department of Pediatrics, Yodogawa Christian Hospital, Japan
3Department of Neonatal Intensive Care, Kurashiki Central Hospital, Japan
4Department of Neonatology, Saitama Medical Center, Japan
- *Corresponding Author:
- Nabetani M
Department of Pediatrics
Yodogawa Christian Hospital, Japan
Tel: 81-66322-2250
E-mail: a103111@ych.or.jp
Received: December 09, 2015; Accepted: December 16, 2015; Published: December 24, 2015
Citation: Uemura H, Ioroi T, Nabetani M, Egawa T, Kugo M, et al. (2015) Temperature Control of Infants with/without Asphyxia during Transport. Neonat Pediatr Med 1: 103. doi: 10.4172/2572-4983.1000103
Copyright: © 2015 Uemura H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
Background: Therapeutic hypothermia (TH) has been shown to improve the outcome following perinatal asphyxia. To obtain the maximum benefit, therapeutic hypothermia should be initiated as soon as possible within 6 hr after birth. In Japan, it is important to develop effective and safe protocols to control the temperature during transport.
Objective: To evaluate the efficacy and safety of continuous monitoring of rectal temperatures during transport of infants with/without asphyxia in order to control body temperature properly and to induce passive cooling for infants with mild to severe Hypoxic-ischemic-encephalopathy (HIE) safely.
Methods: Skin and rectal temperatures during transport were prospectively collected from transported newborns between August 2012 and August 2014 at three regional cooling centers. In the case of infants without asphyxia, the transport team controlled the temperature of the transport incubator 33 ± 2°C to maintain a target rectal temperature at as close to 36.0-36.5°C as possible. While in the case of infants with asphyxia, the transport team controlled the temperature of the transport incubator between 31 and 32°C to maintain a target rectal temperature at as close to 35.0°C as possible. The rectal and skin temperatures were monitored continuously and recorded by the bedside monitor for later analysis.
Results: In the 2 year study period, the skin and rectal temperatures of 52 newborns without asphyxia were monitored continuously. The median gestational age and birth weight of them were 38.1 (36.0-41.3) weeks and 2905 (1904-4408) g. The rectal temperature is correlated significantly with skin temperature (p<0.001). In two cases, only rectal temperatures but skin temperatures showed decrease (≥ 0.4°C) in winter season. Twelve infants with asphyxia were passively cooled during transport. Ten of 12 cases were analyzed. The median gestational age and birth weight of them were 39.6 (34.0-41.0) weeks and 2584 (2032-2838) g, six cases of 10 showed moderate or severe HIE and four cases of 10 showed mild HIE. Five cases of moderate to severe HIE underwent therapeutic hypothermia within 6 hours of birth, but one case with severe HIE did not undergo TH because of prematurity. The median rectal temperature at arrival was 35.3 (32.9-36.4°C (NS). Four of 6 moderate or severe HIE infants had a rectal temperature at arrival between 34.5-35.5°C, and one >35.5°C. One of 4 mild HIE infants had a rectal temperature at arrival between 34.5-35.5°C and three >35.5°C. Only one preterm infant with severe HIE was overcooled.
Conclusion: Passive cooling by controlling the transport incubator temperature for infants with HIE was relatively safe and could prevent to be elevated body temperature. However, there may be a risk of unintended excessive cooling, especially in severe HIE infants and preterm infants during longer transfer. We suggest that continuous monitoring of the rectal temperature to control body temperature during transport especially for passive cooling is mandatory. We need further studies to clarify protocols to control body temperature of infants during transport including passive cooling.
Keywords
Therapeutic hypothermia; Hypoxic-ischemicencephalopathy; Neonatal transport; Passive cooling; Rectal temperature
Introduction
Therapeutic hypothermia (TH) has been shown to improve survival and neurodevelopmental outcome following perinatal asphyxia [1- 6]. To obtain the maximum benefit, TH should be initiated as soon as possible and within 6 hr after birth. Particularly, outborn infants might not be able to transport to cooling center and initiate therapeutic hypothermia within 6 hr. Furthermore, it is thought that elevated core temperature after asphyxial insults is associated with worse outcomes among HIE infants [7]. Therefore it is truly essential to develop effective and safe methods of cooling during transport, because about half of babies were born in private clinics in Japan. Passive cooling could be a simple technique to prevent brain damage from HIE during transport [8-11]. However, we have not got useful device to monitor core temperature during transport. Therefore we have evaluated how to control core and skin temperature of infants with/without asphyxia during transport from clinics to hospitals in Japan in this study.
Objective
The aim of our study was to evaluate the efficacy and safety of continuous monitoring of rectal temperatures during transport of infants with/without asphyxia in order to control body temperature properly and to induce passive cooling for infants with mild to severe HIE safely. We hypothesized that passive cooling during transport could prevent to be elevated body temperature, and it could get infants to targeted temperatures without delay after starting TH.
Methods
• Skin and rectal temperatures of infants during transport were prospectively collected between August 2012 and August 2014 at three regional cooling centers, Himeji red-cross hospital, Kurashiki- Central Hospital and Yodogawa Christian Hospital.
• The patient’s rectal and skin temperatures were monitored continuously and recorded by the bedside monitor in ambulance for later analysis using BSM-3562, a flexible multi-parameter bedside monitor (Nihon Kohden CO., Ltd, Tokyo, Japan).
• In the case of infants without asphyxia, the transport team controlled the temperature of the transport incubator 33 ± 2°C to maintain a target rectal temperature at as close to 36.0-37.0°C as possible.
Enrollment criteria
Gestational weeks: >33 weeks
Birth weight: >1800 g
Apgar score (5 min): >7
• Background of 52 cases without asphyxia
Transient tachypnea of neonates 28, meconium aspiration syndrome 4, chromosomal anomaly 3, congenital heart disease 2, congenital anomaly 2, pulmonary hemorrhage 2 and so on.
• In the case of infants with asphyxia, the transport team controlled the temperature of the transport incubator between 31°C and 32°C to maintain a target rectal temperature at as close to 35.0°C as possible. The rectal and skin temperatures were monitored continuously and recorded by the bedside monitor for later analysis.
Passive cooling: Enrollment criteria
Gestational weeks: >33 weeks
Birth weight: >1800 g
Apgar score (5 min): <8
• After arrival at cooling center, moderate or severe HIE infants who were qualified inclusion criteria of therapeutic hypothermia were initiated servo-controlled hypothermia therapy, and the others were rewarmed carefully.
• The institutional review board approved the study protocol and informed consent was obtained from the parent.
• We did statistical analysis by JMP 11 (SAS Institute Inc., Cary, NC, USA).
Results
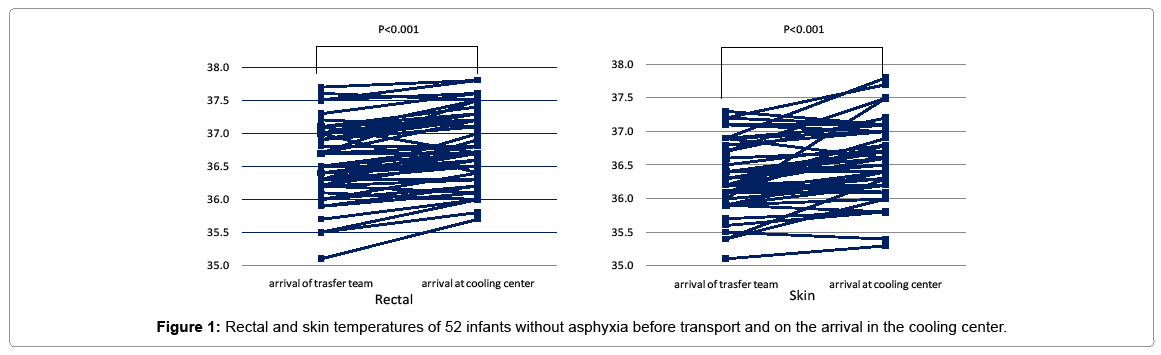
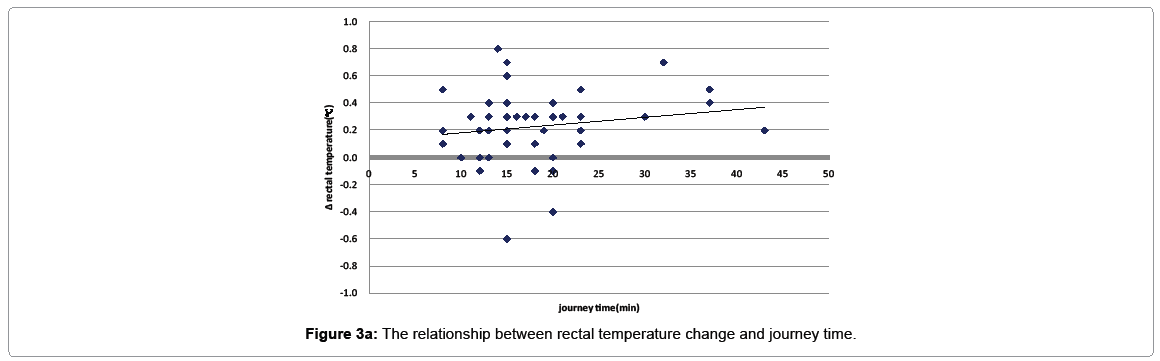
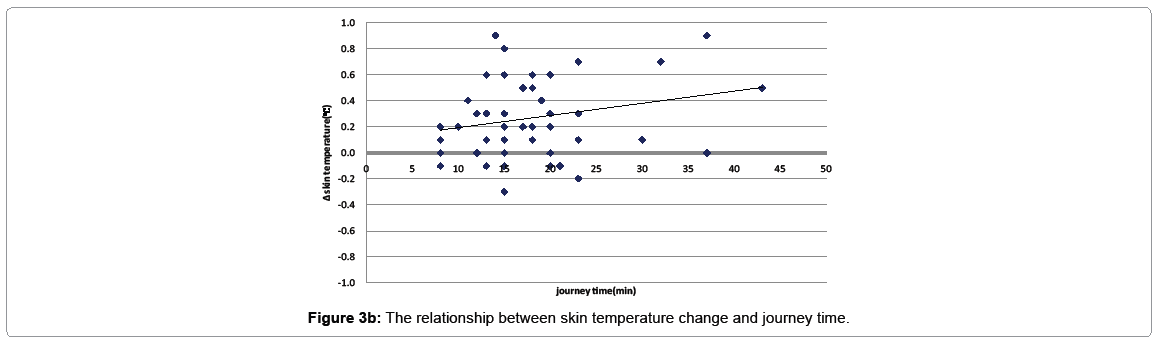
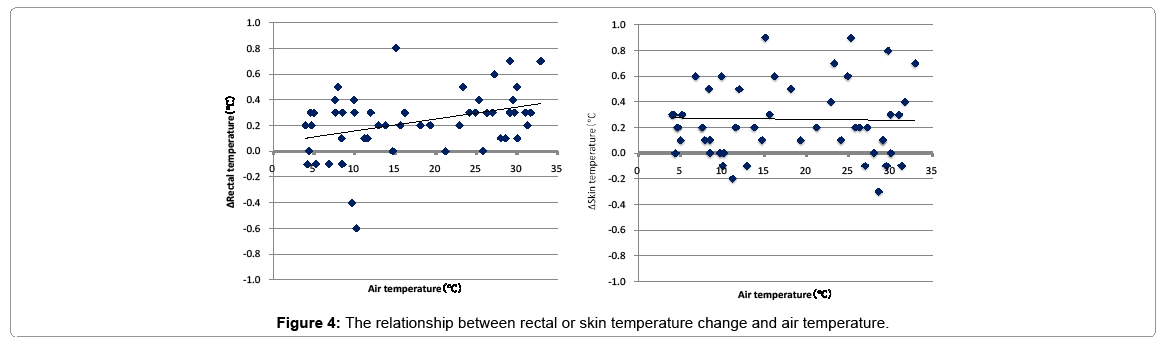
The skin and rectal temperatures excluded due to removal of the rectal and skin monitor, and 52 newborns were analyzed. The median gestational age and birth weight of them were 38.1 (36.0-41.3) weeks and 2905 (1904-4408) g. The median rectal temperature at departure from referring hospital was 36.5°C (range 35.1-37.7°C) and the median rectal temperature at arrival of cooling center was 36.8°C (range 35.7-37.8°C) (P<0.001 Wilcoxon signed-rank test). The median skin temperature at departure from referring hospital was 36.2°C (range 35.1-37.3°C) and the median skin temperature at arrival of cooling center was 36.5°C (5.3°C to 37.8°C) (P<0.001 Wilcoxon signed-rank test). Forty-two cases out of 52 (81%) showed elevation of rectal temperature and 39 cases out of 52 (75%) showed elevation of skin temperature during transport, and no infants had high temperatures of ≥ 38.0°C. Furthermore, we showed no case with hypothermia (<35.0°C) during transport and all of 5 cases who showed rectal temperature <36.0°C at departure showed elevation of rectal temperature at arrival (Figure 1) and the rectal temperatures are correlated significantly with skin temperatures (P<0.001) (Figure 2). Two cases showed decrease (≥ 0.4°C) of rectal temperature but did not show decrease (≥ 0.4°C) of skin temperature in winter season (Figures 3a,3b and 4).
Twelve infants were passively cooled during transport in the 2-year study period. Two infants of them were not recorded fully their temperatures, therefore ten infants were analyzed. The characteristics of ten infants passively cooled during transport are described in Table 1. Four infants had mild HIE. Six infants had moderate or severe HIE. Five infants of them underwent therapeutic hypothermia after arrival at cooling center. One of them could not undergo TH because of preterm infant (34.0 weeks).
| Gestational age (weeks) | 39.6 (34.0 - 41.0) |
|---|---|
| Birth weight (g) | 2584 (2032 - 2838) |
| Sex (m/f) | 07/03 |
| Apgar score 1 min | 2 (0-6) |
| Apgar score 5 min | 4 (0-7) |
| PH at the admission | 7.27 (6.52-7.35) |
| Base Excess at the admission | -6.2 (-36.5--3.4) |
| Lactate at the admission (mmol/l) | 8.4 (4.9-19) |
| HIE mild/moderate/severe | 4/2/4 |
| Data are presented as median (range:min-max) | |
Table 1: Clinical characteristics of passive cooled infants (n=10).
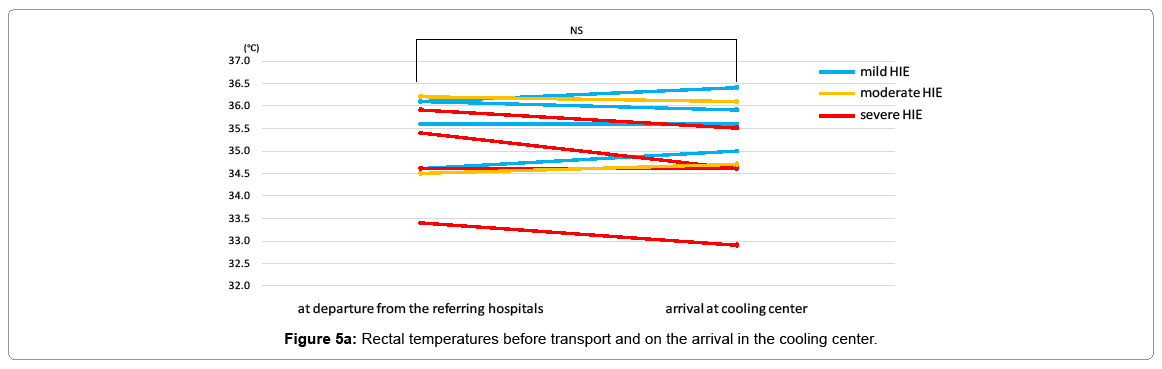
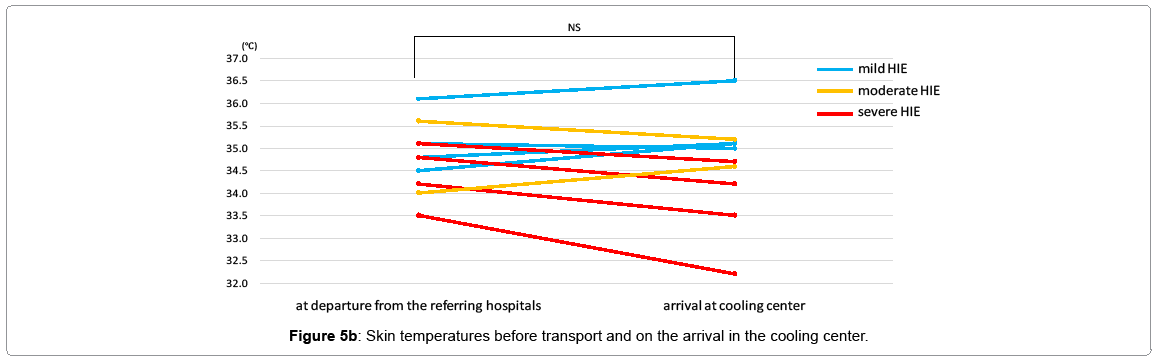
The median rectal temperature at departure from referring hospital was 35.5°C (range 33.4-36.2°C) and the median rectal temperature at arrival of cooling center was 35.3°C (range 32.9-36.4°C) (NS Wilcoxon signed-rank test). The median skin temperature at departure from referring hospital was 34.8°C (range 33.5-36.1°C) and the median skin temperature at arrival of cooling center was 34.9°C (range 32.2-36.5°C) (NS Wilcoxon signed-rank test). No infants had high temperatures of ≥ 37.5°C. The median journey time was 15 min (range 8-50 min). All infants who underwent TH had been achieved a target temperature (34.0°C) within 6h without delay. Median time when infants achieved a target temperature was 281 (271-302) min. after birth.
Five infants (three severe HIE infants, one moderate HIE infant and one mild HIE infant) had achieved successfully target rectal temperature (35.0 ± 0.5°C) at arrival. While, four infants (one moderate HIE and three mild HIE) had a rectal temperature of >35.5°C at arrival. However, one preterm (34.0 weeks) infant was overcooled (rectal temperature at arrival was 32.9°C). This preterm infants showed severe HIE (Figure 5a).
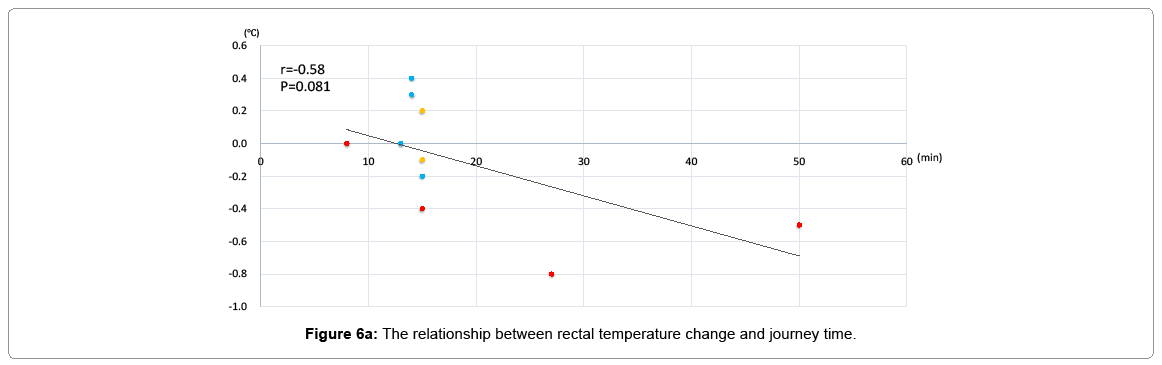
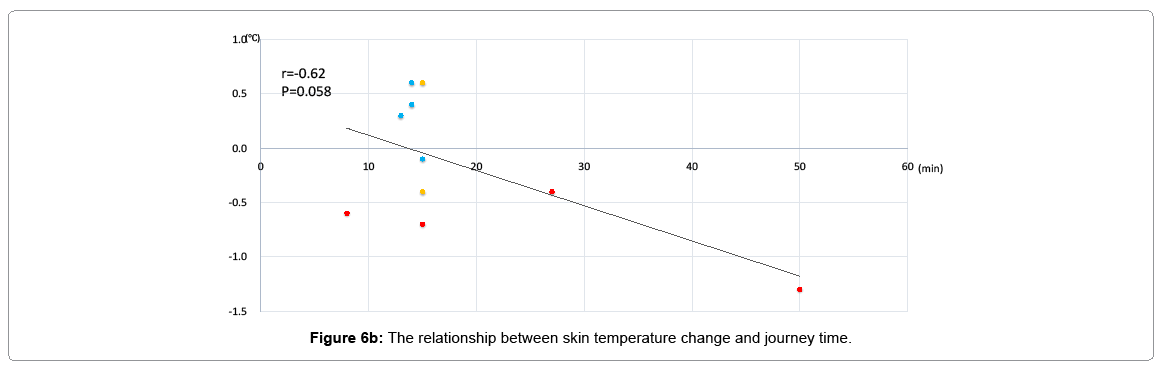
Four infants (three mild HIE infants, one moderate HIE infant) had elevated skin temperatures during transport. However no infants had high temperature greater than 37.5°C. All four infants of severe HIE had decreased skin temperatures during transport and showed lower skin temperatures than rectal temperatures at arrival. One overcooled preterm infant with severe HIE (34.0 weeks) showed lowest skin temperature (32.2°C) at arrival (Figure 5b). As the journey time becomes longer, both rectal and skin temperatures had a decrease tendency, but not significantly (p=0.081, p=0.058, respectively) (Figures 6a and 6b). The monitoring of rectal temperature was done without significant adverse events such as rectal bleeding. Two severe HIE infants had showed hypotension on arrival at cooling center. Blood pressures of them increased immediately after using catecholamine and volume expander.
Discussion
In Japan, about half of newborns were born in private clinics. So we need to transport newborns from clinics to hospitals when the newborn would show some clinical symptoms and need any medical investigation or treatment at hospital. During transport, we have checked only skin temperature of infants. However, some reports recently said that core temperature such as rectal or esophageal temperature is more important to indicate the metabolic, circulatory or central nerves system conditions of babies. Especially, infants with HIE show abnormal higher core temperature than skin temperature due to neuronal cell damage [7]. However, we have no reports about the relationship between skin temperature and core temperature during newborn transport in Japan. So firstly we investigate the relationship between skin temperature and rectal temperature using continuous monitoring system. In our study, infants without asphyxia showed significantly good correlation between skin temperature and rectal temperature. While as the journey time becomes longer, both rectal and skin temperatures had tendency of elevation. Furthermore we showed no case with hypothermia (< 35.0°C) during transport and all of 5 cases who showed rectal temperature <36.0°C at departure showed elevation of rectal temperature at arrival. So, transport protocol for newborns without asphyxia in Japan is relatively feasible and safe. However in two cases, only rectal temperatures showed decrease (≥ 0.4°C) in winter season. So continuous monitoring of rectal temperatures might be effective especially in winter season. We have limitation that many of journey time are around 15 minutes. We need further studies how length of journey and change of air temperature affect skin and rectal temperatures even in the case without asphyxia.
Therapeutic hypothermia has been shown to improve the outcome following perinatal asphyxia [1-6] and the standardized protocol of TH has spread all over Japan since Consensus [12,13] To obtain the maximum benefit, therapeutic hypothermia (TH) should be initiated as soon as possible within 6 h after birth [14,15]. Furthermore, it is thought that elevated core temperatures after asphyxial insults are associated with worse outcomes among HIE infants [7]. However, infants who were born at clinics in rural area might not be able to transport to cooling center and initiate therapeutic hypothermia within 6 h in Japan. Therefore it is truly essential to develop effective and safe methods of cooling during transport. There have been some reports about the effectiveness of pre-hospital cooling as progression of TH [4,8-11,16,17]. Johnston reported that it is safe to provide servo-controlled cooling during neonatal transport [18]. However, we do not have enough transporting amenities to use servo-controlled cooling system in Japan. On the other hand, it is known that passive cooling is more feasible during newborn transport like the situation in many other countries. Kendall reported that 67% cases got targeted temperature at admission and it took earlier to start TH safely by passive cooling during transport using continuous temperature monitoring [10]. So we evaluated the efficacy and safety of passive cooling using continuous monitoring of rectal temperatures during transport in this study. Ten infants with asphyxia were passively cooled during transport. No infants had high temperature >37.5°C and 5 infants (three severe HIE infants, one moderate HIE infant and one mild HIE infant) successfully got a rectal temperature at arrival of cooling centers between 34.5°C to 35.5°C. Five infants who needed to undergo TH had been achieved a target temperature (34.0°C) without delay. However, one preterm infant with severe HIE infant showed hypothermia (rectal temperature 32.9°C). Furthermore, as the journey time becomes longer and the severity of HIE worsen, both rectal and skin temperatures had a decrease tendency. We need to take careful attention to control body temperatures to avoid infants being overcooled during transport especially in the case of severe HIE or prematurity. In our study, passive cooling during transport could be effective to prevent hyperthermia and get targeted temperature (35.0 ± 0.5°C) at arrival of cooling centers for newborns with asphyxia, while it could not decrease temperature at all in some cases. And, we should not forget that passive cooling could induce overcooling in some cases [11]. Severe HIE cases sometimes easily show the symptom of hypothermia shortly after birth, and we experienced similar cases in our study. We should use continuous rectal temperature monitoring if we undergo passive cooling for newborns, especially in the case of severe HIE infants or preterm infants during longer transfer.
Conclusion
Passive cooling by controlling the transport incubator temperature for infants with HIE was relatively safe and could prevent to be elevated body temperature. However, there may be a risk of unintended excessive cooling, especially in severe HIE infants and preterm infants during longer transfer. We suggest that continuous monitoring of the rectal temperature to control body temperature during transport especially for passive cooling is mandatory and feasible. We need further studies to clarify protocols to control body temperature of infants during transport including passive cooling.
Limitation
The object size is limited in three cooling centers in the western side of Japan.
Many of journey time are around 15 minutes.
Acknowledgement
This study was supported by Grants-in-Aid from the Ministry of Health, Labor and Welfare, Japan. The authors are grateful to Prof. H. Sobajima.
References
- Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, et al. (2005) Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy.N Engl J Med 353: 1574-1584.
- Jacobs SE, Morley CJ, Inder TE, Stewart MJ, Smith KR, et al. (2011) Whole-body hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: a randomized controlled trial.Arch PediatrAdolesc Med 165: 692-700.
- Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, et al. (2009) Moderate hypothermia to treat perinatal asphyxial encephalopathy.N Engl J Med 361: 1349-1358.
- Eicher DJ, Wangner CL, Katikaneni LP, Hulsey TC, Bass WT, et al. (2005) Moderate hypothermia in neonatal encephalopathy: efficacy outcomes. PediatrNeurol 32:11-7
- Simbruner G, Mittal RA, Rohlmann F, Muche R (2010) Systemic hypothermia after neonatal encephalopathy: outcomes of neo.nEURO.network RCT. Pediatrics 126:e771-e778.
- Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, et al. (2013) Cooling for newborns with hypoxic ischemic encephalopathy. Cochrane Database Syst Rev1:CD003311.
- Laptook A, Tyson J, Shankaran S, McDonald S, Ehrenkranz R, et al. (2008) Elevated temperature after hypoxic-ischemic encephalopathy: Risk factor for adverse outcomes.Pediatrics 122: 491-499.
- Anderson ME, Longhofer TA, Phillips W, McRay DE (2007) Passive cooling to initiate hypothermia for transported encephalopathic newborns.J Perinatol 27: 592-593.
- Hallberg B, Olson L, Bartocci M, Edqvist I, Blennow M (2009) Passive induction of hypothermia during transport of asphyxiated infants: a risk of excessive cooling.ActaPaediatr 98: 942-946.
- Kendall GS, Kapetanakis A, Ratnavel N, Azzopardi D, Robertson NJ; Cooling on Retrieval Study Group (2010) Passive cooling for initiation of therapeutic hypothermia in neonatal encephalopathy.Arch Dis Child Fetal Neonatal Ed 95: F408-F412.
- O'Reilly D, Labrecque M, O'Melia M, Bacic J, Hansen A, et al. (2013) Passive cooling during transport of asphyxiated term newborns.J Perinatol 33: 435-440.
- Takenouchi T, Iwata O, Nabetani M, Tamura M (2012) Therapeutic hypothermia for neonatal encephalopathy: JSPNM & MHLW Japan Working Group Practice Guidelines Consensus Statement from the Working Group on Therapeutic Hypothermia for Neonatal Encephalopathy, Ministry of Health, Labor and Welfare (MHLW), Japan, and Japan Society for Perinatal and Neonatal Medicine (JSPNM). Brain Dev34:165-170.
- Iwata O, Nabetani M, Takenouchi T, Iwaibara T, Iwata S, et al. (2012) Working Group on Therapeutic Hypothermia for Neonatal Encephalopathy, Ministry of Health, Labor and Welfare, Japan; Japan Society for Perinatal and Neonatal Medicine. Hypothermia for neonatal encephalopathy: Nationwide Survey of Clinical Practice in Japan as of August 2010. Acta Paediatr101: e197-e202.
- Iwata O, Iwata S, Thornton JS, De Vita E, Bainbridge A, et al. (2007) "Therapeutic time window" duration decreases with increasing severity of cerebral hypoxia-ischaemia under normothermia and delayed hypothermia in newborn piglets.Brain Res 1154: 173-180.
- Thoresen M, Tooley J, Liu X, Jary S, Fleming P, et al. (2013) Time is brain: starting therapeutic hypothermia within three hours after birth improves motor outcome in asphyxiated newborns. Neonatology 104:228-33.
- Chaudhary R, Farrer K, Broster S, McRitchie L, Austin T (2013) Active versus passive cooling during neonatal transport.Pediatrics 132: 841-846.
- Akula VP, Joe P, Thusu K, Davis AS, Tamaresis JS, et al. (2015) A randomized clinical trial of therapeutic hypothermia mode during transport for neonatal encephalopathy.J Pediatr 166: 856-861.
- Johnston ED, Becher JC, Mitchell AP, Stenson BJ (2012) Provision of servo-controlled cooling during neonatal transport.Arch Dis Child Fetal Neonatal Ed 97: 365-367.
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 15394
- [From(publication date):
December-2015 - Jul 15, 2025] - Breakdown by view type
- HTML page views : 14326
- PDF downloads : 1068