Review Article Open Access
Teaching Patient-Centered Safety-Netting in Primary Care
Silverston P*University Campus Suffolk, Ipswich, United Kingdom
- Corresponding Author:
- Paul Silverston, BA Jt Hons, MBChB, PFHEA
Snailwell, Cambridgeshire, United Kingdom
Tel: +443-287-4843
Fax: 410-502-7029
E-mail: paul.silverston@btinternet.com
Received Date: June 06, 2016; Accepted Date: June 23, 2016; Published Date: June 30, 2016
Citation: Silverston P (2016) Teaching Patient-Centered Safety-Netting in Primary Care. J Community Med Health Educ 6:447. doi: 10.4172/2161-0711.1000447
Copyright: © 2016 Silverston P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
In primary care, it is common for patients to present during the early stages of illness with non-specific symptoms, at which time the positive clinical findings in the history and examination that enable a clinician to make a firm diagnosis, or to discriminate between a serious and minor illness, may not have developed. Where diagnostic uncertainty exists, there is a need for the doctor to provide safety-netting advice so as to reduce the risk of misdiagnosis inherent in making a diagnosis at this early stage in the patient’s illness. It is important that medical students and junior doctors learn the principles and practices of safety-netting, including the patient’s perspective of why safety-netting advice is required and how best to communicate this advice to the patient in a way that is comprehensible to them. This article discusses how simple visual models can be used in the teaching of safetynetting skills to help discuss the rationale for safety-netting with the patient.
Keywords
Primary care; Safety-netting advice; Models of illness; Safe practice; Protective medicine
Introduction
In 2011, the World Health Organisation published the Multi-Disciplinary Patient Safety Curriculum Guide in which the human and financial cost of medical errors worldwide was highlighted, along with the need to adopt a patient safety-centred approach to the practice of medicine [1]. In primary care, it can often be difficult to distinguish between a serious and a minor illness if the patient presents during the early stages of an illness, when symptoms may be non-specific and the clinical findings required to establish the diagnosis may not have developed. The resulting diagnostic uncertainty needs to be managed as safely as possible and one factor in achieving this is for the clinician to provide safety-netting information to the patient during the consultation [2,3]. The term “safety-netting” is used to describe an action or behaviour that covers the possibility that an adverse event may take place at a future time and in this case it describes information that is provided to cover the possibility that the patient’s condition may worsen, either because of diagnostic uncertainty at the time that the patient was first seen, or because of the potential for complications of that illness to occur. A good example of the principles and practices of safety-netting is seen in the advice issued to a patient who has sustained a head injury. Clinical assessment of the patient at that point in time has not revealed the presence of a serious head injury but it is recognised that bleeding and swelling of the brain may continue to occur after the initial assessment. As a result, the patient is sent home with specific instructions of symptoms and signs to look for that might indicate that further bleeding or swelling is taking place and the appropriate action to take if those warning signs begin to develop. The medical model of teaching safety-netting concentrates on delivering the medical content of the advice, in terms of what patients should look for and what to do if the existing symptoms worsen or fail to resolve within the expected time, or if new symptoms develop. Simply explaining to patients what they should be looking for without explaining why it is important that they do so may mean that the advice is not followed as closely as is required for the patient to be safe. The patient-centered approach to safety-netting seeks to provide the patient with an explanation as to why diagnostic uncertainty exists in medicine and thus why the clinician is providing them with safety-netting information, with the intention of ensuring that the patient truly appreciates the importance of following the advice that is provided. Safety-netting is an essential part of safe practice for both doctor and patient.
Teaching the Patient-Centered Approach
It is important that medical students and junior doctors learn how to deliver safety-netting advice in a way that is comprehensible to the patient. Safety-netting advice for specific conditions is relatively straightforward to develop and deliver but determining the medical content of the advice for provided for non-specific symptoms, such as a fever, is more complex, as not knowing which illness is developing makes it difficult to decide which patterns of illness and the red flags associated with these to share with the patient. Discussing safetynetting advice is similar to discussing the potential side-effects of drugs that are being prescribed, in that it is difficult to know how much information to disseminate, particularly when the risks are small but can cause great concern to the patient. Most packaged medication now comes with a data sheet included, which act as an aid in this discussion and, in the same way, it can be helpful for clinicians to have symptom and condition-based information sheets available to them to help aid the discussion about which symptoms and signs the patient should be looking for; how often to look for them; and what to do if they arise. Head injury advice sheets are routinely provided to all patients who are being sent home after being assessed for what appears to be a minor head injury and should be considered the “industry standard” for written safety-netting advice for such information sheets.
However, inexperienced doctors often comment that patients question their clinical competence and diagnostic abilities when they begin to discuss safety-netting advice with them because there is an expectation that a competent clinician is always able to make an accurate diagnosis. This assumption is reinforced by popular medical television programmes, such as “House”, where it appears that diagnostic uncertainty can always be solved by doing more investigations, or considering more esoteric diagnoses. If patients do not understand the limitations of clinical assessment in early illness and the difficulties of formulating a diagnosis when the positive findings required for this have yet to develop, then they will struggle with the concept of diagnostic uncertainty and the need for safetynetting advice to be provided. Inherent in the principles of safetynetting is the possibility that the doctor has not been able to make a firm diagnosis, or, indeed, may have made the wrong diagnosis, which, in the patient’s eyes may be associated with a failure to assess the patient thoroughly or competently, whilst to the clinician this is related to the relationship between illness, time and a single-point-in-time clinical assessment.
As clinicians, we accept that in early illness there are limitations to the effectiveness of clinical assessment, as the diagnostic reasoning process requires the presence of disease-specific clinical findings, which may only develop later in the illness. A child presenting a few hours into a febrile illness may have no other clinical findings to indicate the cause of the fever, or even whether or not there is a serious underlying cause, such as invasive meningococcal disease. A patient with a streptococcal sore throat may develop any one of a number of serious complications of that disease. A two-day history of loose stool may be looked back on later as being due to gastroenteritis, or, if it persists, as the beginning of altered bowel habit due to bowel cancer or inflammatory bowel disease. Safety-netting advice exists because diagnostic uncertainty exists but the existence of diagnostic uncertainty and the role that the relationship between illness, time and clinical assessment plays in diagnostic uncertainty is not always understood by the patient.
Explaining Diagnostic Uncertainty in Early Illness
The existence of diagnostic uncertainty is not always easy to accept, either for doctors, or for patients [4]. In family practice, one needs to learn about how to perform a competent and thorough clinical assessment but also what the limitations of clinical assessment are in early illness and when it is more appropriate to use time as a diagnostic tool, rather than performing investigations too early in the disease for the results to be positive and unequivocal. Knowing at what point in an illness there will be positive diagnostic findings in the history, clinical examination, or with tests and investigations is as important as knowing what to do in the way of a clinical assessment. Patients are often not aware of relationship between illness, time and clinical assessment and the way that the natural history of an illness influences the point in time when the diagnosis of that illness can be made, although they may well have experienced an illness where the symptoms and signs developed over time. A patient-centred approach to teaching safety-netting involves teaching the trainee to share with the patient how a diagnosis is formulated from positive and negative clinical findings in the clinical assessment and the way in which illnesses develop over time. Understanding this is fundamental to explaining to the patient why safety-netting is required and that it is not a reflection on the knowledge and skills of the clinician but is a result of the dynamic nature of illness and the clinical assessment process [5]. It is said that “a picture speaks a thousand words” and so it can be helpful to use simple visual models to explain these concepts during the consultation.
Using Visual Models in Patient-Centered Teaching
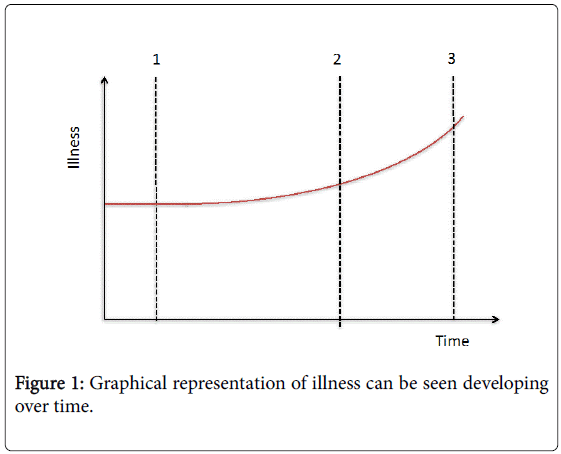
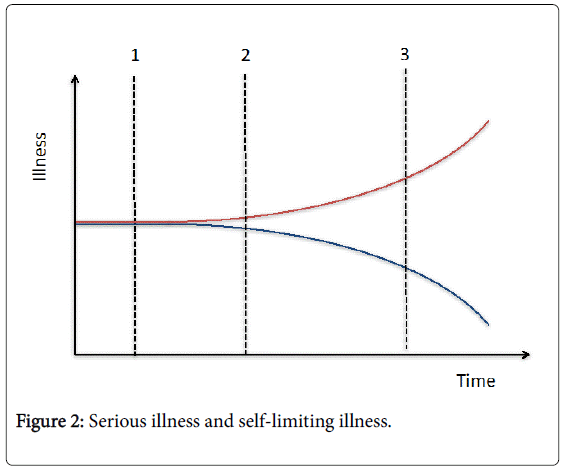
Simple, visual models can be used to help explain the relationship between symptoms, time and clinical assessment in teaching medical students and doctors to develop their safety-netting skills. In Figure 1, an illness can be seen developing over time, graphically. As time passes, the symptoms and signs of the illness increase and the number of positive diagnostic findings that can be elicited during a clinical assessment increases, making it more likely that certain illnesses can be excluded and a firm diagnosis reached. It will be easier for a doctor to establish the diagnosis at point 3 on the graph than at either point 1 or 2, as a result. This graph can be used to demonstrate two important factors, which are that symptoms and signs change over time and that a clinician can only find what has developed up to the point in time when the patient is assessed, not what will develop later in the illness. The Figure 2 features two illnesses, a “red line” serious illness, in which the symptoms and signs worsen over time and a “blue line” selflimiting illness, in which the symptoms and signs resolve over time [6]. At point 1 on the graph, it can be seen that a serious and a minor illness are indistinguishable, as the patient’s symptoms are likely to be non-specific (such as a fever, or headache) and the signs of a serious illness have yet to develop. At point 2 on the graph, subtle symptoms and signs are beginning to appear that will enable the clinician to distinguish between these two illnesses and at point 3 it will become clear that one is dealing with a serious illness.
These figures can be used to help trainees discuss with patients why a diagnosis might change over time from that of a minor illness to one of serious illness and why that diagnosis cannot be made earlier in the illness. Secondly, it enables them to discuss the specific symptoms and signs that would indicate that the patient is developing a serious “red line” illness, especially the earliest “red flag” symptoms and signs associated with point 2 on the graph, as well as those of late illness at point 3. Thirdly, it can be used to discuss the temporal element of making a diagnosis, in terms of how often a patient should be reassessed (the speed of progression from point 1 to point 2 for a serious illness) and the point in time when a minor illness should have resolved, which the distinguishes a serious illness from a minor illness (point 3). If one applies these figures to the natural history of a head injury initially assessed as being “minor”, one can easily explain the medical contents of the head injury advice sheet but also why time is being used as a diagnostic tool in an evolving disease process. The initial injury may not result in any clinical or radiological evidence of a serious head injury. Subsequent to that assessment the injury may progress, due to bleeding or swelling, resulting in the development of new symptoms and signs. The head injury advice sheet contains information on the earliest symptoms and signs of this happening, as well as the later ones and explains and emphasizes the need to monitor the patient for these occurring. Not only can these figures be used to aid communication skills teaching in providing safety-netting advice but they can also be used in delivering safety-netting advice to patients both verbally and in writing.
In Summary
In primary care, patients often present so early in an illness that it is not possible to determine whether the patient is in the early stages of a serious or a minor illness, as the diagnostic reasoning process requires the presence of positive and negative findings to formulate a diagnosis. The absence of these findings during the early stages of a serious illness can create diagnostic uncertainty, which needs to be managed safely through the provision of safety-netting advice. Safety-netting is an essential part of safe practice in primary care and the principles and best practices of this need to be taught in both undergraduate and postgraduate medical training programmes. There is evidence to suggest that incorporating a patient-centred approach into safetynetting advice information is beneficial and that advice is more likely to be acted upon by the patient, or their relatives [7]. Whilst some may see safety-netting as a form of defensive medicine, it should be seen as a form of “protective” medicine, there to protect both the patient and the doctor from the limitations of clinical assessment in early illness caused by the relationship between illness, time and clinical assessment and its impact on the diagnostic process. Simple visual models can be used in teaching safety-netting skills and also in the delivery of that advice.
References
- World Health Organisation (2011) Multi-Disciplinary Patient Safety Curriculum Guide.
- Neighbour R (1987) The inner consultation. Kluwer Academic Press, Lancaster.
- Silverston P (2014) The importance of teaching risk assessment and safety-netting skills in primary care.Primary Health Care.
- Silverston P, Stewart L (2014) Diagnosis Uncertain. Student BMJ 22: 28-29.
- Silverston P (2014)Effectivesafety-netting in prescribing practice. Nurse Prescribing 12: 349-352.
- Silverston P (2012) Using a model of illness to aid symptom-based learning in primary care. Educ Prim Care 23: 443-445.
- Lackhanpaul M, Neill S, Shang C, Thompson M (2012) Safety-netting information for the acutely sick child. Archives of Disease in Childhood 97: A494-A495.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 12768
- [From(publication date):
June-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 11823
- PDF downloads : 945