Teaching ENT in Primary Care
Received: 17-Mar-2016 / Accepted Date: 13-Apr-2016 / Published Date: 20-Apr-2016 DOI: 10.4172/2161-119X.1000228
251618Introduction
In the United Kingdom patients suffering from ENT problems are 10% of the workload of GPs and considering there are over 300 million consultations in primary care each year, ENT is one of the largest prevalent groups seen and managed by GPs in the community [1,2]. Otolaryngology as a speciality sits astride three important areas of acute life threatening emergencies, major oncological and reconstructive surgery and the largest volume of non-threatening ailments which nevertheless affect the quality of life of children and adults. The future of healthcare is significantly affected by the demographic changes of increasing longevity of life with chronic disease burden, end of life care, life style choices such as obesity, smoking, alcoholism and drug addiction as well as the social pressures of unemployment and poverty [3,4]. All of this will affect every aspect of medicine including Otolaryngology.
Part of medical leadership is to deal with ‘today’ and plan for ‘tomorrow’. The above demographic changes will seriously impact on the way health organisations are planned, led and patient care delivered [5]. To this extent higher specialist training curriculum in Otolaryngology is well developed, approved by the General Medical Council (GMC) and delivered through the Specialist Advisory Committee, the Royal Colleges and Deaneries. In addition for higher specialist Otolaryngology trainees there are well established interface fellowships funded by the Department of Health (DH) in Head and Neck cancer and Cleft, Lip and Palate [6]. On the other hand, undergraduate teaching in ENT is sparse, fragmented, lacks uniformity in creating a curriculum, the learning objectives, means of assessment and who should teach.
Health Education England aspires for 50% of medical school output to be based in primary care and the Shape of Training report foresees future medical school graduation to be at the level of full registration with the GMC [7,8]. Therefore in the speciality of primary care where the increasing burden of ENT falls, the way medical students are trained to deliver safe and timely patient care is crucial. The most recent publication “Specialists in out – of – hospital settings (2014)” by the King’s Fund encourages Consultants to work beyond their traditional boundaries, and the shift of specialist care to the community [9].
Inevitably this means more of the relevant ENT teaching of medical students should also be carried out in the primary care setting where the patients with common problems exist. This paper, addresses the need to develop a fit for purpose medical undergraduate Otolaryngology curriculum, based on sound principles of education and learning to support ENT teaching in the primary care setting.
What is a Curriculum?
There can be confusion between a syllabus and a curriculum. A syllabus is a list or a summary of topics to be covered in an education or training course. It is descriptive in nature and relates to what should be taught and not how it is taught. The curriculum dictates how education delivers the desired learning outcomes. This should cover generic, professional and speciality – specific areas. It is a statement of the intended aims and objectives, content, experiences, outcomes and processes of an educational programme. There needs to be an understanding of how students learn, how medicine is practised, social responsibility and accountability, professional values, attitudes and behaviours and increasingly how healthcare organisations are structured and financed [10,11]. In this context how students will be exposed to common ENT conditions and their management is relevant.
Delivering the Undergraduate ENT Curriculum
Medical school curriculum is crowded with variation of how ENT is taught. This is usually in the third year and the spending of the equivalent of 2 weeks whole time or less on an Otolaryngology ward, theatres and outpatients does little to prepare students for the challenges facing them with the common ENT conditions seen in primary care. The future will be more community care and inter-professional focussed. Students in the traditional teaching model in Otolaryngology inpatient beds in hospitals are exposed to head and neck cancer, thyroid disease and other complex tertiary referrals. In addition there are pressures from shorter patient stays and the increasing cohort of day case surgery making bedside teaching difficult. How then will students learn about the large number of patients who suffer with ear pain or discharge, sinusitis, tonsillitis, difficulty in swallowing and the exponential growth of elderly patients demanding help with deafness? None of them life threatening, but important for the patient, which in some cases can lead to repeat visits and increasing burden for the GP and hospital staff. This is relevant as the majority of students will not choose otolaryngology as a career.
A possible solution to the above problems is of a much closer working relationship between ENT staff and the GP, and, delivering the consultation, management and teaching in the primary care setting. This means that the curriculum and the students are based in primary care. Both the GP and the student gain from individual teaching and skilling up, and the patients benefit from consultation and swift diagnosis within the community. Due to the presence of the Read Code, it should be possible for GPs to set up ENT specific clinics in their surgeries. The students should also be encouraged to accompany any patient referred to the hospital, so that the teaching accompanies the patient journey, with the opportunity to understand care pathways and witness management of more complex cases. Such opportunistic learning in secondary care will balance the primary care teaching. These cases within the student portfolio should complement the common ENT problems presenting in the GP Surgery. In addition, the understanding of normal structures such as the surface anatomy of head and neck, ear drum and sinuses can be done in GP examination rooms while patients wait, as these examinations require simple, low cost equipment such as the auriscope and without the need for patients to undress.
Exposure in primary care will also support the development of team working skills, inter-professional working, leadership and situational awareness as well as the broader remit of professionalism.
Development of ENT Primary Care Services
The above initiatives will only work if the case for expansion of primary care undergraduate teaching is accepted. Primary care is the largest medical speciality and currently only of three years postgraduate duration, with a plan within Shape of Training to expand to 4 years, but has a DH caveat of the expansion being cost neutral [8]. Medical students on average only spend around 13% in primary care despite the fact that this is the main speciality that deals with the undiagnosed and undifferentiated problems across the spectrum of life, managing uncertainty and ambiguity with the largest number of patients exceeding 300 million consultations per year [3,12]. The driver for these needs to be clearly laid out in the ENT primary care curriculum. A suggested curriculum by no means exhaustive is shown in Tables 1a-1f.
| Presentation | Learning Outcome | Assessment |
|---|---|---|
| Painful Ear | Understanding of causes and management including temporomandibular problems, toothache and referred otalgia from head & neck neoplasia | Direct observation. CBD. Mini- CEX, Knowledge based tests. |
| Discharging ears | Otitis externa and chronic suppurative otitis media management. Swab and culture investigation of common organisms such as Strep.pneumoniae and haemophilusinfluenzae. Referral for persistent discharge suspecting Cholesteatoma. | |
| Sore throat | How to diagnose tonsillitis and when to use antibiotics. Who to refer for tonsillectomy. When to suspect carcinoma. | |
| Hearing loss including wax management | Types of hearing loss. The impact that hearing loss has on individuals and families. Removing wax. Hearing aid science and referral if asymmetrical, conductive or sudden. | |
| Hearing aids | Who would benefit from referral for a hearing aid | |
| Vertigo | Causes of dizziness, vertigo and unsteadiness. Difference between peripheral and central vestibular disorders including Falls Prevention. |
|
| Tinnitus | How to manage and educate patients including habituation versus masking strategies. | |
| Nasal obstruction, polyps and allergy | Topical and systemic treatments | |
| Sinus problems and facial pain | How to distinguish sinusitis from other causes of facial pain |
|
| Snoring and sleep apnoea | Assessment, advice and referral criteria | |
| Hoarse voice | Who to refer for laryngoscopy | |
| Difficulty in swallowing | Who to refer for further assessment | |
| Mouth ulcers | Use of oral steroids, antibiotics, anti-fungal Rx, mouth washes and local anaesthesia. Systemic causes. When to refer if biopsy indicated. | |
| Neck lumps | How to assess the neck for normal anatomy and the present of pathology in lymph nodes, salivary glands, the thyroid gland and other vascular structures. Who to refer for urgent needle biopsy and laryngoscopy. |
Table 1a: Example of an ENT curriculum within primary care: Common GP presentations.
| Presentation | Learning Outcome | Assessment |
|---|---|---|
| Foreign bodies | How to remove and when not to try | Direct Observation. PBA, CBD, knowledge based tests, clinical audit, critical incident reporting |
| Epistaxis | How to manage recurrent intermittent chronic bleeding and acute heavy bleeding | |
| Infections including suspected epiglottitis, orbital cellulitis and mastoiditis | When to suspect and when not to examine. | |
| Sudden onset sensorineural hearing loss | How to diagnose and treat early | |
| Airway obstruction and stridor | How to recognise, assess and refer. ABC of resuscitation |
|
| Facial nerve palsy | How to assess. Who to treat and how |
Table 1b: Example of an ENT curriculum within primary care: Emergencies in otolaryngology.
| Anatomy and Pathology | Learning Outcome | Assessment |
|---|---|---|
| Normal ear. External ear structures and inspection of the drum. | Learn about the light reflex/ cone of light. Use the ear drum as a window into the middle ear. Application of Weber and Rinne’s test. Examination of cranial nerves. | Direct Observation such as Mini-CEX, PBA, DOPS, Patient ratings, Educational Supervisors report, |
| Common ear abnormalities and pathological conditions | Perforation, tympanosclerosis, glue ear/ middle ear effusion, retraction of the drum, haemotympanum and how to check facial nerve function. | |
| Nose. Inspection of nose from front, side, above and below. | Focus on size, shape, swelling, scars and any deviation. Assessment for intra-nasal oedema, obstruction by polyps, turbinate enlargement, grossseptal deviation, discharge, crusting and any offensive smell. Become aware of anterior rhinoscopy and flexible fibreoptic nasal endoscopy | |
| Throat examination | How to remove dentures and examine the mouth systemically using a bright torch, tongue depressor and a nasopharynx mirror. This includes examination of the tongue, hard and soft palate, tonsillar fossa, gingivolabial/gingivobuccal sulci, floor of the mouth and the undersurface of the tongue. Indirect mirror examination. How to systematically palpate the neck, thyroid and salivary glands. |
Table 1c: Example of an ENT curriculum within primary care: Clinical examination.
| Drugs | Learning Outcome | Assessment |
|---|---|---|
| Vestibular sedatives -prochlorperazine, cinnarizine | Understanding management of an acute vestibular crisis including Ménière’s disease. Impact of drugs in the elderly and common side-effects. | Drug prescribing test. CBD, MSF, patient feedback. |
| Steroid nasal sprays and drops e.g. beclomethathsone/ betamethasone | Mode of action such as impact of vasoconstriction of mucosal blood vessels. Length of action | |
| Oral steroids (e.g. prednisolone) | Indications and side effects of prolonged use. | |
| Oral antibiotics | Awareness of commonly used regimes for acute tonsillitis/sinusitis. Risk of amoxicillin in glandular fever. | |
| Topical antibiotic drops in ENT | Awareness antibiotics may be combined with antibacterial or antifungal with steroids. Risk of hypersensitivity. | |
| Topical nasal decongestants | Awareness of dangers of prolonged use i.e. rebound congestion | |
| Topical nasal ointments | Awareness of role of naseptin to improve nasal hygiene and minimise nasal bleeding and crusting | |
| Analgesia | Appropriate use of analgesia in ENT infections, including otitis media |
Table 1d: Example of an ENT curriculum within primary care: Use of drugs in common ENT conditions.
| Other Professional Groups | Learning Outcome | Assessment |
|---|---|---|
| Audiologist and hearing department | How acute and chronic hearing loss is investigated. Audiogram, conductive and sensorineural hearing loss. Managing deafness in the community. Hearing aids | MSF, patient ratings, reflection account, Mini-CEX, CBD, DOPS, direct observation. |
| Vestibular rehabilitation physiotherapy | How to reduce dizziness, vertigo and falls in patients with balance disorders. | |
| Speech therapy | Impact on the lives of patients with laryngectomy. Part of a wider multidisciplinary team treating head and neck cancer and children with speech delay. | |
| Practice and district nurses | Community support for medical and social reasons | |
| Oncology support such as Macmillan nurses | Opportunity to visit patients at home, discuss cancer diagnosis and end of life care |
Table 1e: Example of an ENT Curriculum within primary care: Interprofessional learning and team working.
| Role of the Student | Learning Outcome | Assessment |
|---|---|---|
| Student as a learner | Self-directed deep learning | Presentations, portfolio reflective accounts, MSF, direct observation. Small group working |
| Student as a teacher | Presentations, audit | |
| Student as a leader | Values, empathetic trait, patient-centred, punctuality | |
| Student as a manager | Commissioning of health care. |
Table 1f: Example of an ENT curriculum within primary care: The student’s professional development to understand the wider role of a doctor.
Education basis of Developing the Primary Care ENT Curriculum
Development of a new curriculum model has to recognise the impact of learning research and theory. The emphasis has changed from what and how to teach, to how students learn and learning styles which has to ensure that the design of the curriculum has to accommodate such a pedagogical model.
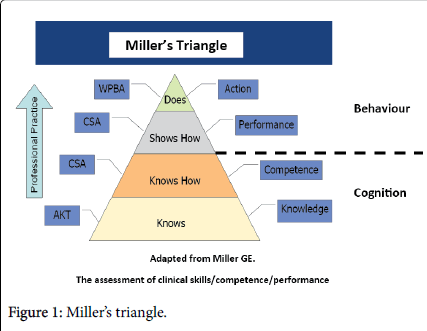
Medical education fits in five domains: knowledge and understanding, generic skills, cognitive skills and importantly that of attitude and behaviour. Therefore the ENT curriculum will need to build on the integrated curriculum of basic science with direct patient contact. The components of this clinical experience will build on the knowledge gained, skills and attitudes, judgement, problem solving, reflection, professionalism through working as teams and identifying with the values of society.
The learning outcomes are often defined in terms of what the student can do. It is equally important to define the conditions in which the student can be expected to perform the task and the competencies achieved (Figure 1) [13].
The ENT Curriculum should
Clarify the expected learning outcomes
Deliver a programme with appropriate learning opportunities
Support and facilitate the student’s learning
Assess the learner’s progress in achieving the set goals
To enhance medical student teaching the key principles of learning (FAIR) need to be enforced. These are
Feedback
Students need to be given feedback on their learning of expected outcomes but also help them become critical reflectors of their own performance, in other words self-feedback is important. Feedback highlights what is expected of the learner, reinforce good performance, correct mistakes and motivate the student who can then plan further study to address any deficiencies and reduce anxiety.
Activity
Students need to engage in active rather than passive learning. Such student centred learning leads to more deeper and meaningful learning.
Individualisation
Relate the learning to the needs of the individual student. Thus they need to have different range of learning opportunities, resources and experiences.
Relevance
The learning needs to be relevant to the student’s career objectives. Students do need to be protected from information overload and the learning outcomes should be complimentary to the defined curriculum. This drives outcome based education.
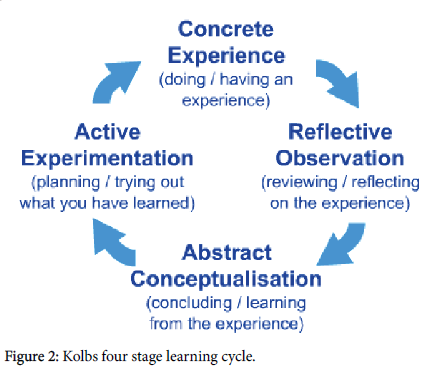
To understand how students learn we need to understand cognition – the act or process of knowing how students gain and organise their knowledge. Effective learning requires personal involvement, stimulation of feelings and thinking, self-initiation and self-evaluation. This humanist theory places the student at the centre of the learning process [14]. Students seek a purpose and have a cognitive map [15,16]. Learners can construct meaning for themselves and knowledge is not independent of meaning but dependent on communication, language, demeanour and doctor-patient interaction. A key part is reflection. New knowledge has to be grasped, often in an experiential setting of a patient consultation and transformed to the individual learner. Education thus becomes the reorganisation of experience [17].
Kolb’s four stage learning cycle (Figure 2) complements the above demonstrating that learning consists of acquiring new information, transforming that learning with regard to existing knowledge and then utilising it in new situations. Medical students are adult learners and need encouragement to be self-directed, understand the curriculum which should be relevant to their needs and take responsibility for their own learning [18].
This means that self-assessment is as important as teacher assessment. As a person matures, the self-concept of being a dependent student changes to one of being a self-directed professional. The motivation to learn becomes internalised and the maturity is reflected from subject centeredness to one of problem solving leading to deep learning.
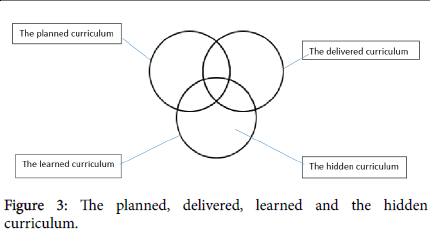
The curriculum should be sequenced as a constructive alignment of aim, objectives, delivery, assessment and evaluation. However a distinction needs to be made between the planned curriculum which is agreed, and the actual curriculum that is delivered, and the learned curriculum which represents the student’s knowledge, skills and attitudes that result from their learning experience. There needs to be an appreciation that part of the learned curriculum is the ‘hidden curriculum’ which is not part of the explicit planned curriculum such as attitudes and beliefs. This can often be related to the educational environment and the student’s experience of what is emphasised, rewarded and encouraged (Figure 3) [11].
All courses need to be assessed so that we can give feedback to students about their progress and motivate them. In addition assessment establishes a record of progress and can be used as a basis for future learning. Reasons for the interest in monitoring performance include well-publicised failures in health care, public concern about the quality of doctors in the UK and patient safety [19]. In addition, higher public demands for excellence in medical care are also recognised perhaps related to the rapid expansion of medical information and a growing consumer culture within healthcare. There are many different types of assessment (Table 2) and in choosing, the methodology should be reliable, valid and practical to undertake.
| Direct Observation | Multi-source Feedback | Routinely Generated Student Portfolio Data | Knowledge Based Tests |
|---|---|---|---|
| Directly Observed Procedural Skills (DOPS) | Colleagues, clinical and non-clinical | Case-based discussion (CBD) | Multiple Choice Questions |
| Mini-clinical evaluation exercise (Mini-CEX) | Patient ratings | Prescribing habits | Best of Five answers |
| Procedure-based Assessment (PBA) | Educational Supervisors report | Morbidity and mortality data | Essays |
| Video consultations | Critical incident review | Project assignments | |
| Objective Structured Clinical Examination (OSCE) | Significant event reporting | Quiz | |
| Clinical audit | Short-Answer Questions | ||
| Reflection accounts | Viva / Viva Voce / Oral | ||
| Index clinical cases | Spot tests – pictures and videos |
Table 2: Common methods of assessment.
A key point about the primary care ENT curriculum is that ENT presentations can be addressed throughout the placement which can add flexibility to delivering the overall curriculum and its evaluation. Such evaluation which is “the process of obtaining information about a course or programme of teaching, for subsequent judgment and decision making of future learning and development” allows constructive feedback and improvement [20].
Conclusion
ENT Consultants will need to adjust to different ways of working and teaching with closer liaison between the primary and secondary care. The ENT curriculum for medical students will need to be redesigned to local commissioning and be an iterative process. On the basis of assessment and evaluation findings, the curriculum should be regularly reviewed to ensure it remains fit for purpose.
References
- Griffiths E (1979) Incidence of ENT problems in general practice. J R Soc Med 72: 740-742.
- Gp Taskforce Final Report (2014) Securing the Future GP Workforce Delivering the Mandate on GP Expansion pp:1-63.
- Sandhu DPS (2015) How can we create a curriculum fit for tomorrow’s doctors and patients? British Medical Journal Careers.
- Smith J, Holder H, Edwards E, Maybin J, Parker H, et al. (2013) Securing the future of general practice: new models of primary care, London. Nuffield Trust and The King’s Fund.
- https://www.rcplondon.ac.uk/projects/outputs/future-hospital-commission
- Lees V, Henley M, Sandhu DPS (2010) Interface Specialty Training in the United Kingdom. Ann R CollSurgEngl 92:126-128.
- Department of Health (2013) Delivering high quality, effective, compassionate care: Developing the right people with the right skills and the right values. A mandate from the Government to Health Education April 2013 to March 2015 England.
- Robertson R, Sonola L, Honeyman M, Brooke B, Kothari S (2014) Specialists in out-of-hospital settings. The King’s Fund, London.
- Grant J (2010) Principles of curriculum design. In: Swanwick T (ed.) Understanding medical education. Evidence, theory and practice pp:1-15.
- Harden RM, Laidlaw JM (2012) Essential skills for a medical teacher. An introduction to teaching and learning in medicine. Churchill Livingstone Elsevier.
- Jones R, Stephenson A (2008) Quality assurance of community based undergraduate medical curricula: a cross sectional survey. Educ Prim Care 19:135-142.
- Miller GE (1990) The assessment of clinical skills/competence/performance. Acad Med 65: S63-67.
- Knowles MS (1983) Andragogy: an emerging technology for adult learning. In: Tight M. Adult Learning and Education. London, Croom Helm.
- Morris C, Blaney D (2010) Work based learning. In: Swanwick T (ed.) Understanding medical education. Evidence, theory and practicepp:69-82.
- Schon DA (1987) Educating the reflective practitioner: Toward a new design for teaching and learning in the professions. Jossey-Bass.
- Kolb DA (1984) Experiential learning: Experience as the source of learning and development. Englewood Cliffs, NJ, Prentice Hall.
- The Mid Staffordshire NHS Foundation Trust Public Inquiry (2013) London: The Stationary Office.
- Wall D (2010) Evaluation: improving practice, influencing policy. In: Swanwick T (ed.) Understanding medical education. Evidence, theory and practice, Wiley-Blackwell, Oxford, UK pp:336-351.
Citation: Sandhu DPS, Waddell A (2016) Teaching ENT in Primary Care. Otolaryngol (Sunnyvale) 6:228. DOI: 10.4172/2161-119X.1000228
Copyright: © 2016 Sandhu DPS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 13267
- [From(publication date): 4-2016 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 12378
- PDF downloads: 889