Systematic Review on Neurological Manifestations of COVID-19 Corona Virus
Received: 18-Jun-2020 / Accepted Date: 03-Jul-2020 / Published Date: 10-Jul-2020
Abstract
COVID-19 patients are reported to be presented with neurological symptoms. This systematic review includes 1,303 COVID-19 patients of 12 articles who had neurological manifestations. Eight articles were prospective case series and three were case reports. Commonest neurological presentation was headache followed by impaired conscious level, seizure, dizziness, cerebral vascular problem and loss of taste and smell. Previous studies supported that Corona virus can cause encephalitis, multiple sclerosis or cerebral hemorrhage. Respiratory failure due to damage of cardiorespiratory center of brainstem by COVID-19 virus has not been ruled out.
Keywords: COVID-19; Corona virus (CoV); Neurological manifestation
Introduction
The genome of SARS-CoV-2 is a 29,903bp single-abandoned RNA (ss-RNA) coronavirus [1]. First announced clinical highlights of 41 patients affirmed to be tainted with COVID-19 on January 2, 2020, which incorporate 13 ICU cases and 28 non-ICU cases [2]. The greater part of the cases (66%) had been presented to the Huanan Seafood Wholesale Market. Practically all the patients had respective lung ground glass opacities on high resolution computed tomography (HRCT) of chest. The underlying side effects included fever (98%), cough (76%), dyspnea (55%), myalgia or weakness (44%), sputum creation (28%), cerebral pain (8%), hemoptysis (5%), and loose motion (3%). Just a single patient didn’t present fever in the onset of illness. Twelve (29%) cases advanced to intense respiratory misery condition (ARDS), 5 (12%) had intense heart injury, 3 (7%) had intense kidney injury (AKI), and 3 (7%) presented with shock. At the information cutoff date, 28 (68%) patients were released and 6 (15%) had died.
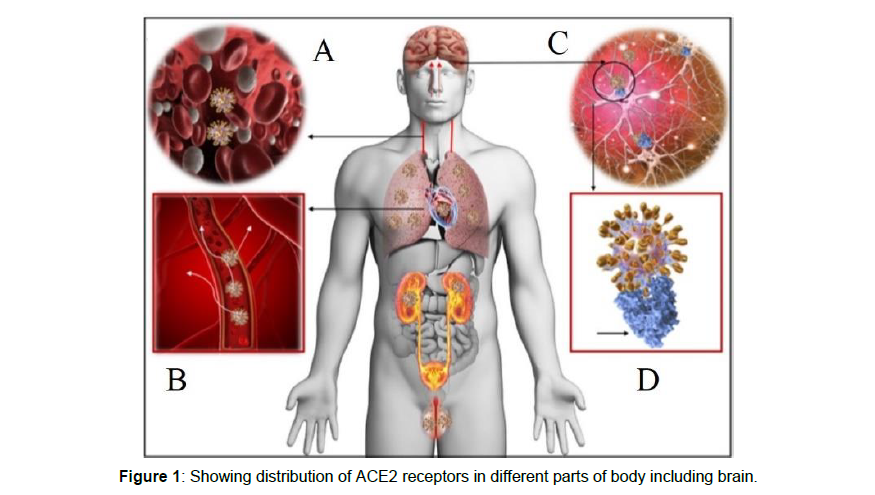
It has been documented in past that brain expresses ACE2 receptors Figure 1 [3]. Viremia helps to spread the COVID-19 infection all through the body by means of the circulatory system Figure 1 A-B. Neurotropism may happen by means of flow as well as an upper nasal course that empowers the COVID-19 to arrive at the cerebrum and tie and connect with the ACE2 receptors Figure 1 C-D. COVID-19 attaches with the ACE2 by means of spike protein over glial cells and neurons, which makes them a potential objective of COVID-19. The spread of COVID-19 in the fundamental dissemination or over the cribriform plate of the ethmoid bone during an early or later period of the contamination can prompt cerebral association as has been accounted for in the past for SARS-CoV affected patients [3]. The nearness of the COVID-19 infection in the general flow justifiably empowers it to go into the cerebral course where the sluggish flow of the blood inside the microcirculation could be one of the variables that may encourage the communication of the COVID-19 infection spike protein with ACE2 communicated in the slim endothelium. Ensuing sprouting of the viral particles from the fine endothelium and harm to the endothelial coating can support viral access to the cerebrum Figure 1B. It is thought that, some time before the neuronal damage occurs, the endothelial rupture in cerebral vessels inside the cerebral tissue can have fatal results in patients with COVID-19 contaminations. The development of the COVID-19 infection to the brain by means of the cribriform plate near the olfactory bulb can be an extra pathway that could empower the infection to reach and affect the cerebrum. Furthermore, the findings like a decreased smell sensation or hyposmia in a simple beginning period COVID19 patient ought to be examined altogether for CNS association. In the SARS-CoV contaminations that were accounted for previously, post-mortem findings of the patients have demonstrated strong evidence of the nearness of SARS-CoV by electron microscopy, immunohistochemistry and constant opposite transcription PCR [3]. Patients with intense SARS-CoV showed presence of infection in cerebrospinal fluid (CSF). The function of the blood-brain barrier in containing the infection and keeping it from accessing the neural tissues yet to be confirmed in patients diagnosed as COVID-19 [4]. Moreover, few patients who had loss of automatic control over breathing during the COVID-19 pandemic suffering intense respiratory failure compelled clinicians to isolate COVID-19 patients into neurologically affected cases and the individuals who are without neurological deficits.
Materials And Methods
Inclusion criteria: Articles on COVID-19 patients suffered from neurological manifestations were included in this study. Exclusion criteria: Articles on COVID-19 patients with other than neurological manifestations, articles with incomplete information about clinical feature and of low reliability were excluded from the study. Rationale of the study was confirmed by the researchers after studying related previous studies. Objectives were set according to PICOS guideline. Review question was set as if the COVID-19 patients may develop neurological manifestations or not? All diagnosed cases of covid-19 had neurological manifestations were included in the studies. Protocol was made according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline. After discussing the methodology, two researchers collected related articles from PubMed, Web of science and Google search engine. Reference manager software Mendeley was used to search from database, sorting according to references and saving and sharing the articles. Individual researchers prepared separate logs using unique IDs. Both the researchers then consulted together and sorted the articles according to the references, selection criterion, statistical analysis and outcomes of the articles and moved for the second log. Second log was comprised of references, number of the participants, types of the statistical analysis, outcome measuring and the types of study. Studies accepted by both the researchers were included. Second set of unique IDs were allotted for finally accepted studies. After preparing the final Table 1, all the results of the studies were tabulated and compared.
| Author | Types of study | No. | Neurological findings & percentage | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Headache | dizziness | ICL | CVS problem | Ataxia | Seizure | Smell lost |
Taste lost | ANS | |||
| Mao | RCS | 214 | 13 | 17 | 8 | 3 | 0.5 | 0.5 | |||
| Lee | RCS | 221 | 6 | ||||||||
| Huang | PCS | 41 | 8 | ||||||||
| Yang | RCS | 52 | 6 | ||||||||
| Wang | RCS | 138 | 7 | 9 | |||||||
| Chen | RCS | 99 | 8 | 9 | |||||||
| Sijia | RCS | 262 | 6.5 | ||||||||
| Yeshun | RCS | 214 | 36.5 | ||||||||
| Sandeep | CR | 1 | 100 | ||||||||
| Asia | CR | 1 | 100 | 100 | |||||||
| Carol H | CS | 59 | 68 | 71 | |||||||
| Rong | CR | 1 | 100 | ||||||||
| Total-1303 | |||||||||||
Table 1: Shows different articles on different types neurological manifestations presented by COVID-19 patients.
RCS- retrospective case series, ICL- impaired conscious level, PCS- prospective case series, CR- case report, ANS- average neurological symptoms, CS- cross sectional.
Results
Results illustrated that total 12 articles were reviewed. Total 1303 COVID-19 patients were included in these articles. Out of these articles, 8 articles were prospective case series, 3 were case reports and one was case series. Headache was commonest neurological feature presented in 6 studies. Impaired conscious level was present in onethird studies. Seizure was presenting feature in 3 studies. In one study nearly one-third patients presented with neurological manifestations. Other presenting features were dizziness, cardiovascular problem including stroke, ataxia, smell disturbance and taste disturbance. The study reviewed the result of 6 articles where all the series had patients with CNS manifestation [5]. According the study they have done retrospective case series study on 214 admitted patients among whom 25% had CNS manifestation. Out of them 13% had headache, 17% had dizziness, 8% had impair consciousness. Presentations like acute cerebral stroke, ataxia and seizure were in 3%, 0.5% and 0.5% patients respectively [6]. In the series of study, it is performed their retrospective case series on 221 Covid-19 patients. Among the patients 5% presented with acute ischemic stroke [7]. Other CNS presentations were cerebral venous thrombosis (0.5%) and cerebral hemorrhage (0.5%). A prospective study has been published in which on 41 patients of them 8% were presented with headache [8]. Retrospective study was on 52 critically ill patients and headache was present in 6% cases [9]. Another retrospective study showed that among 138 patients 9% had dizziness and 7% had headache [10]. In series of experiments carried out (total patients 99) they found confusion in 9% patients and headache in 7% patients [11]. CSF analysis or EEG study was not done in any studies.
Discussion
Sijia Tian et al. publisher article on the characteristics of Covid-19 patients of Beijing. Among total 262 patients, 17% were severe cases [12]. Nearly half of the patients were male and the average age of the patients was 47 years. Commonest presentation at the onset of covid-19 was fever (82.1%). Yeshun et al found more than one third patients presented with ANS complaint in their RCS of 214 cases [13]. Other features were cough (45.8%), headache (6.5%), dyspnea (6.9) and fatigue (26.3%). Sandeep et al reported a case of COVID-19 patient who had developed seizure [14]. A 72-year old man presented with weakness and dizziness who had history of diabetes, chronic kidney disease, hypertension and coronary artery disease. He was reported positive for COVID-19. CT head showed chronic micro vascular ischemic changes without any hemorrhage or infarction. CT scan chest revealed right lower lobe consolidation with both sided lung opacity. On day 3 of admission, patient developed multiple episodes of generalized tonic colonic seizure which lasted for few minutes. He was administered levetiracetam, initially loading dose and followed by maintenance dose. A 24-hour EEG revealed left temporal seizures and left temporal sharp waves which were epileptogenic. On the fifth day of hospital admission he became pulse less and collapsed. The resuscitation attempt was failed and the patient died. According to the case report of Asia et al one 74-year-old male was presented with cough and fever [15]. He was suffering from Parkinson disease, atrial fibrillation and chronic obstructive pulmonary disease (COPD). CT chest typically featured patchy bibasilar consolidations and sub pleural opacities. His COVID-19 result came as positive. On examination, the patient was unresponsive, aphasic with deteriorated cognition level. He did not have any gross motor deficiency. There was no nuchal rigidity. The CT scan of the head showed presence of an area of encephalomalacia in the left temporal region, which was most likely due to his previous cerebral infarction. The EEG showed bilateral slowing and focal slowing in the left temporal region with sharply countered waves. Cerebrospinal fluid (CSF) analysis by lumbar puncture was unremarkable for central nervous system infection. Later on, the patient developed respiratory failure and required intubation and was transferred to the ICU. One single-institute cross-sectional study was performed on 59 COVID-19 positive and 203 COVID-19 negative patients who presented with flu like symptoms. Chemosensory Dysfunction was compared in both the groups [16]. Smell and taste loss were respectively reported in 68% and 71% of COVID-19 -positive subjects, compared to 16% and 17% of COVID-19 -negative patients (p<0.001). The result was statistically significant. Smell and taste impairment were independently and strongly associated with Covid-19-positivity. It was concluded that otherwise asymptomatic cases with influenzalike symptoms, chemosensory dysfunction was strongly associated with Covid-19 infection and should be considered when screening symptoms. Rong Yin et al published their case report on a 64-year old male from Wuhan city who had complaint of raised temperature and mild cough [17]. Then one day 11 of symptom he started becoming lethargic and impaired conscious level. CT scan of brain was unremarkable but CT scan of chest showed peripheral opacities. His oxygen saturation was 88% without oxygen and 98% with 5-liter oxygen by nasal cannula. Throat swab sent on day 12 reported as COVID-19 positive. His signs of meningeal irritation like neck rigidity, Brudzinski sign and upper motor neuron lesion signs like Babinski and Chaddock were positive. Eventually lumbar puncture was done for CSF analysis and resulted as intracranial pressure of 200 mm of H2O with colorless and clear CSF. CSF protein was 275.5 mg/L and other CSF parameters were normal. The CSF was tested negative for the 2019-nCoV nucleic acid test. He started improving from day 27 of symptoms and gradually his CT chest became normal. His conscious level and neurological findings improved markedly. He was able to maintain 99% oxygen saturation without any oxygen supplement. His consecutive two throat swab test reported negative on day 27 and day 29. Autopsy report of COVID19 patients revealed brain edema and cerebral degeneration [18]. For the first time in the pandemic period COVID19 patient presented with viral encephalitis. It was also confirmed by genome sequence that SARS-CoV-2 was present in the CSF of affected patient. It is evident that ACE2 is essentially required for SARS-CoV-2 to infect cells [19]. The function of ACE2 signaling is to lower blood pressure. Hypertension patients has reduced expression of ACE2 that is why the ability of ACE2 to lower blood pressure is significantly reduced in COVID-19 patients. After getting infected by SARS-CoV-2, the function and expression of ACE2 proteins get reduced. As because the expression of ACE2 in hypertensive patients are already low so COVID-19 infection enhances cerebral hemorrhage in these patients. According to a hypothesis, patients with COVID-19 frequently suffer from coagulopathy and prolonged prothrombin time, both of which are responsible for secondary cerebral hemorrhage. COVID-19 patients may have increased in D- dimers, which can lead to thrombotic vascular events [20]. Corona Virus (CoV) infection has been proposed as a contributing factor in the pathogenesis of multiple sclerosis (MS) [21]. This hypothesis was supported by findings from studies. Coronavirus like particles have been detected in autopsied brain tissue from a patient with MS. CoV was isolated in autopsied brain tissue from 2 patients with MS. Another study reported intrathecal synthesis of antibodies to human CoV which suggested CNS infection. Human CoV RNA has also been detected from the CSF of patients suffering from MS [22]. Previous studies documented presence of viruses in the brain of SARS patients especially in the neurons. Experimental studies using transgenic mice further uncovered that either SARSCoV34 or MERS‐COV, when given intranasally, could enter the brain, perhaps through the olfactory nerves, and from there on quickly spread to some particular parts of brain including thalamus and brainstem [23]. It is critical that in the mice infected with low virulence of MERS‐CoV infection particles were recognized distinctly in the cerebrum, however not in the lung, which shows that the CNS infection was significant for the high mortality in infected mice. Among the infected brain regions, the brainstem has been exhibited to be intensely involved by SARS‐CoVor MERS‐CoV. In the brainstem most infected regions included the nucleus of the solitary tract and nucleus ambigus. The nucleus of the solitary tract receives sensory information from the mechanoreceptors and chemo receptors in the lung and respiratory tracts. These neuroanatomic interconnections highlight that the death of CoV infected animals or patients may occur due to the damage of the cardio respiratory vital center in the brainstem [24].
Conclusion
COVID-19 is a Corona virus like SARS and MERS viruses. Patients suffering from this disease can present with different symptoms including neurological manifestations. Some patients may present exclusively with neurological symptoms without having any flue like symptoms. Previous studies showed evidences of encephalitis, multiple sclerosis, cerebral hemorrhage and importantly respiratory failure in Corona affected patients. Enough animal and human studies are required support these findings in case of COVID-19.
Conflict of Interest
None of the co-authors declared any conflict of interest related to this article.
References
- Baig AM, Khaleeq A, Ali U, Syeda H (2020) Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction and Proposed Neurotropic Mechanisms. ACS Chem Neurosci. 11: 995-98
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497-506.
- Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S (2008) Severe acute respiratory syndrome corona virus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol 82 15: 7264-75
- Li YC, Bai WZ, Hashikawa T (2020) The neuro invasive potential of SARS-CoV2 may be at least partially responsible for the respiratory failure of COVID-19 patients. J Med Virol 92: 552-55.
- Ali A, Pooya A, Simani L (2020) Central nervous system manifestations of COVID-19: A systematic review. J Neuro Sci 413: 116832.
- Mao L, Wang M, Chen S (2020) Neurological Manifestations of Hospitalized Patients with COVID-19 in Wuhan, China: a Retrospective Case Series Study. J Elect SSRN 2139.
- Li Y, Wang M, Zhou Y (2020) Acute Cerebrovascular Disease Following COVID-19: A Single Center, Retrospective, Observational Study. Case Rep Neurol 12: 199-209.
- Huang C, Wang Y, Li X (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. J Lancet 395: 497-506.
- Yang X, Yu Y, Xu J (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 8: 475-81.
- Wang D, Hu B, Hu C (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus infected pneumonia in Wuhan, China. Jama 323: 1061.
- Chen N, Zhou M, Dong X (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel corona virus pneumonia in Wuhan, China: a descriptive study. Lancet 395: 507-13.
- Tian S, Hu N, Lou J, Niu S, Zhang L, et al. (2020) Characteristics of COVID-19 Infection In Beijing. Journal of Infect 80: 401-06.
- Wu Y, XU X, Chen Z, Duan J, Hashimoto K, et al. (2020) Nervous system involvement after infection with COVID -19 and other corona viruses. Brain Behav Immun 87: 18-22.
- Sohal S, Mansur M (2020) COVID-19 Presenting with Seizures. IDCases 20: e00782.Â
- Filatov A, Sharma P, Hindi F, Espinosa P (2020) Neurological Complications of Corona virus Disease (COVID-19): Encephalopathy. Â J Cureus 12: e7352.
- Yan HC, Faraji F, Prajapati DP, Boone CE, DeConde AS (2020) Association of Chemosensory Dysfunction and Covid-19 in Patients Presenting with Influenza-like Symptoms. Wiley Online Library.
- Yin R, Feng W, Wang T, Chen G, Wu T, et al (2020) Concomitant neurological symptoms observed in a patient diagnosed with corona virus disease 2019. J Med Virol.
- Xiang P, Xu XM, Gao LL, Wang HZ, Xiong HF, et al. (2020) First case of 2019 novel corona virus disease with Encephalitis. China Xiv 18: 1.
- Â Wang HY, Li XL, Yan ZR (2020) Potential neurological symptoms of COVID-19. Therap Adv Neuro Dis 13: 175628642091783
- Xu X, Chen P, Wang J (2020) Evolution of the novel corona virus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci 63: 457-60.
- Talbot PJ (1997) Virus-induced autoimmunity in multiple sclerosis: The corona virus paradigm. Adv Clin Neurosci 7: 215-33.
- Bonavia A, Arbour N, Yong VW, Talbot PJ (1997) Infection of primary cultures of human neural cells by human corona viruses 229E and OC43. J Virol 71: 800-06.
- Li K, C WL, Perlman S (2016) Middle East respiratory syndrome corona virus causes multiple organ damage and lethal disease in mice transgenic for human dipeptidyl peptidase 4. J Infect Dis 213: 712-22.
- Matsuda K, Park CH, Sunden Y (2004) The vagus nerve is one route of transneural invasion for intranasally inoculated influenza a virus in mice. Â J Vet Pathol. 41: 101- 07.
Citation: Talha A, Selina F, Nasir M, Rahman M, Islam S, et al. (2020) Systematic Review on Neurological Manifestations of COVID-19 Corona Virus. J Neuroinfect Dis 11: 291.
Copyright: © 2020 Talha A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3033
- [From(publication date): 0-2020 - Oct 26, 2025]
- Breakdown by view type
- HTML page views: 2160
- PDF downloads: 873