Research Article Open Access
Synchronous Liver Resection with Cytoreductive Surgery for the Treatment of Liver and Peritoneal Metastases from Colon Cancer: Results from an Australian Centre
Alzahrani N1,3*, Ung L1, Valle SJ1,2, Ferguson J1, Liauw W1,2 and Morris DL11Department of Surgery and St George Hospital Department of Surgical Oncology, University of New South Wales, Level 3, Pitney Clinical Sciences Building, Kogarah NSW 2217, Australia
2Cancer Care Centre, St George Hospital, 1 Short Street, Kogarah NSW 2217, Australia
3College Of Medicine, Imam Muhammed Ibn Saud Islamic University, Saudi Arabia
- *Corresponding Author:
- Dr. Nayef Alzahrani
St George Hospital Department of Surgical Oncology
Level 3, Pitney Clinical Sciences Building
Kogarah, NSW 2217, Australia
Tel: 61 432 639 166
Fax: 61 2 9113 3997
E-mail: nayefalhariri@hotmail.com
Received date: February 23, 2015; Accepted date: March 14, 2015; Published date: March 22, 2015
Citation: Alzahrani N, Ung L, Valle SJ, Ferguson J, Liauw W, et al. (2015) Synchronous Liver Resection with Cytoreductive Surgery for the Treatment of Liver and Peritoneal Metastases from Colon Cancer: Results from an Australian Centre. J Gastrointest Dig Syst 5:264. doi:10.4172/2161-069X.1000264
Copyright: © 2015 Alzahrani N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Treatment of peritoneal metastases (PM) and liver metastases (LM) from colon cancer remains controversial. LM has been viewed as exclusion criterion for cytoreductive surgery (CRS) on the basis that such spread represents systemic disease. CRS and intra-peritoneal chemotherapy (IPC) has gained increasing recognition as a treatment modality for selected patients with colon cancer and PM. This study analyses results of CRS and IPC for colon cancer and synchronous resection for treatment of LM and PM.
Methods: Seventy-eight patients with PM/LM colon cancer were analysed. Forty-two patients with PM were treated for disease limited to the peritoneum (A), and 36 patients received treatment for both PM and LM (B). Overall survival (OS), disease-free survival (DFS), morbidity, mortality, and recurrence were compared.
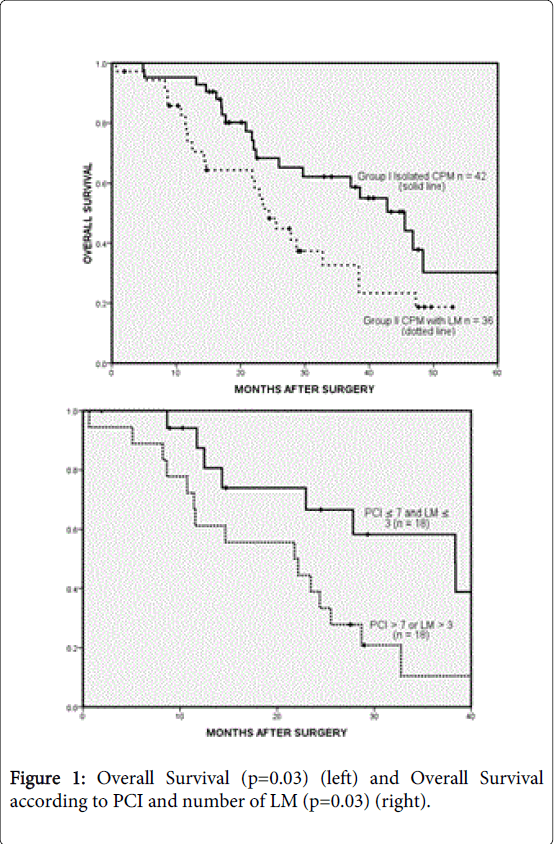
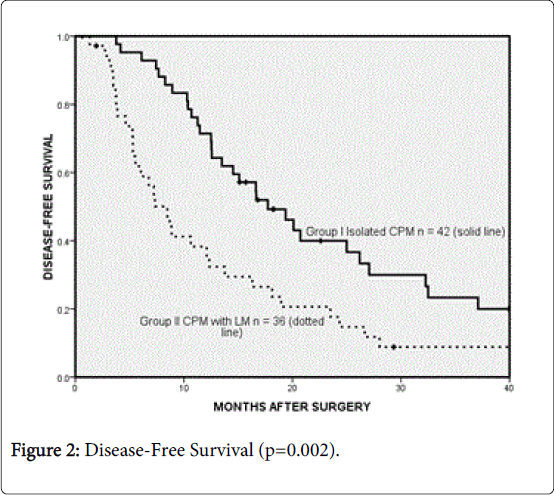
Results: Median overall (OS) and disease-free survival (DFS) was 32.8 and 13.5 months. The median OS for A and B were 45.5 and 24.4 months respectively. Within B patients, 18 had a PCI>7 and >3 LM and median survival of 21.8 months compared to 18 patients with PCI ≤ 7 and LM ≤ 3 with median survival of 38.4 months. Median DFS for A and B were 17.7 and 8.5 months respectively. Twenty-seven in total experienced major complications following surgery. Sixty-one patients recurred. Of A, 71.4% recurred compared to B at 86.1%.
Conclusion: While our study is limited, it has demonstrated encouraging evidence that long-term survival outcomes can be achieved in this small but significant number of patients treated by CRS/IPC and additional synchronous liver resection with no significant increase in morbidity when compared to CRS/IPC alone.
Abstract
Background: Treatment of peritoneal metastases (PM) and liver metastases (LM) from colon cancer remains controversial. LM has been viewed as exclusion criterion for cytoreductive surgery (CRS) on the basis that such spread represents systemic disease. CRS and intra-peritoneal chemotherapy (IPC) has gained increasing recognition as a treatment modality for selected patients with colon cancer and PM. This study analyses results of CRS and IPC for colon cancer and synchronous resection for treatment of LM and PM.
Methods: Seventy-eight patients with PM/LM colon cancer were analysed. Forty-two patients with PM were treated for disease limited to the peritoneum (A), and 36 patients received treatment for both PM and LM (B). Overall survival (OS), disease-free survival (DFS), morbidity, mortality, and recurrence were compared.
Results: Median overall (OS) and disease-free survival (DFS) was 32.8 and 13.5 months. The median OS for A and B were 45.5 and 24.4 months respectively. Within B patients, 18 had a PCI>7 and >3 LM and median survival of 21.8 months compared to 18 patients with PCI ≤ 7 and LM ≤ 3 with median survival of 38.4 months. Median DFS for A and B were 17.7 and 8.5 months respectively. Twenty-seven in total experienced major complications following surgery. Sixty-one patients recurred. Of A, 71.4% recurred compared to B at 86.1%.
Conclusion: While our study is limited, it has demonstrated encouraging evidence that long-term survival outcomes can be achieved in this small but significant number of patients treated by CRS/IPC and additional synchronous liver resection with no significant increase in morbidity when compared to CRS/IPC alone.
Keywords
Cytoreductive surgery; Peritoneal metastases; Colon cancer; Liver metastases; PCI; Heated intraperitoneal chemotherapy
Introduction
Annually, colorectal cancer (CRC) accounts for approximately 1.2 million diagnoses of cancer and 600 000 deaths worldwide [1]. Studies of its natural history have demonstrated that the development of liver (LM) and peritoneal metastases (PM) are the most common causes of death in patients with advanced disease, thought to occur in 50% [2] and 25% [3] of all patients afflicted with this often fatal condition. The progression from local to regional and widely disseminated disease is a feared complication of colorectal cancer, one which has been shown to result in death often within a year of diagnosis when treated with supportive therapy alone, [2,4] and modest survival even with contemporary chemotherapy.
Cytoreductive surgery (CRS) coupled with intra-peritoneal chemotherapy has gained increasing recognition as a potential treatment modality for carefully selected patients with CRC peritoneal metastases. A significant survival advantage using this strategy was demonstrated by a Dutch randomised controlled trial by Verwaal and colleagues published in 2003, who found a median survival of 22.3 months in patients receiving CRS and heated intra-peritoneal chemotherapy with or without systemic chemotherapy, compared to 12.6 months in patients treated with systemic chemotherapy with or without palliative surgery [5]. Perhaps even more important than median survival is the chance of long-term survival, which can occur in approximately 50% of patients with low volume peritoneal disease.
Traditionally however, the presence of additional liver metastases has been viewed as an exclusion criterion for CRS on the basis that such spread represents systemic, rather than isolated loco-regional disease. However, as long-term survival has been observed in patients who undergo liver resection for metastatic CRC [6], a relatively recent development in the management of patients who present with limited liver and peritoneal metastases has been to offer synchronous liver resection with CRS. In this study, we critically evaluate the survival of patients offered this treatment from a high volume Australian centre, to determine whether this surgical strategy may be used to achieve long-term survival in these patients.
Methods
Patient selection
A total of 78 patients with metastatic colon cancer, managed at St. George Hospital Australia from April 2003 to June 2014, were drawn from a prospective on-site database of almost 800 patients, with 178 colorectal patients; and analysed. In this time, 36 and 42 patients with colon cancer were treated with CRS, with and without synchronous liver resection respectively. A multidisciplinary diagnostic work-up by participating surgeons, medical oncologists, radiologists and clinical nurse consultants assessed the eligibility of all patients based on a histopathological and image-based diagnosis of PM ± LM and the presence of resectable disease. Criteria for selection and consideration of CRS/HIPEC in colon cancer patients includes a PCI<15 ( PCI<10 in patients with LM, no evidence of N3 lymph node involvement, no progressive disease after pre-operative chemotherapy, no severe co-morbidities, ECOG<2, LM<4, no extra-abdominal disease). Patients with disease of appendiceal or rectal origin, or with benign liver lesions, were excluded from analysis.
Patients from the PM group with additional LM treated by CRS were compared with patients treated by CRS for isolated PM. Patients were analysed manually using the on-site database of a group of almost 800 cases, and the decision to include patients with isolated PM was based on: period of surgery (2003 onwards), gender, age, PCI<10 in patients with LM, completeness of cytoreduction score, tumour grade, lymph node status and use of pre- and post-operative chemotherapy, in an attempt to homogenise baseline characteristics.
Treatment
All patients underwent CRS according to a standardised protocol based on the Sugarbaker technique. Following a midline laparotomy, the amount of disease located within the peritoneal cavity was quantified using the Peritoneal Cancer Index (PCI) which provides a numerical indication of abdominal tumour burden according to the distribution and size of metastatic deposits [7]. Within thirteen specified regions (nine abdominopelvic and four quadrants of the small bowel mesentery), a score out of 3 was given to indicate the presence and size of disease in that particular area. A lesion score of 0 indicated absence of disease; 1 indicated deposits <0.5 mm in diameter; 2 indicated nodules between 0.5 mm and 5 cm and 3 indicated nodules >5 cm or tumour confluence. A maximum score of 39 was therefore possible. CRS as described by Sugarbaker consists of the macroscopic removal of all tumour and can be achieved by a combination of six peritonectomy procedures and associated multi-visceral resection, including: anterior parietal, right and left sub-phrenic, pelvic, greater omentectomy with or without splenectomy and lesser omentectomy with or without cholecystectomy [8,9].
Intra-operative ultrasound was performed in all patients to detect possible liver metastases. Our criteria for CRS intra-operatively PCI upper limit of 15 for PM or PCI<10 and a maximum of four liver lesions for combined PM and LM. Liver resection was performed using ultrasonic dissection (Sumisonic ME2210, Simitomo Bakelite Co or Selector Spembly). Following completion of CRS, patients received a combination of either intra-operative heated intra-peritoneal chemotherapy (HIPEC); consisting of an infusion of mitomycin-C (12.5 mg/m2) in 3 L of 1.5% dextrose peritoneal dialysis fluid heated to 42°C and/or early post-operative intra-peritoneal chemotherapy (EPIC) consisting of up to 5 days of 5-fluorouracil (650-800 mg/m2) in 1 L of 1.5% dextrose peritoneal dialysis fluid, however, EPIC was withheld in patients with post-operative complications. The French Bidirectional Protocol was adopted in February 2010 and consisted of folinic acid 50 mg intravenously 1-hour prior to procedure and 5 FU 400 mg/m2 intravenously in addition to the intra-operative heated intra-peritoneal chemotherapy (HIPEC) of an infusion of oxaliplatin 350 mg/m2 in 500 mL of 5% dextrose heated to 42°C; for 30 minutes. EPIC was not longer performed for colon cancer under this protocol. A completeness of cytoreduction (CC) score was given to each patient to reflect the amount of residual disease: CC-0 indicates all macroscopic tumours have been removed; CC-1 indicates that no deposit >2.5 mm remained and CC-2 indicates residual tumour between 2.5 mm and 2.5 cm [10].
Data collection and statistical analysis
All cases included for retrospective analysis were retrieved from a prospective database containing relevant clinicopathologic variables as documented in Table 1. Post-operative mortality was defined as death within 30 days of surgery, and morbidity was graded using the National Cancer Institute’s Common Toxicity Criteria. A score of 3 or 4 was considered major morbidity and defined as complications that necessitated return to theatre or radiological intervention [11].
| GroupA: Isolated Colonic Peritoneal Metastases | GroupB: Colonic Peritoneal and Liver Metastases | Pvalue | |
| Total | 42 | 36 | — |
| Follow-up(median) | 21.5 | 21.9 | — |
| Age(years) | |||
| Mean(s.d.) | 59.4(14.3) | 60.3(12.6) | 0.54 |
| Sex | |||
| Male | 19(44.2) | 15(41.6) | 0.75 |
| Female | 23(54.8) | 21(58.4) | |
| PCI | |||
| Mean(s.d.) | 12.7(9.9) | 7.0(5.1) | <0.001 |
| Completenessofcytoreduction | |||
| CC0 | 39(92.8) | 35(97.2) | 0.58 |
| CC1 | 2(4.8) | 1(2.8) | |
| CC2 | 1(2.4) | 0 | |
| HIPEC | |||
| Yes | 36(85.7) | 18(50) | 0.001 |
| No | 6(14.3) | 18(50) | |
| TumourGrade | |||
| Well | 0 | 2(5.5) | 0.11 |
| Moderate | 27(64.3) | 27(75) | |
| Poor | 15(35.7) | 7(19.5) | |
| MucinousHistology | |||
| Yes | 19(45.2) | 8(22.2) | 0.03 |
| No | 23(54.8) | 28(77.8) | |
| LymphNodeStatus | |||
| Positive | 29(69) | 16(44.4) | 0.76 |
| Negative | 13(31) | 20(55.6) | |
| Pre-OperativeChemotherapy | |||
| Yes | 17(40.9) | 33(91.7) | <0.001 |
| No | 25(59.1) | 3(8.3) | |
| Post-OperativeChemotherapy | |||
| Yes | 34(81) | 33(91.7) | 0.18 |
| No | 8(19) | 3(8.3) | |
| DurationofProcedure(hours) | |||
| Mean(s.d.) | 8.0(3.1) | 6.1(2.3) | 0.23 |
| DurationofICUStay(days) | |||
| Mean(s.d.) | 3.0(3.1) | 2.4(2.7) | 0.28 |
| DurationofHospitalStay(days) | |||
| Mean | 23.7(13.9) | 21.8(11.6) | 0.66 |
| BloodTransfusion(units) | |||
| Mean(s.d.) | 4.0(4.4) | 2.4(2.5) | 0.09 |
| MajorComplications | |||
| Yes | 13(31) | 14(38.9) | 0.46 |
| No | 29(69) | 22(61.1) | |
| Survival | |||
| Overall,median(months) | 45.5 | 24.4 | 0.03 |
| Disease-free,median(months) | 17.7 | 8.5 | 0.002 |
| 1-yearoverall(%) | 95 | 74 | — |
| 3-yearoverall(%) | 62 | 33 | — |
| 5-yearoverall(%) | 31 | 18 | — |
| Recurrence | |||
| Yes | 30(71.4) | 31(86.1) | 0.12 |
| No | 12(28.6) | 5(13.9) | |
Table 1: Baseline comparison of characteristics between group A and B.
All statistical analysis was completed using SPSS® (Windows Version 18). In the comparison of patient characteristics, means were obtained using either independent samples t-test for normally distributed data or Mann-Whitney U test for skewed data. For categorical data, Pearson’s chi-squared test was used. Follow-up was determined by the time between surgery and date of death or censor date (August 2014). The end-points of this study included overall survival (OS), the time between operation and death (or censor date if still alive), disease-free survival (DFS), the time between operation and relapse, and patterns of recurrence. To compare survival between patients treated for isolated PM and PM with LM, Kaplan-Meier curves were constructed and differences between strata computed by the log-rank test. Univariate analyses using Kaplan-Meier curves and the log-rank test were also conducted on patients with PM and LM to elucidate prognostic factors associated with survival. Patients in this group were separated into two groups: extensive disease (PCI>7 and LM>3) and minimal to moderate disease (PCI ≤ 7 and LM ≤ 3) for this purpose. No patient was lost from follow-up. P ≤ 0.05 was considered statistically significant.
Results
Patient characteristics
From 2003 to 2014, seventy-eight (78) patients at St. George Hospital, Australia; were treated for peritoneal metastases, including a group with liver involvement, of colonic origin. Their baseline characteristics are shown in Table 1. In total, 42 (53.8%) patients with isolated peritoneal disease were treated for disease limited to the peritoneum (Group A), while 36 (46.2%) received treatment for both peritoneal and liver metastases (Group B).
Overall, there were no significant differences observed in the following baseline characteristics: age (mean 59.4 versus 60.3 years, p=0.54), sex (p=0.75), completeness of cytoreduction (p=0.58), tumour grade (p=0.11), lymph node metastases (p=0.76), post-operative chemotherapy (p=0.18). There were statistically significant differences in the PCI (mean 12.7 versus 7.0, p<0.001), use of HIPEC (p=0.001), mucinous histology (p=0.03) and the use of pre-operative chemotherapy (p<0.001). The difference in the number of patients receiving both HIPEC and EPIC between both groups was of borderline significance (p=0.06).
Peri-operative outcomes
One (1.3%) patient died within thirty days of the procedure. This patient died from acute respiratory distress syndrome. Operative data showed that there were no differences observed in the duration of the procedure (mean 8.0 hours versus 6.1, p=0.23), duration of ICU stay (mean 3.0 days vs. 2.4, p=0.28), total hospital stay (mean 23.7 days versus 21.8 days, p=0.66) and amount of blood transfusion units required (mean 4.0 units versus 2.4, p=0.09). A total of 27 (n=27, 34.6%) experienced major complications following surgery, but there was no difference between both groups (p=0.46).
Complications included infection (n=22, 28.2%), post-operative haemorrhage (n=4, 5.1%), cardiotoxicity (n=3, 3.8%), pneumonia (n=3, 3.8%), pleural effusion (n=19, 24.4%), pneumothoraces (n=7, 9.0%), pulmonary embolism (n=4, 5.1%), fistula formation (n=6, 7.7%), ileus (n=4, 5.1%), pancreatic leakage (n=4, 5.1%), small bowel obstruction (n=1, 1.3%) and leak of intra-peritoneal chemotherapy (n=4, 5.1%). A total of 7 patients (9%) were returned to the operating theatre for surgical resolution of their post-operative complication.
Survival and recurrence
The overall median follow-up was 21.8 months (range, 1-86). For patients with isolated peritoneal metastases (A), follow-up was 21.5 months compared to 21.9 months for patients with both peritoneal and liver metastases (B). The median overall survival (OS) and disease-free survival (DFS) were 32.8 months (95% CI 19.0-46.5) and 13.5 months (95% CI 10.3-16.7). The median OS for groups A and B were 45.5 months and 24.4 months respectively (p=0.03, Figure 1).
The median DFS were 17.7 months and 8.5 months respectively (p=0.002, Figure 2). The 1-year, 3-year and 5-year survival was 95%, 62% and 31% for group A, compared to 74%, 33% and 18% for group B. Within group B patients, 18 patients had a PCI>7 and greater than 3 LM, and had a median survival of 21.8 (95% CI 6.2-37.3) compared to the remaining 18 patients with PCI ≤ 7 and LM ≤ 3 who achieved survival of 38.4 months (95% CI 23.2-53.5, p=0.03, Figure 1).
It is important to note that the proportion of mucinous patients is higher in the LM group (group B) and this, especially in a larger series, may have translated in an overall survival difference. On univariate analysis, post-operative chemotherapy (p<0.001) and lower PCI (p=0.01) were factors associated with an improved survival (Table 2).
| Factor | Number(n) | Mediansurvival(months) | UnivariateP |
| Age | |||
| >60 | 21(58.3) | 28.7 | 0.13 |
| ≤60 | 15(41.7) | 21.8 | |
| Sex | |||
| Male | 15(41.7) | 25.5 | 0.81 |
| Female | 21(58.3) | 23.5 | |
| Tumourgrade | |||
| Well | 2(5.6) | 10.7 | 0.26 |
| Moderate | 27(75) | 27.8 | |
| Poor | 7(19.4) | 21.8 | |
| Mucinoushistology | |||
| Mucinous | 8(22.2) | 23.0 | 0.20 |
| Non-mucinous | 28(78.8) | 27.8 | |
| Lymphnodemetastases | |||
| Yes | 26(72.2) | 23.0 | 0.12 |
| No | 10(27.8) | 32.8 | |
| Pre-operativechemotherapy | |||
| Yes | 33(91.7) | 23.5 | 0.10 |
| No | 3(8.3) | 38.4 | |
| Post-operativechemotherapy | |||
| Yes | 33(91.7) | 25.5 | <0.001 |
| No | 3(8.3) | 8.6 | |
| PCI | |||
| 1-5 | 16 | 47.2 | 0.01 |
| 6-10 | 13 | 23.5 | |
| >10 | 7 | 21.8 | |
| NumberofLiverLesions | |||
| ≥3 | 11 | 11.6 | 0.15 |
| <3 | 25 | 27.8 | |
| HIPEC | |||
| Yes | 18(50) | 32.8 | 0.27 |
| No | 18(50) | 22.2 | |
| EPIC | |||
| Yes | 20(55.6) | 23.0 | 0.15 |
| No | 16(44.4) | 38.4 | |
| HIPEC+EPIC | |||
| Yes | 6(16.7) | 23.0 | 0.34 |
| No | 30(83.3) | 24.4 | |
| ExtentofDisease | |||
| PCI>7andLM>3 | 18(50) | 21.8 | 0.03 |
| PCI≤7andLM≤3 | 18(50) | 38.4 | |
Table 2: Univariate analysis of clinicopathologic factors influencing survival for patients treated for colorectal peritoneal and liver metastases.
In the 78 patients, 61 patients experienced recurrence (78.2%). Of group A patients, 30 of 42 (71.4%) patients recurred compared to 31 of 36 of patients from group B (86.1%). There was no statistically significant difference between groups and their association with recurrence ( (2, n=78)=2.5, p=0.12).
Discussion
In the last decade, cytoreductive surgery and intra-peritoneal chemotherapy (CRS/IPC) has become recognised as an appropriate management strategy for a subset of patients with metastatic colorectal cancer with peritoneal disease. While natural history studies of patients with disseminated peritoneal metastases of colorectal origin have reported a median survival range of 3.1 - 7 months when treated by palliative means [4,12], large multicentre studies have shown that CRS/IPC may improve this range to 30 - 32.4 months [13,14]. In a recent update of our results from this Australian tertiary referral centre, we showed that the median survival in 109 patients treated by CRS/IPC for colorectal peritoneal metastases was 37.1 months [15].
The surgical rationale behind CRS/IPC appears to lie in the observation that peritoneal metastases may not represent widespread lymphohaematogenous spread of the primary tumour, but rather a loco-regional entity for which surgical resection may be warranted. However, a recent development in the management of peritoneal metastases by CRS/IPC has been the expansion of this subset of patients to include patients with limited liver involvement, for which additional synchronous liver resection may be performed in conjunction with CRS/IPC. While no phase III trial has ever evaluated liver metastasectomy for colorectal metastases against controls, this form of surgery is nevertheless regarded as the standard of care in many centres globally. The aim of this retrospective analysis was to compare the results of CRS/IPC with and without synchronous liver resection in this Australian centre with a view to determining whether the selection criteria of CRS/IPC may be extended to patients with limited liver disease.
This study demonstrated that promising survival outcomes may be achieved in carefully selected patients who are treated by CRS/IPC with additional synchronous liver resection. In comparing patients with similar baseline characteristics, most notably PCI, we showed that although there was a statistically significant difference in both overall and disease-free survival between patients with and without liver metastases (median OS 45.5 months versus 24.4 months, p=0.03, Figure 1 and median DFS 17.7 months versus 8.5 months, p=0.002, Figure 2), the five-year survival rate of patients undergoing synchronous liver resection was 18%. While our study is limited by its observational, retrospective nature, the selection biases inherent in single-institution studies and our small sample size; our results nevertheless may suggest that long-term survival is achievable in a small but significant number of patients who undergo CRS/IPC with additional synchronous liver resection for liver metastases. Elias et al. prospectively studied 24 patients who had CRS for colon cancer with liver metastases and/or moderate peritoneal carcinomatosis. The five-year survival rate of all patients was 26.5% with a median overall survival of 30-36 months.
Our recorded median survival of 24.4 months should be recognised in the context of current survival outcomes in patients with liver and peritoneal disease arising from colorectal cancer when treated by the current standard of palliative chemotherapy and surgery to relieve symptoms. In the last ten years, great strides have been made to this end, with the publication of several high-profile randomised controlled trials which have evaluated the efficacy of several modern chemotherapy regimens in the treatment of metastatic colorectal cancer. Currently, oxaliplatin- and irinotecan-based chemotherapies have improved median survival to 20.8-23.1 months respectively [16,17]. The recent addition of targeted therapies to these regimens, including bevacizumab and cetuximab has further improved survival up to 28 months [18,19].
However, it is questionable whether these survival outcomes may be achieved in patients with concomitant liver and peritoneal metastases. First, patients with isolated peritoneal metastases of colorectal origin are unlikely to have been entered into these aforementioned trials due to the difficulties encountered in accurately detecting and quantifying disease according to the Response Evaluation Criteria in Solid Tumours (RECIST) criteria [20]. Second, recent efforts to stratify response rates according to the site of metastatic spread has shown that patients with colorectal peritoneal metastases may achieve inferior outcomes possibly due to the presence of a plasma-peritoneum barrier which may inhibit exposure of tumorous nodules to the administered chemotherapy. This was clearly shown by a pooled subgroup analysis by Franko et al. who analysed 2095 patients enrolled in two high profile chemotherapy trials for metastatic colorectal cancer, NCCTG-N9741 and NCCTG-N9841 [21]. The authors demonstrated that the median overall and progression-free survival was significantly shorter in patients with peritoneal metastases compared to patients with non-peritoneal metastases (12.7 versus 17.6 months, p<0.001 and 5.8 versus 7.2 months, p=0.001 respectively) [21]. Therefore in patients with both liver and peritoneal disease, a more aggressive surgical approach may be warranted to augment systemic chemotherapy in order to achieve long-term survival.
While our results cannot be extrapolated to other centres given important differences in the surgical expertise of different operating teams, selection criteria and the type and mode of intra-peritoneal chemotherapy administered, it is nonetheless important to note that the results of this study are consistent with the published literature. A systematic review of all studies identifying patients undergoing additional liver surgery as a subset of patients undergoing CRS/IPC is presented in Table 3, demonstrating a median overall and disease-free survival in the order of 24.4-36 months and 8.5-24 months respectively. The median five-year survival documented was 26.2% (18-31%).
| Authors | n | IPC used | Mean PCI | Mean No. of Liver Lesions | Median follow-up(months) | Median over all survival (months) | Median disease-frees urvival (months) | Survival rates (%) | Morbidity n(%)* | Mortality n(%)* |
| Alzahranietal. (current study-unpublished data) | 78 | HIPEC: Oxaliplatin 350mg/m2 500mL of 5% dextrose,42°C,30 minutes. Mitomycin (12.5mg/m2),42ºC, 3L,30-90 minutes.EPIC:1L650-800 mg/m25-FUin1L1-5 days (pre02/10). | 12.7 | 2.7 | 21.8 | 32.8 | 13.5 | A:1,3,5 year: 95,62 and 31 B:1,3,5 year: 74,33 and 18 | 27(34.6) | 1(1.3) |
| Ungetal. | 36 | HIPEC: Mitomycin (12.5mg/m2)in 42ºC 3L peritoneal dialysis fluid,30-90 minutes. EPIC:1L650-800 mg/m2 5-FUin1L peritoneal dialysis fluid,1-5days | 7.0 | 2.3 | 21.8 | 24.4 | 8.5 | 1,3,5 year: 74, 33 and 18 | 14(39) | 1(3) |
| Maggiori etal. [22] | 37 | — | 11 (median) | 2 (median) | 36 (mean) | 32 | 9 | 3 and 5 year:40 and 26 | 19(51) | 3(8) |
| Chua etal. [23]** | 16(55 total) | AsUngetal. | 8.0 | — | 19 | — | — | 2year:65% | 17(31)* | 0 |
| Kianmanesh etal.[24]*** | 16(43 total) | HIPEC:6 Lmitomycin 120 mg and 6L 200mg/m2 for 30-90minutes | — | — | — | 36 | — | — | 17(39)* | 1(2)* |
| Elias etal.[25] | 24 | Various | 8.6 | 4.4 | 27.8 (mean) | 30-36 | 18-24 | 2,3,5 year:61.3,41.5 and 26.5 | 14(58) | 1(4) |
| MEDIAN (RANGE) [26] | 8.6(7-12.7) | 2.5(2-4.4) | 21.8(19-36) | 24.4-36 | 8.5-24 | 5-year: 26.25 (18-31) | 35(31-58) | 1(0-8) | ||
Table 3: Systematic Review of Retrospective Studies of Patients Undergoing Liver Resection with CRS/IPC. *Presented as percentage of all included patients** Of 16 patients with liver metastases, 10 patients had synchronous liver resection, 2 had cryotherapy and 4 had both. ***The timing of liver metastectomy in this study varied – between pre-operative, intra- and post-operative. “—‘’ denotes “unstated” or not applicable.
A reasonable question to posit, however, is how survival in this carefully selected group may be further improved to more closely resemble patients with isolated peritoneal metastases. In our centre, patients were generally selected on the basis of relatively low disease burden or PCI as well as having 3 or fewer liver lesions. In this study, we compared this group by patients with “higher” disease volume (PCI>7 and >3 LM) and “lower” disease volume (PCI ≤ 7 and LM ≤ 3). Patients with higher disease volume had a median overall survival of 21.8 months compared to patients with a lower burden of disease who recorded a median survival of 38.4 months, approaching that of non-LM patients (p=0.03). It would therefore appear that the greatest benefit from this procedure may be experienced by patients in this latter group and may come into consideration in the revision of our surgical criteria.
This study provides encouraging evidence that patients with peritoneal and liver metastases of colon origin, particularly those with limited disease burden may achieve long term survival through a radical surgical approach consisting of CRS/IPC and synchronous liver resection. By refining the surgical criteria and selection process, this strategy may be used to augment the use of systemic chemotherapy in order to optimise patient outcomes.
Acknowledgements
Database manager, Jing Zhao, for providing statistics and data.
References
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, et al. (2011) Global cancer statistics. CA Cancer J Clin 61: 69-90.
- Stangl R, Altendorf-Hofmann A, Charnley RM, Scheele J (1994) Factors influencing the natural history of colorectal liver metastases. Lancet 343: 1405-1410.
- Koppe MJ, Boerman OC, Oyen WJ, Bleichrodt RP (2006) Peritoneal carcinomatosis of colorectal origin: incidence and current treatment strategies. Ann Surg 243: 212-222.
- Jayne DG, Fook S, Loi C, Seow-Choen F (2002) Peritoneal carcinomatosis from colorectal cancer. Br J Surg 89: 1545-1550.
- Verwaal VJ, van Ruth S, de Bree E, van Sloothen GW, van Tinteren H, et al. (2003) Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 21: 3737-3743.
- Simmonds PC, Primrose JN, Colquitt JL, Garden OJ, Poston GJ, et al. (2006) Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies. Br J Cancer 94: 982-999.
- Sugarbaker PH (2005) Surgical management of carcinomatosis from colorectal cancer. Clin Colon Rectal Surg 18: 190-203.
- Sugarbaker PH (1998) Intraperitoneal chemotherapy and cytoreductive surgery for the prevention and treatment of peritoneal carcinomatosis and sarcomatosis. Semin Surg Oncol 14: 254-261.
- Chua TC, Pelz JO, Morris DL (2012) Surgery for colorectal peritoneal carcinomatosis. Scand J Gastroenterol 47: 277-285.
- Glehen O, Gilly FN, Boutitie F, Bereder JM, Quenet F, et al. (2010) Toward curative treatment of peritoneal carcinomatosis from nonovarian origin by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy: a multi-institutional study of 1,290 patients. Cancer 116: 5608-5618.
- (2014) National Cancer Institute. National Cancer Institute Common Toxicity Criteria Version 2. 1999. Accessed.
- Sadeghi B, Arvieux C, Glehen O, Beaujard AC, Rivoire M, et al. (2000) Peritoneal carcinomatosis from non-gynecologic malignancies: results of the EVOCAPE 1 multicentric prospective study. Cancer 88: 358-363.
- Glehen O, Cotte E, Schreiber V, SayagaeBeaujard A, Vignal J, et al. (2004) Intraperitoneal chemohyperthermia and attempted cytoreductive surgery in patients with peritoneal carcinomatosis of colorectal origin. British journal of surgery 91: 747-754.
- Glehen O, Gilly FN, Arvieux C, Cotte E, Boutitie F, et al. (2004) Peritoneal carcinomatosis from gastric cancer: a multi-institutional study of 159 patients treated by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy. Annals of surgical oncology 17: 2370-2377.
- Ung L, Chua T, Morris D (2013) Peritoneal metastases of lower gastrointestinal tract origin: a comparative study of patient outcomes following cytoreduction and intraperitoneal chemotherapy. Journal of Cancer Research and Clinical Oncology 2013: 1-10.
- Díaz-Rubio E, Tabernero J, Gómez-España A, Massutí B, Sastre J, et al. (2007) Phase III study of capecitabine plus oxaliplatin compared with continuous-infusion fluorouracil plus oxaliplatin as first-line therapy in metastatic colorectal cancer: final report of the Spanish Cooperative Group for the Treatment of Digestive Tumors Trial. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 25: 4224-4230.
- Fuchs CS, Marshall J, Mitchell E, Wierzbicki R, Ganju V, et al. (2007) Randomized, controlled trial of irinotecan plus infusional, bolus, or oral fluoropyrimidines in first-line treatment of metastatic colorectal cancer: results from the BICC-C Study. J Clin Oncol 25: 4779-4786.
- Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, et al. (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350: 2335-2342.
- Fuchs CS, Marshall J, Barrueco J (2008) Randomized, controlled trial of irinotecan plus infusional, bolus, or oral fluoropyrimidines in first-line treatment of metastatic colorectal cancer: updated results from the BICC-C study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 26:689-690.
- Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, et al. (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. Journal of the National Cancer Institute 92: 205-216.
- Franko J, Shi Q, Goldman CD, Pockaj BA, Nelson GD, et al. (2012) Treatment of colorectal peritoneal carcinomatosis with systemic chemotherapy: a pooled analysis of north central cancer treatment group phase III trials N9741 and N9841. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 30: 263-267.
- Maggiori L, Goéré D, Viana B, Tzanis D, Dumont F, et al. (2013) Should patients with peritoneal carcinomatosis of colorectal origin with synchronous liver metastases be treated with a curative intent? A case-control study. Ann Surg 258: 116-121.
- Chua T, Yan T, Zhao J, Morris D (2009) Peritoneal carcinomatosis and liver metastases from colorectal cancer treated with cytoreductive surgery perioperative intraperitoneal chemotherapy and liver resection. European Journal of Surgical Oncology (EJSO) 35: 1299-1305.
- Kianmanesh R, Scaringi S, Sabate JM, Castel B, Pons-Kerjean N, et al. (2007) Iterative cytoreductive surgery associated with hyperthermic intraperitoneal chemotherapy for treatment of peritoneal carcinomatosis of colorectal origin with or without liver metastases. Ann Surg 245: 597-603.
- Elias D, Benizri E, Pocard M, Ducreux M, Boige V, et al. (2006) Treatment of synchronous peritoneal carcinomatosis and liver metastases from colorectal cancer. European Journal of Surgical Oncology (EJSO) 32: 632-636.
- Klaver YL, Simkens LH, Lemmens VE, Koopman M, Teerenstra S, et al. (2012) Outcomes of colorectal cancer patients with peritoneal carcinomatosis treated with chemotherapy with and without targeted therapy. European Journal of Surgical Oncology (EJSO) 38: 617-623.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14533
- [From(publication date):
April-2015 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 10141
- PDF downloads : 4392